[1]
Mayes J, Davison E, Panahi P, Patten D, Eljelani F, Womack J, Varma M. An anatomical evaluation of the serratus anterior plane block. Anaesthesia. 2016 Sep:71(9):1064-9. doi: 10.1111/anae.13549. Epub 2016 Jul 20
[PubMed PMID: 27440171]
[2]
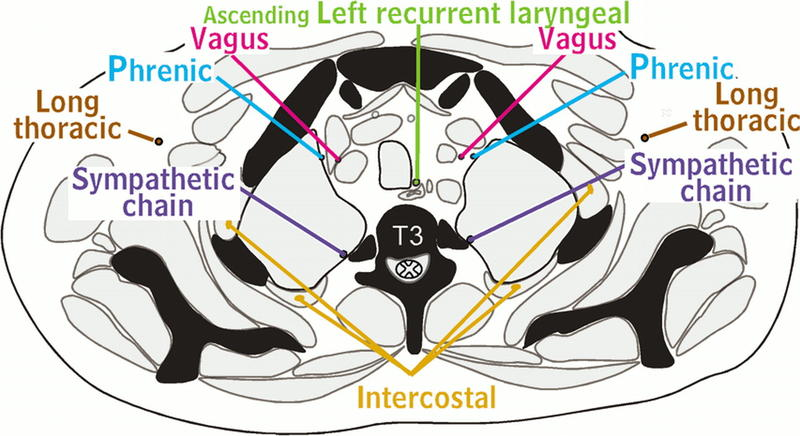
Kommuru H, Jothi S, Bapuji P, Sree D L, Antony J. Thoracic part of sympathetic chain and its branching pattern variations in South Indian cadavers. Journal of clinical and diagnostic research : JCDR. 2014 Dec:8(12):AC09-12. doi: 10.7860/JCDR/2014/9274.5246. Epub 2014 Dec 5
[PubMed PMID: 25653929]
[3]
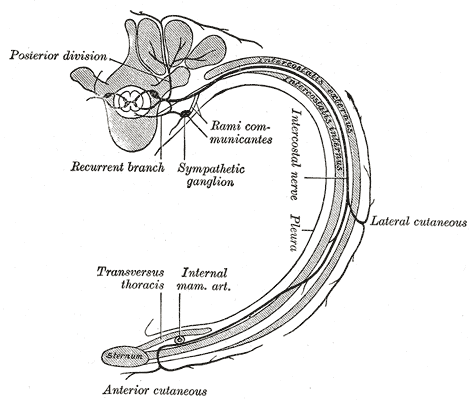
Iida T, Narushima M, Yoshimatsu H, Mihara M, Kikuchi K, Hara H, Yamamoto T, Araki J, Koshima I. Versatility of lateral cutaneous branches of intercostal vessels and nerves: anatomical study and clinical application. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2013 Nov:66(11):1564-8. doi: 10.1016/j.bjps.2013.06.056. Epub 2013 Jul 26
[PubMed PMID: 23896163]
[4]
Palussière J, Canella M, Cornelis F, Catena V, Descat E, Brouste V, Montaudon M. Retrospective review of thoracic neural damage during lung ablation - what the interventional radiologist needs to know about neural thoracic anatomy. Cardiovascular and interventional radiology. 2013 Dec:36(6):1602-1613. doi: 10.1007/s00270-013-0597-z. Epub 2013 Apr 11
[PubMed PMID: 23576208]
Level 2 (mid-level) evidence
[5]
Haam S, Kim D, Hwang J, Paik H, Lee D. An anatomical study of the relationship between the sympathetic trunk and intercostal veins of the third and fourth intercostal spaces during thoracoscopy. Clinical anatomy (New York, N.Y.). 2010 Sep:23(6):702-6. doi: 10.1002/ca.21001. Epub
[PubMed PMID: 20533514]
[6]
Miyawaki M. Constancy and characteristics of the anterior cutaneous branch of the first intercostal nerve: correcting the descriptions in human anatomy texts. Anatomical science international. 2006 Dec:81(4):225-41
[PubMed PMID: 17180761]
[7]
Wraight WM, Tweedie DJ, Parkin IG. Neurovascular anatomy and variation in the fourth, fifth, and sixth intercostal spaces in the mid-axillary line: a cadaveric study in respect of chest drain insertion. Clinical anatomy (New York, N.Y.). 2005 Jul:18(5):346-9
[PubMed PMID: 15971216]
[8]
Ueshima H, Hara E, Marui T, Otake H. RETRACTED: The ultrasound-guided transversus thoracic muscle plane block is effective for the median sternotomy. Journal of clinical anesthesia. 2016 Mar:29():83. doi: 10.1016/j.jclinane.2015.10.014. Epub 2016 Feb 9
[PubMed PMID: 26897453]
[9]
Fujii S, Vissa D, Ganapathy S, Johnson M, Zhou J. Transversus Thoracic Muscle Plane Block on a Cadaver With History of Coronary Artery Bypass Grafting. Regional anesthesia and pain medicine. 2017 Jul/Aug:42(4):535-537. doi: 10.1097/AAP.0000000000000607. Epub
[PubMed PMID: 28632672]
[10]
Jammes Y, Delpierre S. Respiratory and circulatory effects of parietal pleural afferent stimulation in rabbits. Journal of applied physiology (Bethesda, Md. : 1985). 2006 May:100(5):1539-46
[PubMed PMID: 16614364]