Introduction
Fascia is made up of sheets of connective tissue that is found below the skin. These tissues attach, stabilize, impart strength, maintain vessel patency, separate muscles, and enclose different organs. Traditionally, the word fascia was used primarily by surgeons to describe the dissectible tissue seen in the body encasing other organs, muscles, and bones. Recently, the definition has been broadened to include all collagenous based soft tissues in the body, including cells that create and maintain the extracellular matrix. The new definition also includes certain tendons, ligaments, bursae, endomysium, perimysium, and epimysium. [1]
Classification System
Fascia can be classified as superficial, deep, visceral, or parietal and further classified according to anatomical location. [2]
Superficial Fascia
Superficial fascia is found directly under the skin and superficial adipose layers. It can show stratification both grossly and microscopically. Traditionally, it is described as being made up of membranous layers with loosely packed interwoven collagen and elastic fibers.
- Superficial fascia is thicker in the trunk than in the limbs and becomes thinner peripherally.
- Superficial fascia layers can sometimes include muscle fibers to create all types of structures in the body. A few examples include the platysma muscle in the neck, the external anal sphincter, and the dartos fascia in the scrotum.
- A subtype of superficial fascia in the abdomen is Scarpa’s fascia.
Deep Fascia
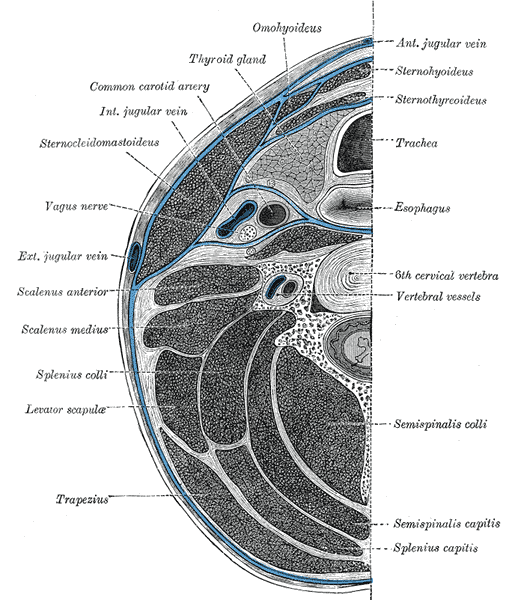
Deep fascia surrounds bones, muscles, nerves, and blood vessels. It is commonly has a more fibrous consistency and rich in hyaluronan as compared to the other subtypes. Deep fascia tends to be highly vascularized and contain well developed lymphatic channels. In some instances, deep fascia can even contain free encapsulated nerve endings, such as Ruffini and Pacinian corpuscles.
There are 2 subtypes of deep fascia:
Aponeurotic fascia
- It forms into sheets of pearly-white fibrous tissue to attach muscles needing a wide area of attachment. Aponeurosis can thin into a tendon and become a point of origin or insertion for other muscles. Some examples of aponeurotic fascia include the fascia of limbs, thoracolumbar fascia, and rectus sheath.
- It is the thicker of the 2 subtypes that are normally easily separated from the underlying muscle layer.
- It is comprised of 2 to 3 parallel collagen fiber bundles.
Epimysial fascia
- Also known as the epimysium, this is the connective tissue sheath surrounding skeletal muscle and can, in some cases, connect directly to the periosteum of bones.
- Some major muscle groups enveloped in epimysium include muscles of the trunk, pectoralis major, trapezius, deltoid, and gluteus maximus.
- It is the thinner of the 2 subtypes, on average, and is more tightly connected to the muscle via septa that penetrate the muscle layer.
Visceral Fascia
Visceral fascia surrounds organs in cavities like the abdomen, lung (pleura), and heart (pericardium).
Parietal Fascia
Parietal fascia is a general term for tissues that line the wall of a body cavity just outside of the parietal layer of serosa. The most commonly known parietal fascia is found in the pelvis.
In many places in the body, superficial and deep fascial layers are connected by fibrous septa and create a connection network that weaves in between fat lobules that make up the deep adipose tissue layer. [3]
Structure and Function
Fascia may appear passive structurally but are, in fact, active. They can provide support for surrounding tissues, help reduce friction, and play a supportive role for the tissues and organs. Fascia can transmit mechanical tension generated by muscular activity or external forces. The biomechanical regulatory system of the fascia is currently being studied further.
In a healthy state, fascia is a relaxed and wavy connective tissue that can lose its malleability when damaged via local trauma or inflammation. This can then cause fascial layers to tighten and restrict the movement of underlying tissues leading to pain, hindered range of motion, or decreased blood flow.
The distinct feature of fascia is that it possesses strength because it is tightly packed with bundles of collagen and wrapped tightly. The fibers are usually oriented in one direction so that the structure does not become loose or lax. Fascia is quite flexible and able to resist tension. The function of the fascia depends on its location.[4]
Embryology
The fascial system is classically understood to originate from the mesoderm layer divided during week 2 of development during the embryo's gastrulation phase. There is also some evidence that certain fascial layers, particularly in the cervical and cranial neck, derive from the ectoderm. [5]
Nerves
Sensory nerves innervate the fascial tissue. The deep fascia, specifically, is extensively innervated with multiple sensory nerve subtypes. This includes, but is not limited to, nociceptors, proprioceptors, mechanoreceptors, thermoreceptors, and chemoreceptors.
Surgical Considerations
Following a procedure, surgeons suture superficial fascia together to ensure that there is no weakness in the wound. If the suturing is not done correctly, the sutures can tear, resulting in wound dehiscence. If the patient is malnourished, suturing the fascia together can prove much more difficult, showing the importance of adequate nutrition pre-op. Wound dehiscence is a surgical emergency, and the diagnosis is usually clinical. [6]
Aponeurotic fascia (fascia lata) can be used as a surgical patch by plastic surgeons.[7]
In some cases, retaining ligaments of the face can be cut or released for aesthetic purposes.[8]
A new technique has gained traction in recent years called myofascial release. It is a form of noninvasive manual therapy usually provided by physical therapists. The goal is to use sustained pressure along with stretching techniques to restore optimal length, decrease pain, and improve the overall function of the treated area. It has also shown promise for post-operative orthopedic surgery patients.[9]
The Desarda technique is a surgical technique that sutures the aponeurosis of the external oblique to create a new posterior wall and result in a mesh-free, open, surgical treatment for inguinal hernias.
Clinical Significance
Compartment syndrome is a condition where the tissues within a fascial layer experience higher than normal pressures leading to pain, pallor, loss of pulses, and eventual paresthesias. Compartment syndrome can develop in morbidly obese patients or following crush injuries, severe burns, and impact injuries. Diagnosis can be confirmed by measuring the pressure within a fascial compartment with a pressure device, although clinical judgment is often used to determine the diagnosis. A compartment pressure of thirty mmHg or greater is pathognomonic for compartment syndrome. In patients who develop compartment syndrome, treatment regularly involves a fasciotomy. An urgent fasciotomy can be done at the bedside. A fasciotomy is a procedure where the compressing fascia is cut to relieve compartment pressure and allow the muscle to swell, decrease pressure, and restore blood flow and nerve function. [10][11][12]
Plantar fasciopathy, or plantar fasciitis, is a common health concern in the general population resulting in inferior heel pain. Patients can receive non-invasive therapies such as physical therapy, orthosis, NSAIDs, radiation therapy, or shockwave therapy to help relieve symptoms. Invasive treatments include local corticosteroid injections, botulinum injection, platelet-rich plasma injection, and surgery. [13]
Necrotizing fasciitis is a rare and sometimes fatal soft-tissue infection that is a medical and surgical emergency. It is the resulting condition of inflammation and necrosis at multiple layers including fascia, muscle, subcutaneous fat, and subsequent necrosis of overlying skin. Emergency radical debridement of the necrotic tissues is the standard mandatory procedure. [14]