Medical Oncology
Adjuvant therapy is crucial when managing colon cancer, reducing recurrence risk and improving overall survival rates. Interventional strategies are tailored to the disease stage and patient risk factors. Close monitoring and treatment adherence are essential to optimize outcomes and minimize potential side effects.
Adjuvant Therapy
Adjuvant chemotherapy has no role in stage I colon cancer management. Patients with low-risk stage II colon cancer can opt for adjuvant therapy-free surveillance, individualized medical oncology discussions, or clinical trial enrollment. Current guidelines from the American Society of Clinical Oncology (ASCO), European Society for Medical Oncology (ESMO), and NCCN strongly recommend adjuvant therapy for selected stage II cancers with high-risk features, ie, those with proficient DNA mismatch repair or microsatellite stability (pMMR/MSI-S) disease, and all stage III (node-positive) tumors.
For colon cancer adjuvant therapy, 3-year disease-free survival (DFS) is an acceptable surrogate marker for 5-year overall survival recognized by the FDA based on data from the Adjuvant Colon Cancer End Points (ACCENT) study group. Guidelines advocate delivering adjuvant chemotherapy within 6 to 8 weeks of surgical resection pending the patient’s recovery.
A meta-analysis revealed that extending the time to adjuvant chemotherapy beyond 4 weeks was linked to a notable decrease in both overall survival (hazard ratio 1.14; 95% confidence interval 1.10-1.17) and DFS (hazard ratio 1.14; 95% confidence interval 1.10-1.18). In terms of chemotherapy regimens, an oxaliplatin-based combination is preferred over monotherapy, whether it be 5-fluorouracil/leucovorin (5-FU/LV), as demonstrated in the Multicenter International Study of Oxaliplatin/5-Fluorouracil/Leucovorin in the Adjuvant Treatment of Colon Cancer (MOSAIC) and the National Surgical Adjuvant Breast and Bowel Project (NSABP) C-07 trials, or capecitabine, as shown in the Xeloda in Adjuvant Colon Cancer Therapy (XELOXA) trial.
The standard duration of adjuvant therapy remains 6 months, although ongoing investigation in the International Duration Evaluation of Adjuvant Chemotherapy (IDEA) trial is exploring the potential noninferiority of a 3-month regimen for low-risk patients or those experiencing oxaliplatin’s dose-limiting neurotoxicity. Administering a full weight-based chemotherapy dosing is recommended, especially in cases where the intention is curative.[34][35][36]
Adjuvant fluorouracil-based chemotherapy became the standard treatment for stage III colon cancer in the early 1990s following the groundbreaking NSABP C-01 trial. This trial was the first randomized clinical trial to demonstrate a significant improvement in DFS and overall survival. Subsequent evidence from the NSABP C-03 trial showed that 6 months of 5-FU/LV therapy resulted in even better DFS and overall survival at 3 years compared to the NSABP C-01 regimen of lomustine, vincristine, and 5-FU. For over a decade, 5-FU/LV remained the standard adjuvant therapy. However, the landscape shifted when combinations containing oxaliplatin, irinotecan, and capecitabine (an oral fluorouracil prodrug) were introduced for the treatment of advanced colorectal cancer.
Oxaliplatin was approved as part of adjuvant treatment for stage III colon cancer after the 2004 MOSAIC trial. Investigators randomly assigned patients who had undergone curative colon resection for stage II (40%) or III (60%) to receive 5-FU/LV alone (leucovorin 200 mg/m as a 2-hour infusion, followed by a 5-FU bolus 400 mg/m, and then a 22-hour infusion of 5-FU 600 mg/m, every 2 weeks) or with oxaliplatin (5-FU/LV with 85 mg/m day 1 every 14 days, a regimen termed Fluorouracil, Leucovorin, and Oxaliplatin regimen version 4 or “FOLFOX4”) for 6 months.
FOLFOX4 therapy significantly improved 5-year DFS rates to 73.3% compared to 67.4% in the 5-FU/LV group (hazard ratio = 0.80; 95% confidence interval, 0.68 to 0.93; P = .003) and 6-year overall survival rates were 78.5% and 76.0% in the FOLFOX4 and 5-FU/LV groups, respectively (hazard ratio = 0.84; 95% confidence interval, 0.71 to 1.00; P = .046). Stratified, 6-year overall survival rates for patients with stage III disease were 72.9% and 68.7%, respectively (hazard ratio = 0.80; 95% confidence interval, 0.65 to 0.97; P = .023) but no significant difference in overall survival was seen in the stage II population. The 10-year follow-up on overall survival corroborated the aforementioned trend results. Neuropathy was seen in 92% of patients who received FOLFOX4, with 13% being severe but mostly reversible.
United States oncologists further modified the regimen, including FOLFOX6 (a single-day regimen) and FOLFOX7 (no 5-FU bolus). In a retrospective review of unselected patients with stage II disease, the 5-year DFS benefit for FOLFOX compared with 5FU/LV alone was not statistically significant (84% compared to 80%, hazard ratio for recurrence 0.84, p = 0.26). However, survival significantly exceeded 5% (82% versus 77%) for patients with stage II tumors with high-risk clinical features such as poor histological grade, T4, perforation/obstruction, less than 10 lymph nodes sampling, perineural invasion (PNI), and lymphovascular invasion (LVI).
Other trials in 2011 confirmed the value of oxaliplatin-based regimens as a component of adjuvant chemotherapy for stages II and III colon cancer, surpassing the effectiveness of 5-FU/LV monotherapy. The NSABP C-07 phase III clinical trial evaluated the impact on DFS of adding oxaliplatin to bolus weekly 5-FU/LV as surgical adjuvant therapy for stage II (29%) and III (71%) colorectal adenocarcinoma patients. After intent of curative resection, patients were randomly assigned to 1 of 2 regimens. The first is 5-FU (500 mg/m2 IV) bolus weekly for 6 weeks plus leucovorin (500 mg/m2 IV) weekly for 6 weeks during each 8-week cycle for 3 cycles. The other has the same 5-FU/LV regimen with oxaliplatin (85 mg/m2 IV) administered on weeks 1, 3, and 5 of each 8-week cycle for 3 cycles (the fluorouracil/leucovorin/oxaliplatin or “FLOX” regimen).
In the NSABP C-07 trial, the 8-year overall survival was similar between treatment groups (hazard ratio, 0.88; 95% confidence interval, 0.75 to 1.02; p = 0.08). FLOX remained superior for DFS (hazard ratio, 0.82; 95% confidence interval, 0.72 to 0.93; p = 0.002). The effect of oxaliplatin on overall survival did not differ by stage of disease (stage II compared to stage III = 0.38 for overall survival; 0.37 for DFS) but did vary by age (younger than 70 compared to older than 70; HR = 0.39) with a similar trend for DFS (p = 0.073). Oxaliplatin significantly improved overall survival in patients younger than 70 (hazard ratio, 0.80; 95% confidence interval, 0.68 to 0.95; p = 0.013). However, no positive effect was seen in older patients. FLOX regimen was associated with higher hospitalization rates for diarrhea (5.5% compared to 3%), and a total of 1.2% of patients died of any cause within 60 days of receiving chemotherapy, with no significant difference between regimens.
The XELOXA trial was a multicenter, randomized trial comparing capecitabine plus oxaliplatin (XELOX) with bolus 5-FU/LV as adjuvant therapy for individuals with stage III colorectal cancer. Patients were randomly assigned to XELOX (Oxaliplatin 130 mg/m2 on day 1 plus Capecitabine 1000 mg/m2 twice daily on days 1 to 14 every 3 weeks for 24 weeks) or the standard bolus 5-FU/LV adjuvant regimen. XELOX improved DFS and overall survival compared with bolus 5-FU/LV in patients with resected stage III colorectal cancer after a median follow-up of almost 7 years (DFS 63% compared to 56%, hazard ratio, 0.80; 95% confidence interval; 0.69; 0.93; p = 0.0045 and OS 73% compared to 67%, hazard ratio, 0.83; 95% confidence interval, 0.70 to 0.99; P = .04).
XELOX was associated with more neurotoxicity, hand-foot syndrome, and thrombocytopenia. Patients on capecitabine are advised not to take a proton pump inhibitor to avoid increasing gastric pH and lowering absorption. Another trial established that 6 months of oral capecitabine monotherapy is a safe and equally effective alternative to conventional 5-FU/LV for stage III colon cancer.
Adjuvant chemotherapy may be helpful for selected patients with stage II high-risk disease. The largest study of Stage II colorectal cancer, the UK QUick And Simple And Reliable (QUASAR) trial, randomly assigned nonstratified patients (eg, high-risk and low-risk) to receive 5-FU/LV with or without levamisole (later removed) as adjuvant chemotherapy following surgical resection. The relative risk of death from any cause with chemotherapy versus observation alone was 0.82 (95% confidence interval 0.70 to 0.95; p=0.008) and for recurrence relative risk 0.78 (0.67-0.91; p=0.001) after a 10-year follow-up. The absolute survival improvement with 5-FU/LV was 3.6%. However, the trial’s quality has been questioned due to a poor median of 6 lymph node dissection (> 60% with < 12 lymph nodes), a group of patients received radiation therapy (14%) or portal infusion chemotherapy (6%), which does not meet current standards.
The ACCENT retrospective analysis has demonstrated a trend toward an improved 10-year DFS and overall survival for stage II disease with chemotherapy compared to observation, regardless of the risk feature with high-risk disease (51% compared to 35%). The identification of high-risk prognostic factors may help identify patients at higher relapse risk who will more likely benefit from adjuvant therapy. Datasets confirmed that patients with stage II colorectal cancer without high-risk features and MSI-H/dMMR have an excellent prognosis and do not need adjuvant chemotherapy. However, the need for adjuvant chemotherapy in patients with high-risk disease remains uncertain.
Irinotecan-based regimens are effective in palliative therapy for advanced colorectal cancer. However, for unknown reasons, none of the 3 major phase III trials (Cancer and Leukemia Group B 89803 or CALGB89803, Pan-European Trials in Alimentary Tract Cancers 3 or PETACC-3, and Adjuvant Colorectal Cancer Endpoints or ACCORD) using irinotecan combination regimens with 5-FU/LV has demonstrated that the regimen confers significantly superior 3-year DFS when compared with 5-FU/LV alone.
The roles of novel targeted agents, bevacizumab (an antibody against vascular endothelial growth factor) and cetuximab (an antibody against epidermal growth factor receptor) have been investigated in the adjuvant setting in large phase III trials. Three major trials have failed to demonstrate any benefit of adjuvant bevacizumab with FOLFOX (NSABP C-08), XELOX (Avastin in Adjuvant Treatment of Colon Cancer or AVANT trial) or Capecitabine (QUASAR2). Cetuximab was also tested as part of adjuvant therapy for stage III colon cancer alongside the FOLFOX regimen. However, this agent did not enhance outcomes, even in cases of preselected KRAS wild-type tumors, and proved harmful to patients with KRAS mutations. Cetuximab's lack of efficacy was later confirmed in the PETACC-8 trial on patients with RAS and BRAF wild-type stage III colon cancer.
Based on prior clinical trial results, the standard adjuvant chemotherapy for stage III colon cancer is an oxaliplatin-containing regimen (FOLFOX, XELOX, or FLOX) administered for 6 months. Capecitabine or 5-FU/LV monotherapy should be reserved for patients not considered optimal candidates for oxaliplatin (eg, those with pre-existing neuropathy). Stage III colon cancer patients with MSI-high/dMMR tumors are intrinsically resistant to adjuvant 5-FU monotherapy, requiring the addition of oxaliplatin to overcome the resistance and impact outcomes. Patients with Stage II colon cancer and any high-risk combination should discuss the risks and benefits of adjuvant therapy. Retrospective analysis from trials did not document a significant improvement with the addition of oxaliplatin to 5-FU/LV for patients older than 70, and only younger patients had a statistically significant DFS, overall survival, and time to tumor recurrence.
Currently, irinotecan-based and targeted therapies have no indication in colon cancer adjuvant therapy outside of investigational trials. No conclusive evidence exists to recommend standard radiation therapy alone or combined chemoradiotherapy in the adjuvant setting. Two web-based validated tools are available to calculate the relative risk of disease recurrence and mortality based on clinicopathological features and potential adjuvant benefits (an ACCENT tool by the Mayo Clinic and Adjuvant! Online). Furthermore, gene profiling by Oncotype DX Colon, Colorectal Cancer Assay (ColDX) or ColoPrint are currently used in clinical practice to assist in risk assessment. However, these tools have no valid predictive value and are thus not recommended by clinical practice guidelines.
Neoadjuvant Therapy
The role of preoperative chemotherapy for patients with colorectal cancer is currently being investigated in a phase III Fluoropyrimidine Oxaliplatin and Targeted Receptor Preoperative Therapy (FOxTROT) trial (National Clinical Trial 00647530 or NCT00647530) after the pilot study showed promising results. The FOxTROT collaborative group randomized candidates with locally advanced resectable lesions (T3 with > 5 mm invasion beyond the muscularis propia and T4) to 2 regimens. The first is 3 preoperative FOLFOX cycles (Oxaliplatin; 85 mg/m2, Leucovorin; 175 mg, Fluorouracil; 400 mg/m2 bolus, then 2400 mg/m2 via 46-hour infusion), surgery, and 9 additional cycles. The second is surgery and 12 adjuvant cycles. Findings favored neoadjuvant therapy, showing significant improvements in tumor regression (31% compared to 2%), node-positive (1% compared to 20%), and negative margins (4% compared to 20%), resulting in significant downstaging (p=0.04).
Systemic Therapy
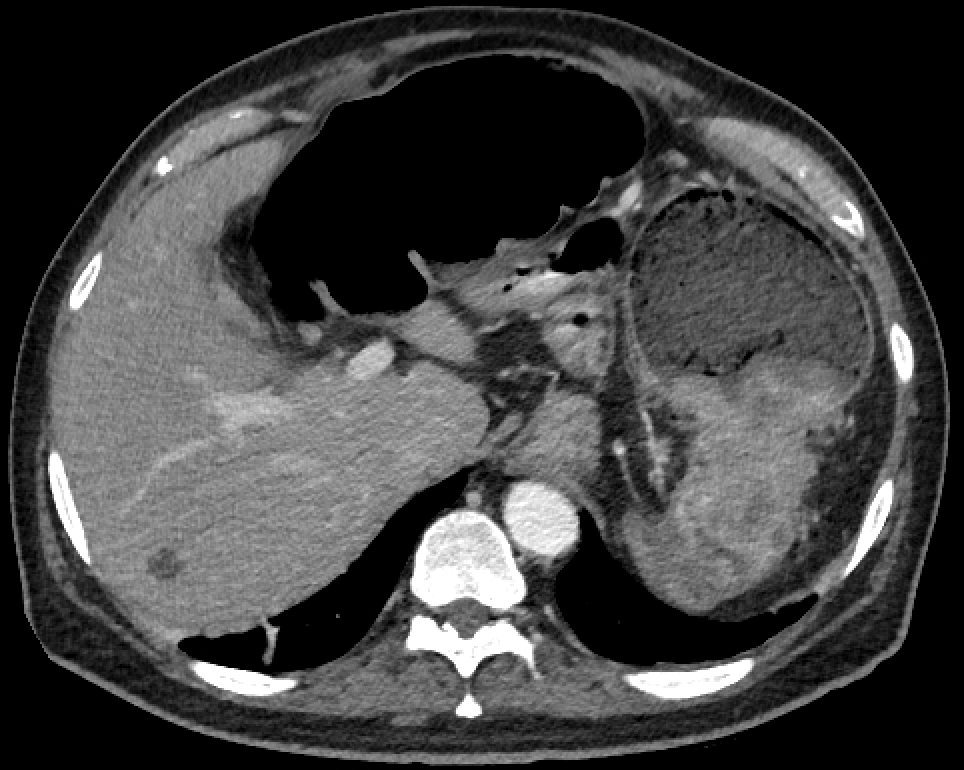
More than half of all patients with colorectal cancer develop metastasis, with most tumors metastasizing to the liver (80% to 90%). The prognosis for advanced nonresectable and metastatic colon cancer with best supportive care is poor, with a median overall survival (mOS) of 5 to 6 months. However, a subset of patients with oligometastatic hepatic or pulmonary involvement are potentially curable with perioperative chemotherapy. Systemic therapy’s goals for advanced nonresectable and metastatic colon cancer are symptom palliation, quality of life enhancement, and survival prolongation.
Systemic therapy for colon and rectal cancers is addressed jointly by clinical research and practice. In the 1990s, 5-FU/LV monotherapy was the standard first-line therapy, with an approximate mOS of 12 months. Adding oxaliplatin and irinotecan to the 5-FU/LV backbone in the early 2000s resulted in a mOS improvement to nearly 24 months. The introduction of biologic agents, including monoclonal antibodies (MAbs) targeting vascular endothelial growth factors (VGFRs) and epidermal growth factor receptor (EGFR), further enhanced the efficacy of systemic medical therapy, with mOS reaching 36 months and an impressive 20% 5-year overall survival even at a metastatic stage after exposure to multiple lines of therapy.
The current availability of 9 antineoplastic classes and over a dozen drugs for metastatic colorectal cancer offers numerous therapeutic possibilities, with varied combinations and sequences not yet established. These agents include fluoropyrimidines, capecitabine, S-1, tegafur plus uracil (UFT), irinotecan, oxaliplatin, anti-EGFRs (ie, cetuximab or panitumumab), anti-VEGFRs (ie, bevacizumab and ramucirumab), the recombinant fusion protein aflibercept, the tyrosine kinase inhibitors regorafenib, antimetabolites like TAS-102, and immunotherapeutic agents (ie, nivolumab and pembrolizumab).
The most appropriate treatment regimen conceivably generates the highest overall response rate (ORR), greatest impact on metastases for surgical conversion, longest progression-free (PFS) and overall survival, and a favorable toxicity profile. Treatment decisions for specific patient subpopulations may be guided by predictive biomarkers (RAS/BRAF type and MMR/MSI status), primary location (tumor and metastasis), patient factors (performance status and comorbidities), and therapy goals (palliation or conversion).
For otherwise healthy candidates, the standard first-line treatment approach is to start with a FOLFOX, CAPOX, or Folinic Acid/Fluorouracil/Irinotecan (FOLFIRI) regimen plus an anti-EGFR agent when the tumor is RAS/BRAF wild-type and left-sided or anti-VGFR when the tumor is RAS/BRAF mutated or right-sided. Disease progression or unacceptable toxicity warrants switching to a second-line regimen with either continuation of prior anti-VGFR or using a new biological agent regardless of the tumor location. ASCO, ESMO, and NCCN recommend comprehensive testing of KRAS, NRAS exons 2 (codons 12 and 13), 3 (codons 59 and 61), 4 (codons 117 and 146) and BRAF V600E for anti-EGFR candidates based on the results of the Panitumumab Randomized Trial in Combination with Chemotherapy for Metastatic Colorectal Cancer to Determine Efficacy (PRIME) trial and other major meta-analyses.
Incorporating biological agents into chemotherapy regimens has markedly enhanced ORR, DFS, and overall survival in the first- and second-line settings. Cetuximab and panitumumab exhibit comparable effectiveness in first- and second-line treatments and single-agent salvage therapy. However, cross-resistance may develop from using these agents, limiting their use after anti-EGFR treatment failure. Bevacizumab may be continued into second-line therapy after first-line progression, particularly for RAS/BRAF-mutated cases, but not in combination with new anti-EGFR agents for RAS/BRAF wild-type and left-sided tumors. Patients who progress despite anti-VEGF therapy may consider adding aflibercept or ramucirumab to their chemotherapy regimen.
Sequential single agents remain a valid option for patients with metastatic colorectal cancer compared to combination treatments demonstrated in the United Kingdom Medical Research Council's Fluorouracil, Oxaliplatin, CPT-11: Use and Sequencing (FOCUS) and Dutch Colorectal Group’s capecitabine/irinotecan/oxaliplatin (CAIRO) trials. Biological agents were not used in either trial, and most patients did not receive all 3 drugs. Multiple phase III trials have confirmed similar ORR, PFS, and overall survival rates between FOLFOX and FOLFIRI regimens, even with added anti-VEGFs or anti-EGFRs. In clinical practice, the choice between FOLFOX and FOLFIRI is based on the treatment toxicity profile. The capecitabine-oxaliplatin (CAPOX) combination is a statistically noninferior substitute to the FOLFOX regimen in PFS and OS with a tolerable toxicity profile. Conversely, the capecitabine-irinotecan (XELIRI) combination has shown higher intolerable rates of gastrointestinal toxicities. Maintenance therapy with low-dose capecitabine-bevacizumab after the first-line FOLFOX-bevacizumab good response is an accepted treatment option based on CAIRO3 trial results. Complete chemotherapy discontinuation may be detrimental and remains controversial. Meanwhile, intermittent treatment has not significantly reduced overall survival but, instead, improved quality of life.
FOLFOX with irinotecan (FOLFOXIRI) with or without bevacizumab is reserved for conversion approach in potentially resectable liver/lung metastasis on selected patients with excellent performance status. Consensus-based guidelines for individuals unfit for triple or double therapies recommend 5-FU/LV IV or capecitabine PO monotherapy. Patients eligible for further chemotherapy after progression on FOLFOX, CAPOX, or FOLFIRI with anti-VEGFs and anti-EGFRs may explore regorafenib or TAS-102 as salvage therapy. Alternatively, immunotherapy is approved for MSI-H/dMMR tumors. Clinical trials may offer access to novel targeted agents following failure on various therapeutic lines.
The recommended treatment monitoring involves close observation for signs and symptoms of adverse reactions before each treatment cycle and as needed. Blood work parameters should be checked frequently, also before each treatment cycle and as indicated. Serial CEA assays are recommended every 1 to 3 months, and radiographic evaluation using Response Evaluation Criteria In Solid Tumors (RECIST) should be performed every 2 to 3 months by an interprofessional team. Patients should also be regularly screened for somatic symptoms and psychosocial distress.
Selected Landmark Clinical Trials
Pivotal studies have shaped the standard of care for colorectal cancer treatment. Introducing new colorectal cancer therapies has significantly improved both efficacy and safety profiles, offering patients better outcomes and quality of life. These interventions are described below.
Cytotoxic chemotherapy
Cytotoxic agents target rapidly dividing cancer cells, thereby inhibiting tumor proliferation and promoting cancer cell death. These medications include 5-FU/LV, capecitabine, irinotecan, and oxaliplatin.
An updated meta-analysis compared 5-FU/LV to 5-FU alone. The combination regimen produced a higher ORR (21% compared to 11%) and 1-year overall survival (47% compared to 37%). The 2 most commonly used regimens in the United States include the Mayo regimen (bolus 5-FU 425 mg/m2 and leucovorin 20 mg/m2 on days 1 to 5 every 4 to 5 weeks) and the Roswell Park regimen (bolus 5-FU 500 mg/m2 and leucovorin 500 mg/m2 administered weekly for 6 out of 8 weeks).
The outcomes further improve by using the de Gramont regimen, with leucovorin 200 mg/m2 given as a 2-hour infusion followed by bolus 5-FU 400 mg/m2 and 22-hour infusion 5-FU 600 mg/m2 for 2 consecutive days every 2 weeks). Outcome measures include better ORR (33% compared to 14%), longer PFS (7 compared to 5 months) and overall survival (15.5 versus 14.2 months), and significantly less grade 3/4 toxicities (23.9% compared to 11.1%) than the Mayo regimen.
For capecitabine, Hoff PM et al’s phase III clinical trial prospectively randomly assigned patients to either oral capecitabine (1250 mg/m2 twice daily for 14 days every 21 days) or 5-FU/LV Mayo regimen, resulting in noninferior ORR (24.8% compared to 15.5%), time to progression (TTP 4.3 compared to 4.7 months) and mOS (12.5 compared to 13.3 months). Capecitabine’s common side effects included diarrhea (overlapping toxicities with irinotecan), hyperbilirubinemia, and hand-foot syndrome. Capecitabine has never been directly compared with infusional 5-FU/LV using the de Gramont regimen. However, CAPOX and infusional FOLFOX have been shown to have similar efficacy in advanced colon cancer treatment by the Three Regimens of Eloxatin Evaluation-1 (TREE-1) and Arbeitsgemeinschaft Internistische Onkologie (AIO) trials.
In clinical practice in the United States, reducing the dose of capecitabine by approximately 20% (to 1000 mg/m2) either alone or in combination with other regimens does not seem to diminish treatment effectiveness. However, this strategy significantly enhances the treatment's safety profile. Additionally, alternative oral fluoropyrimidines unapproved in the United States include different agents derived from S1: tegafur-uracil, gimeracil, and oteracil, as well as raltitrexed.
For irinotecan, a landmark phase II clinical trial was conducted where patients with 5-FU-refractory metastatic colon cancer were randomly assigned to either single-agent irinotecan (300 mg/m2 every 3 weeks) or best supportive care (BSC). The drug regimen demonstrated a significant 1-year overall survival (36% compared to 14%) with improved quality of life (better performance status, weight, and pain levels). Following this outcome, 3 key trials were conducted to test irinotecan’s role versus 5-FU/LV in the front-line setting. A 3-arm trial compared 3 treatment regimens: the Roswell Park regimen, irinotecan with 5-FU/LV weekly bolus regimen (the IFL or Saltz regimen), and irinotecan alone. The trial results significantly favored IFL with an ORR (39% compared to 21%) and mOS (14.8 compared to 12.6 months).
In Europe, 3 pivotal phase III trials compared the 5-FU/LV and FOLFIRI regimens. The Douillard FOLFIRI regimen included irinotecan (180 mg/m2 on day 1), 5-FU (400 mg/m2 bolus followed by 600 mg/m2 over 22 hours, both on days 1 and 2), and leucovorin (200 mg/m2 on days 1 and 2). The Douillard FOLFIRI regimen trial demonstrated a significant ORR (49% compared to 31%), TTP (6.7 compared to 4.4 months), and mOS (17.4 compared to 14.1 months). However, higher incidences of diarrhea, myelosuppression, and alopecia were observed in the irinotecan group. Irinotecan combinations require adequate biliary function for the drug’s active glucuronide metabolite, SN-38, to be excreted. Approximately 10% of United States patients are homozygous for the UGT1A1*28 allele polymorphism, which increases SN-38 bioavailability and, therefore, requires starting with a lower irinotecan dose.
Oxaliplatin has very limited activity in colorectal cancer as a single agent thus not recommended unless synergist with fluoropyrimidines. In the phase III trial, FU/LV (de Gramont regimen) was compared with or without OXA (OXA: 85 mg/m2 on day 1 over 2 hours FOLFOX4 regimen) as first-line therapy for patients with mCRC. FOLFOX4 regimen had significantly higher ORR (51% versus 22%) and PFS (9 compared to 6 months) but comparable mOS (16.2 versus 14.7 months) with more grade 3/4 neutropenia, diarrhea, and neurotoxicity. Because no overall survival benefit was achieved in these first-line trials, the FDA did not approve oxaliplatin for colorectal cancer until years later for second-line therapy that showed prolonged PFS and increased ORR compared with FU/LV for patients who experienced disease progression while receiving first-line irinotecan regimens. The most important side effect and dose-limiting toxicity of oxaliplatin is neurotoxicity. It may present as an acute and reversible, cold-triggered sensory neuropathy, or a chronic dose-limiting cumulative sensory neurotoxicity.
Oxaliplatin has very limited activity in colorectal cancer as a single agent and is thus not recommended unless it is used to synergize with fluoropyrimidines. In a phase III trial, 5-FU/LV using the de Gramont regimen was compared with or without oxaliplatin (oxaliplatin: 85 mg/m2 on day 1 over 2 hours, FOLFOX4 regimen) as first-line therapy for patients with metastatic colorectal cancer. The FOLFOX4 regimen showed a significantly higher ORR (51% compared to 22%) and PFS (9 compared to 6 months) but comparable mOS (16.2 compared to 14.7 months) and with more grade 3/4 neutropenia, diarrhea, and neurotoxicity.
Since no overall survival benefit was achieved in these first-line trials, the FDA did not approve oxaliplatin for colorectal cancer until years later for second-line therapy, which showed prolonged PFS and increased ORR compared with 5-FU/LV for patients who experienced disease progression while receiving first-line irinotecan-based regimens. Oxaliplatin’s most important, dose-limiting adverse effect is neurotoxicity, which may present as acute and reversible cold-triggered sensory neuropathy or chronic dose-limiting cumulative sensory neurotoxicity.
With oxaliplatin and irinotecan’s encouraging trial results in the United States and Europe, the North Central Cancer Treatment Group (NCCTG)/Intergroup trial N9741 performed a pivotal and practice-changing trial comparing FOLFOX4, the standard combination IFL, and the new irinotecan oxaliplatin (IROX) combination (oxaliplatin 85 mg/m2 with irinotecan 200 mg/m2, both on day 1 every 3 weeks). The N9741 results demonstrated FOLFOX’s superiority over IFL and IROX as first-line therapy for metastatic colon cancer with ORR (45% compared to 31% and 36%), PFS (8.7 compared to 6.9 and 6.7 months) and mOS (19.5 compared to 15 and 17.3 months). The toxicity profile likewise favored FOLFOX, except for neurotoxicity. FOLFOX emerged as the new standard first-line therapy with rapid and widespread adaptation in the United States.
VEGF inhibitors
VEGF inhibitors work by inhibiting VEGF, a key signaling protein involved in angiogenesis. In colon cancer, this mechanism helps suppress the formation of new blood vessels within tumors, thus reducing their blood supply and growth. The widely used agents in this class are bevacizumab, aflibercept, and ramucirumab.
In a randomized placebo-controlled phase III trial, IFL with bevacizumab (5 mg/kg every 2 weeks) was assessed as a first-line therapy for metastatic colorectal cancer. For the first time, the addition of an anti-VEGF inhibitor was validated as an efficacious antineoplastic treatment by significantly improving ORR, PFS, and mOS. This trial was the first phase III validation of an antiangiogenic agent as an effective treatment option in human malignancy. Subsequently, FOLFOX with bevacizumab (FOLFOX-BEV) also showed improved mOS in the first-line and second-line settings.
The Avastin in Elderly Colorectal Cancer Patients (AVEX) phase III trial selected patients age 70 or older ineligible for oxaliplatin or irinotecan-based chemotherapy first-line regimens to receive capecitabine regimen alone or with bevacizumab (7.5 mg/kg intravenously on day 1 given every 3 weeks). The study showed a significantly longer median progression-free survival (mPFS) and a remarkable improvement in mOS for capecitabine-bevacizumab (CAP-BEV) than with capecitabine alone.
Prolonged VEGF inhibition with bevacizumab beyond the first-line progression was evaluated by the European Therapy for Metastatic Colorectal Cancer (ML18147) phase III trial. Patients who experienced progression within 3 months were randomly assigned to either continue second-line therapy with or without bevacizumab. The mOS, the study’s primary endpoint, favored continuing with bevacizumab with chemotherapy over chemotherapy alone. PFS improvement confirmed this effect but not ORR. The toxicity profile observed with bevacizumab included hypertension, bleeding, gastrointestinal perforations, impaired wound healing, and arterial-venous thrombotic events.
In the placebo-controlled phase III Aflibercept Plus FOLFIRI vs. Placebo Plus FOLFIRI in Second-Line Metastatic Colorectal Cancer (VELOUR) trial, aflibercept was assessed in the second-line setting for patients who had progressed on oxaliplatin-based chemotherapy, with or without bevacizumab, in the first line. Patients randomly assigned to receive FOLFIRI with aflibercept (4 mg/kg IV every 2 weeks) demonstrated a significant improvement in ORR (19.8% compared to 11.1%), PFS (6.9 compared to 4.7 months), and mOS (13.5 compared to 12.1 months). However, the aflibercept arm exhibited an increased incidence of grade 3/4 diarrhea, mucositis, neutropenia, infection, fatigue, hypertension, proteinuria, hemorrhage, and arterial-venous thromboembolic events, typically observed in second-line FOLFIRI with bevacizumab (FOLFIRI-BEV).
In the double-blinded, placebo-controlled Ramucirumab in Colorectal Cancer: Efficacy and Safety (RAISE) trial, adding ramucirumab (8 mg intravenously every two weeks) to FOLFIRI as second-line therapy for patients who progressed with FOLFOX plus bevacizumab showed improved PFS (5.7 compared to 4.5 months) and mOS (13.3 compared to 11.7 months). However, the combination arm had worse grade 3/4 neutropenia, hypertension, diarrhea, and fatigue.
Anti-EGFR monoclonal antibodies
Anti-EGFR monoclonal antibodies block EGFR on cancer cells, inhibiting downstream signaling cascades involved in cell proliferation, survival, and angiogenesis. These agents cause tumor growth inhibition and enhanced immune response against cancer cells. Agents in this caregory include cetuximab and panitumumab.
Cetuximab monotherapy (400 mg/m2 followed by a weekly infusion of 250 mg/m2) in patients who had experienced disease progression on prior 5-FU, oxaliplatin, and irinotecan-based therapy had an improved ORR (40% compared to 11%) and mOS (6.1 compared to 4.6 months) with BSC as the comparator.
The Evaluation of Panitumumab in Colorectal Cancer to Improve Survival (EPIC) and Biomarker Oncology Research and Development (BOND) trials proved the PFS and ORR superiority of irinotecan-cetuximab (IRI-CET) over irinotecan alone on patients with prior irinotecan failure, without significantly improving survival. A large multicenter randomized phase III Cetuximab Combined With Irinotecan in First-Line Therapy for Metastatic Colorectal Cancer (CRYSTAL) trial, using the regimen FOLFIRI with or without cetuximab in treatment-naive colorectal cancer patients, confirmed that selected patients with wild-type KRAS have a significantly higher ORR, PFS, and mOS (23.5 compared to 20 months).
The benefit of FOLFOX-cetuximab (FOLFOX-CET) remains uncertain. Three trials, the Oxaliplatin and Cetuximab in First-Line Treatment of Metastatic Colorectal Cancer (OPUS), Cancer and Leukemia Group B (CALGB) 80203, and CALGB 80405, showed that the regimen only had modest significant ORR and PFS improvements but no mOS benefit. Three other trials, the Medical Research Council (MRC) COIN, NORDIC VII, and New EPOC demonstrated the treatment’s lack of benefit. The cetuximab arm had higher-grade diarrhea, magnesium-wasting syndrome, infusion reaction, and ocular-skin toxicity, with the last correlating to response rate.
Single-agent panitumumab (6 mg/kg every 2 weeks) was compared to BSC in a large international phase III trial in patients with chemotherapy-refractory metastatic colorectal cancer. Panitumumab had an ORR of 37%, similar to cetuximab, and a modestly prolonged mPFS of 8 compared to 7.3 weeks. However, mOS was not increased, likely due to patients crossing over from the BSC arm to the panitumumab arm. The A Study of Panitumumab Efficacy and Safety Compared to Cetuximab (ASPECCT) phase III trial directly compared panitumumab with cetuximab monotherapies in patients with chemotherapy-refractory disease and showed noninferior mOS (10 months) with a similar expected toxicity profile. The FOLFOX4-panitumumab (FOLFOX4-PAN) benefit in the first-line setting was seen in the phase III Panitumumab Randomized Trial in Combination with Chemotherapy for Metastatic Colorectal Cancer to Determine Efficacy (PRIME) trial with an mPFS improvement (9.6 compared to 8 months) and a trend for mOS (23.0 compared to 19.7 months), although not significant at 55 weeks follow-up.
Comparing VEGF inhibitors with anti-EGFR monoclonal antibodies
The FOLFIRI Plus Cetuximab versus FOLFIRI plus Bevacizumab as First-Line Treatment for Patients with Metastatic Colorectal Cancer (FIRE-3) trial enrolled treatment-naïve patients with metastatic colorectal cancer with KRAS exon2 wild-type status and randomly assigned them to receive FOLFIRI with cetuximab (FOLFIRI-CET) or FOLFIRI with bevacizumab (FOLFIRI-BEV). The trial’s primary endpoint, which looked at the ORR using an intention-to-treat approach, did not show a significant difference between the 2 groups (cetuximab’s 62% compared to bevacizumab’s 58%, p = 0.18). While progression-free survival (PFS) was similar between the 2 arms (cetuximab’s 10 months compared to bevacizumab’s 10.3 months), the mOS was significantly longer in the FOLFIRI-CET arm (cetuximab’s 28.7 months compared to bevacizumab’s 25.0 months; hazard ratio, 0.77; p = 0.017).
An updated analysis, considering additional mutations in KRAS exon 3 and 4 and NRAS exon 2 and 3 showed an even longer mOS of 33.1 months for FOLFIRI-CET. However, the U.S. Intergroup study, CALGB/Southwest Oncology Group (SWOG) 80405 trial, which compared FOLFOX or FOLFIRI (chosen by the physician) with cetuximab versus bevacizumab as first-line therapy, found no difference in mOS (cetuximab had 30 months compared to bevacizumab’s 29.9 months), even with expanded RAS-mutated analysis. Preliminary retrospective analysis suggests that patients with KRAS wild-type left-sided tumors treated with cetuximab had a significantly higher mOS compared to individuals with right-sided tumors (33.3 months and 19.4 months, respectively). Combination therapy with VEGF inhibitors and anti-EGFR monoclonal antibodies has shown no benefit and even harm in multiple trials (BOND-2, PACCE, CAIRO-2), and is therefore not recommended.
An updated analysis, which accounted for additional mutations in KRAS exons 3 and 4, as well as NRAS mutations exons 2 and 3, demonstrated a longer mOS survival of 33.1 months for FOLFIRI-CET. In contrast, the U.S. Intergroup study, CALGB/South-west Oncology Group (SWOG) 80405 trial that compared FOLFOX or FOLFIRI (dealer’s choice) with CET compared with BEV as first-line therapy had no difference in mOS (30 versus 29.9 months, respectively), not even whit expanded RAS-mutated analysis. The preliminary retrospective analysis suggests that patients treated with CET for KRAS wild-type left-sided tumors mOS are significantly higher than right-sided counterparts by 33.3 versus 19.4 months, respectively. Regimens combining VEGF inhibitors and anti-EGFRs monoclonal antibodies have failed, even proved detrimental, in multiple trials (BOND-2, PACCE, and CAIRO-2) and are thus not recommended.
Immune checkpoint inhibitors
Immune checkpoint inhibitors work by targeting specific proteins that act as brakes on the immune system's ability to attack cancer cells. In a phase II study, pembrolizumab 10 mg/kg every 14 days was given to 11 heavily pretreated patients with dMMR metastatic colorectal cancer with a remarkable ORR of 71% and PFS rate of 67%. In an expanded cohort of 54 patients, pembrolizumab showed an ORR of 50% and an 89% disease control rate with a durable response for more than a year, not seen in pMMR colon cancer. In CheckMate-142, nivolumab (3mg/kg every 2 weeks) was given to 74 patients with dMMR colon cancer, resulting in 31% objective response, 69% disease control, and median duration response not reached at 12 months.
Salvage therapy for refractory disease
The efficacy of regorafenib 160 mg PO daily for 3 weeks in a 4-week cycle was investigated in a placebo-controlled, multicenter international, randomized, phase III CORRECT trial after the progression of multiple therapies. Regorafenib had a higher ORR (41% compared to 15%) and PFS (1.9 compared to 1.7 months) than placebo, with modest but significant mOS benefit (6.4 compared to 5.0 months, p = 0.0052). The observed toxicity profile with regorafenib included hand-foot skin reaction, fatigue, hypertension, diarrhea, and rash, with a 1.6% fatal hepatic failure rate. The CONCUR trial later confirmed regorafenib’s benefit.
The international, double-blind, placebo-controlled, randomized-controlled, phase III RECOURSE study of patients with refractory disease showed that Trifluridine-tipiracil (TAS-102) 35 mg/m2 orally twice daily on days 1 through 5 and 8 to 12 of each 28-day cycle improved ORR (44% versus 16%), DFS and mOS (7.1 versus 5.3 months). The most serious adverse events were neutropenia (38%), febrile neutropenia (4%), and a treatment-related death.