Introduction
The auriculotemporal nerve is a tributary of the mandibular division of cranial nerve five, the trigeminal nerve. It contains sensory, vasomotor, and parasympathetic fibers. It has a superior and inferior root that originates from the trigeminal nerve, encircles the middle meningeal artery ultimately traveling inferior to the temporomandibular joint and up the temple providing sensation to parts of the ear, temporomandibular joint, scalp, as well as secretory and vasomotor innervation to the parotid gland. This nerve is clinically relevant in the setting of temporal mandibular joint disease repair, postoperative complications in a parotidectomy, and trigeminal neuralgia.
Structure and Function
The auriculotemporal nerve contains secretomotor, somatosensory, and vasomotor fibers. This nerve originates from the sensory nucleus of the trigeminal nerve in the pons. The mandibular branch of the trigeminal nerve exits the cranium out of the foramen ovale. After exiting the skull, the auriculotemporal nerve branches off where it has a superior and posterior root encircling the middle meningeal artery before joining together to form one nerve. After both roots fuse, it continues posterior to the lateral pterygoid muscle and travels between the sphenomandibular ligament and the neck of the mandible. The nerve lies posterior the parotid gland where it gives off parasympathetic and vasomotor fibers before it travels just inferior to the superior aspect of the mandibular condyle of the temporal mandibular joint. As it continues to travel superior, past the temporal mandibular joint, in the infratemporal fossa, it shares an intimate relationship with the superficial temporal artery. Along its path, it anastomoses with the facial nerve on the and the otic ganglion.
The superior root of the auriculotemporal nerve contains general somatic afferent fibers that provide sensation to the tragus and helix of the ear, the external portion of the tympanic membrane, the posterior temporomandibular joint, and the temple. The fibers originate from the trigeminal nucleus in the pons and travel with the mandibular division of the trigeminal nerve through the foramen ovale.
The inferior root of the auriculotemporal nerve contains general visceral efferent fibers that provide autonomic parasympathetic innervation to the parotid gland. The fibers originate in the inferior salivary nucleus as part of cranial nerve nine, the glossopharyngeal nerve, it passes through the tympanic canaliculus and divides into its branches, including, the lesser petrosal nerve. The lesser petrosal nerve synapses in the otic ganglion and the postsynaptic fibers pass to the auriculotemporal nerve.
Embryology
The auriculotemporal nerve is a division of the trigeminal nerve with some post otic ganglionic parasympathetic fibers from the glossopharyngeal nerve. The embryologic derivative of the trigeminal nerve is the first pharyngeal arch that begins to form around the fourth week of gestation and ultimately provides sensation to the ophthalmic, maxillary, and mandibular regions of the face, as well as motor function to the muscles of mastication in the developing fetus. The embryologic derivative of cranial nerve nine, the glossopharyngeal nerve, is the third pharyngeal arch which begins developing in the fourth week of gestation and provides branchial motor innervation to the stylopharyngeus muscle, general visceral efferent via parasympathetic fibers, and visceral sensory from the carotid body and sinus.
Nerves
There are five main branches to the auriculotemporal nerve; the anterior auricular, articular, parotid, superficial temporal and branches to the external auditory meatus:
- The anterior auricular branch provides somatosensory innervation to the skin of the ear, including the tragus and part of the helix.
- The articular branch provides somatosensory innervation to the posterior temporal mandibular joint
- The parotid branch receives its preganglionic fibers from the lesser petrosal nerve of the tympanic plexus originating from the glossopharyngeal nerve, before sending postganglionic general visceral efferent fibers within the parotid branch of the auriculotemporal nerve. This branch provides secretomotor innervation via parasympathetic fibers to the parotid gland and vasomotor via sympathetic innervation.
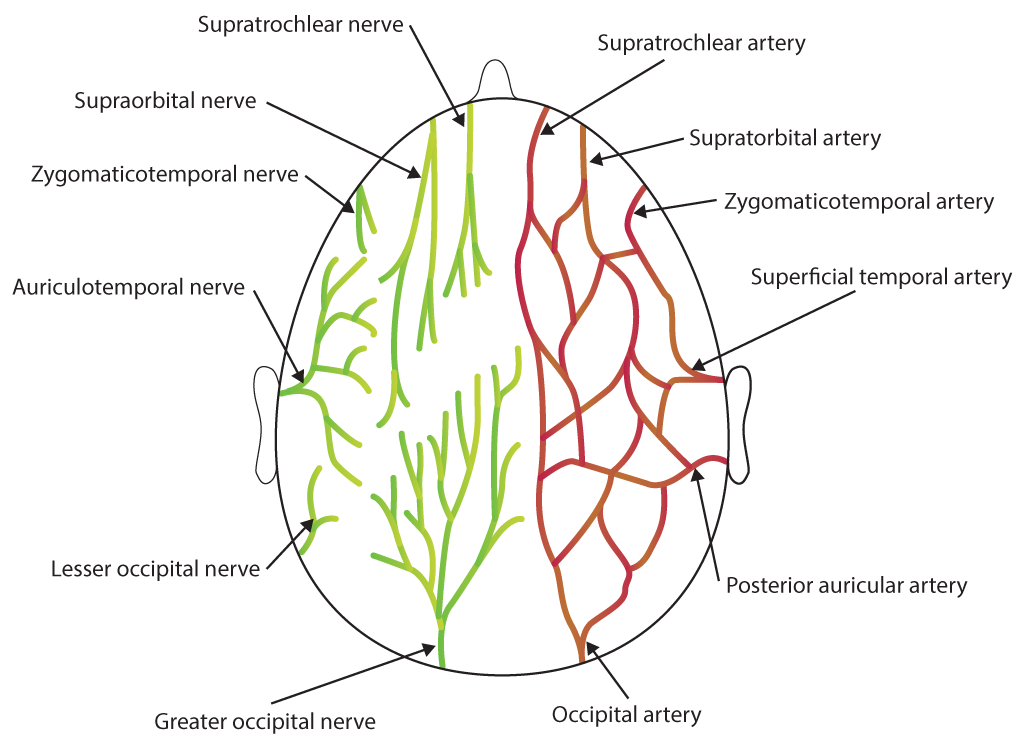
- The superficial temporal branches run posterior to the superficial temporal artery. These branches provide somatosensory innervation to the skin over the temple. This branch also anastomoses with the facial nerve and zygomaticotemporal nerve, a branch of the maxillary division of cranial nerve five, the trigeminal nerve.
- The branch to the external auditory meatus provides somatosensory innervation to the skin of the meatus as well as the tympanic membrane.
Physiologic Variants
The most common variant of the auriculotemporal nerve is seen in its branching pattern off of the trigeminal nerve. Although most often, the nerve has two roots, and an inferior root and a superior root, the literature describes variations of the number and location of the roots. In two reports of cadaveric dissections, there were various branching patterns reported, and researchers found that as few as one and as many as four roots can arise from the trigeminal nerve.[1][2]
Surgical Considerations
Due to the complex path of the auriculotemporal nerve, it merits consideration in various surgical procedures. In temporomandibular joint surgery, the nerve is vulnerable to damage as it courses 10 to 13 mm inferior to the superior edge of the mandibular condyle.[3][4] If damaged during surgery, the patient can develop pain or paresthesias in all terminal branches distal to the lesion, noted in the ‘Nerves' section above. Another surgical procedure in which preservation of this nerve is essential is in parotidectomy. Post parotidectomy, parasympathetic secretomotor fibers which were innervating the parotid gland can be damaged and have inappropriate regeneration to sympathetic receptors on salivary glands, which results in Frey syndrome discussed in Clinical Significance section below.[5]
Clinical Significance
Auriculotemporal nerve neuralgia and Frey syndrome are two common disorders of the auriculotemporal nerve.
- Neuralgia of the nerve can present as a throbbing unilateral pain in any of the sites of its terminal branches including the temporomandibular joint, skin of the scalp, skin of the external auditory meatus, skin of the ear, and the parotid gland. The neuralgia can result from compression along its path. One example of this is compression of the nerve by the lateral pyrgotid muscle upon mastication. Although uncommon, with an incidence rate at about 0.4%, diagnosis can be difficult due to its vague symptoms and has an extensive list of differential diagnoses which can include cervicalgia, temporomandibular joint disease, migraine, continuous hemicrania, otitis, trigeminal neuralgia, atypical facial pain, temporal arteritis, and odontalgia. Diagnosis is possible by blockade of the nerve with complete resolution of symptoms.[6][7] The treatment and relief of symptoms are achievable with botulinum toxin injection.[8]
-
Frey syndrome is unilateral sweating of the cheek and external ear accompanied by reddening of the area seen after eating or drinking food. Interestingly, it can also present if the affected patient thinks, sees, or dreams about food that causes salivation. The syndrome results from a lesion of the auriculotemporal nerve where inappropriate regeneration of damaged parasympathetic fibers regenerates innervating sympathetic receptors of salivary glands in the face. Frey syndrome is most commonly seen secondary to surgery, parotid gland infection or facial trauma and is the most common adverse side effect of a parotidectomy.[5] Treatment of Frey syndrome can include botulinum toxin, aluminum chloride, epoetin or intraoperative flaps, and implants can be used to prevent the seeding of fibers into unwanted locations.[9][10]