Continuing Education Activity
Oral candidiasis is an infection of the oral cavity by Candida albicans. The condition is generally obtained secondary to immune suppression, which can be local or systemic, including extremes of age (newborns and elderly), immunocompromising diseases such as HIV/AIDS, and chronic systemic steroid and antibiotic use. This activity illustrates the evaluation and treatment of oral candidiasis. It highlights the role of the interprofessional team in evaluating and treating patients with this condition; it describes the disease's original discovery, epidemiology, and pathophysiology and reviews how a clinician should approach a patient with potential oral candidiasis, including history taking, physical examination, evaluation, differential diagnosis, and appropriate treatment.
Objectives:
- Identify the etiology of oral candidiasis.
- Review the presentation of the different types of oral candidiasis and their evaluation.
- Explain the treatment and management options available for oral candidiasis.
- Identify the differential diagnosis, prognosis, and possible complications of oral candidiasis.
Introduction
Oral candidiasis is an infection of the oral cavity by Candida albicans, first described in 1838 by pediatrician Francois Veilleux. The condition is generally obtained secondary to immune suppression, which can be local or systemic, including extremes of age (newborns and elderly), immunocompromising diseases such as HIV/AIDS, and chronic systemic steroid and antibiotic use.[1][2] An example of local immunosuppression is inhaled corticosteroids, often prescribed in the preventive treatment of asthma and chronic obstructive pulmonary disease.
Even though acute pseudomembranous candidiasis, also known as thrush, is the most common form of oral candidiasis, it is important to recognize that other types of oral candidiasis exist and that candidal infection can present as white and erythematous lesions. White lesions include acute pseudomembranous candidiasis and chronic hyperplastic candidiasis; red lesions include acute and chronic erythematous candidiasis, angular cheilitis, median rhomboid glossitis, and linear gingival erythema.[3] Other rare oral types not included in these categories are cheilocandidiasis, chronic mucocutaneous candidiasis, and chronic multifocal candidiasis.[3] However, such types are beyond the scope of this article.
Diagnosis of oral candidiasis is often clinical, based on clinical examination, medical history taking, and assessment of risk factors. A biopsy is recommended for certain types in addition to empirical treatment.[4] Cultures are usually done if antifungal treatment is ineffective.[4] Topical antifungal therapy and oral hygiene measures are generally sufficient to resolve mild oral candidiasis,[4] and systemic antifungal therapy is usually reserved for patients who are refractory or intolerant to topical treatment and those at increased risk of developing systemic infections.[4]
Etiology
Candida species cause oral candidiasis, most commonly Candida albicans, isolated from more than 80% of lesions.[3] Candida albicans is a dysmorphic yeast that can present as both hyphal and yeast forms depending on the environment.[3]
Although much less common, other implicated species include Candida glabrata, Candida tropicalis, Candida kruesi, Candida guillermondii, Candida lusitaniae, Candida parapsilosis, Candida pseudotropicalis, and Candida stellatoidea.[5] Non-albicans Candida species have been shown to colonize patients 80 years old and above more frequently than younger patients.[6]
Candida is part of the normal oral microflora of immunocompetent individuals.[3] Around 30 to 60% of adults and 45 to 65% of infants carry candida species in their oral cavities.[5][3][5] Most of these species live in the oral cavity as a commensal population rather than a pathological one.[5]
Risk factors for the pathologic colonization of Candida include but are not limited to malnourishment, age extremes (young children and elderly), metabolic disease, immunocompromising conditions, concomitant infections, radiation therapy, organ transplantation, long-term steroid treatment, antibiotic treatment, and salivary gland hypofunction.[5]
Epidemiology
Oral candidiasis can occur in immunocompetent or immunocompromised patients but is more common in immunocompromised hosts. More than 90% of patients with HIV develop oral candidiasis at some point during the duration of the disease.[7]
Oral candidiasis occurs equally in males and females. It typically occurs in neonates and infants; it is rare in the first week of life. It is most common during the fourth week of life and less common in infants older than six months, likely secondary to the development of host immunity. Signs and symptoms of immunosuppression in these patients are diarrhea, rashes, repeated infections, and hepatosplenomegaly.
Pathophysiology
Candidal species cause oral candidiasis when a patient's host immunity becomes disrupted. This disruption can be local, secondary to oral corticosteroid use. Overgrowth of the fungus then leads to the formation of a pseudomembrane. Vaginal infections can colonize neonates as they pass through the birth canal. Alternatively, neonates and infants may contract the disease through colonized breasts when breastfeeding. A patient's oral Candida infection can often lead to GI involvement and subsequent candidal diaper dermatitis. Candidal species thrive in moist environments. As such, females can develop vaginal candidiasis as well.
In healthy patients, the patient's immune system and normal bacteria flora inhibit candida growth. Consequently, immunosuppression such as diabetes, dentures, steroid use, malnutrition, vitamin deficiencies, and recent antibiotic use often leads to the disease.
Histopathology
Oral candidiasis is a clinical diagnosis. Further evaluation is necessary when a differential diagnosis is required and for cases resistant to antifungal therapy.[8] However, a biopsy is indicated for chronic hyperplastic candidiasis due to its risk of malignant transformation.[8] The commonly implemented methods for identifying Candida are 10% potassium hydroxide stain and culture with sabouraud dextrose agar.[8] Differentiation of specific species is possible with special culture mediums like Chromagar Candida.[9] ELISA and PCR tests are used in cases of invasive candidiasis and to differentiate Candida dubliniensis from Candida albicans.[8]
History and Physical
Pseudomembranous candidiasis, also known as oral thrush, is the classic and most common presentation of oral candidiasis, but several other types exist. Candidiasis can appear in the oral cavity as white or erythematous lesions.[3] White lesions develop as pseudomembranous or hyperplastic lesions; erythematous lesions include atrophic lesions in acute and chronic forms, angular cheilitis, median rhomboid glossitis, and linear gingival erythema.[3] Other rare oral types that cannot be included in these categories are cheilocandidiasis, chronic mucocutaneous candidiasis, and chronic multifocal candidiasis.[3]
Acute Pseudomembranous Candidiasis
Pseudomembranous candidiasis is the most frequently encountered oral candidiasis, accounting for a third of cases.[3] It is most commonly seen in newborns and immunocompromised patients,[5] but the elderly are also susceptible.[3] Other risk factors include topical steroids use in the form of inhalers, gels, or rinses and decreased salivary flow.[5]
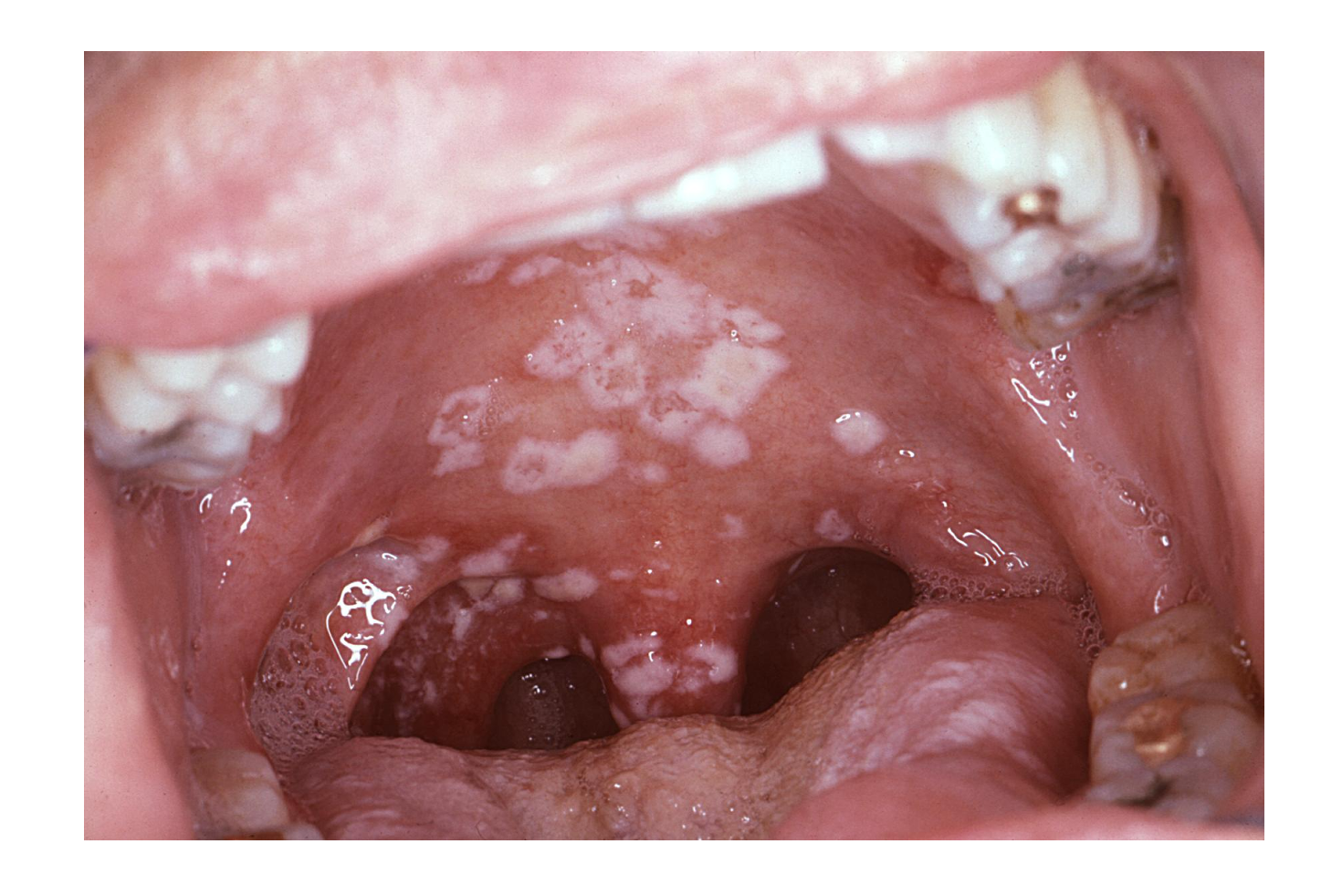
It typically presents with extensive white patches that can be easily removed with gauze, leaving an erythematous mucosa surface.[3] The pseudomembrane is formed by desquamated epithelial cells, fibrin, and fungal hyphae.[4] The lesions are usually asymptomatic and appear on the tongue, labial and buccal mucosa, gingival tissues, hard and soft palate, and oropharynx.[4] If symptomatic, patients report a burning sensation in the mouth, oral bleeding, and changes in taste perception.[3]
Hyperplastic Candidiasis
Hyperplastic candidiasis presents as slightly raised and well-circumscribed white plaques, usually on the buccal mucosa, which may extend to the labial commissures.[3] The lesions may also be nodular or spotted.[3] Unlike oral thrush, hyperplastic candidiasis cannot be easily wiped off.[3] Smoking seems to be linked to the development of the lesion, and smoking cessation is required for complete resolution.[4]
Hyperplastic candidiasis has the potential to evolve into severe dysplasia or malignancy.[4] Candida involvement in leucoplakia lesions has been shown to increase the risk of malignancy compared to non-candidal leucoplakias.[3]
Acute Atrophic Candidiasis
Acute atrophic candidiasis presents as a generalized or localized erythema on the oral mucosa,[5] most commonly on the palate. Still, it may also develop on the buccal mucosa and tongue's dorsum.[3] Atrophy of tongue papillae may accompany the erythema.[3] Patients usually seek consultation due to a burning sensation in the mouth or tongue.[4] Therefore, it should be included in the differential diagnosis of a sore tongue.[4]
Acute atrophic candidiasis is frequently secondary to treatment with broad-spectrum antibiotics.[3] However, other risk factors have been described, including corticosteroids, HIV disease, iron deficiency anemia, vitamin B12 deficiency, and uncontrolled diabetes mellitus.[3]
Chronic Atrophic Candidiasis
Chronic atrophic candidiasis, also known as denture stomatitis, is localized erythema of the oral mucosa under dentures.[4] It is a common condition, with an incidence of up to 65%.[4] It may sometimes be seen in relation to orthodontics appliances.[5] Risk factors mainly include poorly fitted dentures,[3] prolonged use of dentures – patients that wear their dentures for 24 hours- and poor oral hygiene.[5]
Lesions are typically edematous and erythematous and limited to the area in contact with the denture.[3] Angular cheilitis is usually found simultaneously with chronic atrophic candidiasis.[3]
The clinical aspect of denture stomatitis can be classified into three types. In type I, there is petechial hemorrhage and local inflammation; in type II, there is erythema of the mucosa under the dentures; in type III, there is erythema of the central area of the hard palate or papillary hyperplasia of the oral mucosa under the denture.[3]
The condition is often asymptomatic, but patients may report a sore mouth or oral burning.[3]
Median Rhomboid Glossitis
Median rhomboid glossitis is a very rare type of oral candidiasis, occurring in less than 1% of the population.[10] It presents as a rhomboid-shaped erythematous patch in the center of the tongue's dorsum anterior to the circumvallate papillae.[3] The appearance of the lesion results from the atrophy of the filiform papillae.[4] Smoking and inhaled steroids are associated with the condition.[4]
A concomitant erythematous lesion can develop on the palate directly opposite the tongue's lesion, known as a "kissing" lesion, which frequently signifies immunosuppression. The kissing lesion is a potential HIV marker, and further investigations should be performed.[11]
Angular Cheilitis
Angular cheilitis presents as erythematous fissured patches in one or both commissures of the mouth, but it is typically bilateral.[4][3] The lesions are usually painful and sore. A moist environment due to the accumulation of saliva in the corners of the mouth favors Candida growth. But, bacteria, including Staphylococcus aureus and streptococcal species, are also isolated from the lesions.[12] Wearing dentures, licking the lips, biting the commissures, and facial wrinkling at the commissures and along the nasolabial fold contribute to the accumulation of saliva; hence, chronically moist commissures and angular cheilitis.[3] Other factors linked to the etiology of angular cheilitis include iron, folic acid, thiamine, riboflavin, and vitamin B12 deficiencies.[3]
Linear Gingival Erythema
Linear gingival erythema is typically seen in HIV patients and may even reveal how the disease progresses.[3] However, the condition can also develop in healthy children.[3] Clinically, the lesion presents as an erythematous line or band over the gingival margins of one or more teeth.[13] Candida and bacterial infections participate in its development.[3]
Evaluation
Diagnosis of oral candidiasis is often clinical, based on clinical examination, medical history taking, and assessment of risk factors. The diagnosis is made after finding the typical lesion's features, excluding other conditions, and assessing the lesion's response to antifungal treatment.[4] Acute atrophic candidiasis and chronic hyperplastic candidiasis resemble premalignant or malignant lesions; therefore, a biopsy is recommended on top of the empirical treatment.[4]
Cultures and sensitivity tests can be done if antifungal treatment is ineffective.[4] Several methods have been developed to obtain a sample from the oral cavity to identify Candida species. The selection of the method mostly depends on the clinical findings. If visible lesions can be identified, taking a swab with a plain microbial swab or an imprint with a sterile foam pad is recommended.[12] If no specific lesion is identified, but a Candida infection is suspected, collecting a whole saliva sample in a sterile container or the oral rinse technique is advised.[12] If denture stomatitis is suspected, a sample should be obtained from both the internal surface of the denture and palatal mucosa, as sampling from the oral mucosa alone may be negative.[12]
In addition to confirming candidiasis, testing to diagnose an underlying immunocompromising condition should be considered. Patients may be tested for diseases such as HIV, adrenal insufficiency, malnutrition, steroid use, and diabetes mellitus.
Treatment / Management
Treatment focuses on Candida species. It should be targeted to the extent of the patient's involvement and degree of immunosuppression. Topical antifungal therapy is the first-line therapy for uncomplicated cases of oral candidiasis and should continue simultaneously when systemic treatment is indicated.[4] Systemic antifungal therapy is usually reserved for patients who are refractory to topical treatment, those who are intolerant to topical therapy, and those at increased risk of developing systemic infections.[4]
Topical antifungal therapy and oral hygiene measures are usually sufficient to resolve mild oral candidiasis. Topical antifungal drugs available include nystatin, miconazole, clotrimazole, and ketoconazole.[4] The use of miconazole in the mouth is limited since it induces vomiting and diarrhea.[4] However, it is prescribed to manage angular cheilitis and denture stomatitis.[12] Nystatin is a widely used topical antifungal for treating oral candidiasis, available as pastille, mouth wash, and oral suspension.[4] Patients are indicated to rinse their mouth with topical nystatin four times daily for two weeks. Its adverse effects most commonly include nausea, vomiting, and diarrhea.[4]
Nystatin (oral rinse) and clotrimazole (troches) are high in sucrose. Therefore, triazoles - fluconazole or itraconazole – prescribed once daily can be an alternative [14] in oral candidiasis associated with diabetes mellitus or if there is a high risk of dental caries.[4]
Topical treatment is recommended for patients with a mild presentation or first presentation of the disease. One option is clotrimazole troches 10 mg orally five times daily (dissolved over 20 minutes). Another is nystatin oral suspension (100000 units/mL) 5 mL orally four times daily (swished for several minutes then swallowed).[15][16] In the appropriate circumstances, miconazole oral gel may also be an option.[17]
For moderate to severe disease, fluconazole 200 mg orally once, then 100 mg orally once daily for 7 to 14 days, is recommended. Data regarding the safety of fluconazole during breastfeeding is reassuring.[18]
For refractory disease, options are itraconazole oral solution 200 mg once daily without food for 28 days, posaconazole suspension 400 mg orally twice daily for three days, then 400 mg orally daily for a total of 28 days, and voriconazole 200 mg orally two times daily for 28 days.
Additionally, single-dose oral fluconazole 150 mg has shown to be effective in patients with advanced cancer, thus helping reduce pill burden.[19]
Oral azoles are teratogenic and should not be used to treat mucosal candidiasis during the first trimester. Clotrimazole troches, nystatin swish and swallow topical therapies, and miconazole buccal tablets are also treatment options.
Dosing for these regimens should be adjusted according to weight for pediatric patients.
In addition to treatment, patients should receive counseling on decreasing immunosuppressing conditions such as uncontrolled diabetes mellitus, smoking, and malnutrition.
Management of Dentures
Denture hygiene is particularly important in treating denture stomatitis; however, it must be indicated in managing all forms of oral candidiasis to eradicate the Candida colonization from dentures, which acts as a reservoir.[12]
- Patients must clean and disinfect their dentures daily and remove them for at least six hours every night.[4]
- Dentures should be soaked in chlorhexidine and allowed to dry, as air also kills Candida adhered to dentures.[4] Hypochlorite can be used instead of chlorhexidine in dentures with no metallic components.[12]
- Dentures must be taken out every time an antifungal rinse is used and, in established cases of chronic atrophic candidiasis, soaked in chlorhexidine before placing them back in the mouth.[4]
- In denture stomatitis cases, patients should be recommended to apply topical miconazole to the dentures' internal surface and place them back in the mouth.[12]
- Mixing an antifungal agent with a denture liner is recommended for denture wearers that cannot hold antifungal rinse in their mouth for long enough.[4]
- Nystatin and chlorhexidine digluconate combination inactivates both; hence, it is contraindicated.[4]
Specific Considerations
Acute Pseudomembranous Candidiasis in Infants
The management of acute pseudomembranous candidiasis in breastfed infants includes topical antifungals for the infant and the mother's nipples, even if the mother does not show signs of involvement. A systemic antifungal, typically fluconazole, is prescribed to the mother in addition to topical treatment if the nipples show symptoms of thrush.[20] Nystatin oral suspension is applied to the infant's oral lesion [21] and miconazole 2% cream to the mother's nipples. It is worth noting that miconazole 2% cream is an off-label indication to treat oral candidiasis in breastfeeding women.
Acute Erythematous Candidiasis
Most cases of acute erythematous candidiasis are secondary to antibiotic therapy; stopping the antibiotic treatment usually resolves the candidiasis without intervention.[12] Alternatively, if symptoms are more severe systemic fluconazole 50 mg once daily for one week can be indicated.[12]
Angular Cheilitis
The treatment of angular cheilitis includes antifungal and steroid creams.[4] Miconazole cream is recommended, and treatment should continue for ten more days after the complete resolution of lesions. Miconazole cream can be indicated alone or in its combined formulation with hydrocortisone.[12] Concomitant oral lesions must be simultaneously treated.[4] Dietary deficiencies must also be resolved.[4]
Staphylococci aureus reservoir is in the nostrils;[4] therefore, applying mupirocin cream to the anterior nares aids in eliminating this niche.
Chronic Hyperplastic Candidiasis
The treatment of chronic hyperplastic candidiasis includes fluconazole 50 mg daily for seven to fourteen days, depending on the extent of the lesion, and smoking cessation.[12] Patients must be aware of malignant transformation risk.[12]
In suspected cases of chronic hyperplastic candidiasis, prescribing systemic antifungal treatment for seven days before taking a biopsy has been shown to help identify true dysplasia rather than dysplasia caused by the presence of Candida.[12]
Linear Gingival Erythema
Debridement, chlorhexidine mouthwash, and ensuring patients receive appropriate antiretroviral treatment are included in the management of linear gingival erythema in addition to antifungal therapy.
Differential Diagnosis
The differential diagnosis of erythematous forms of oral candidiasis includes oral mucositis, erythroplakia, thermal burns, erythema migrans, and anemia.[22] Chronic hyperplastic candidiasis may be confused with leukoplakia,[22] lichen planus, pemphigoid, pemphigus, and oral squamous cell carcinoma (OSCC).[4]
Other conditions included in the differential diagnosis of oral candidiasis are oral hairy leukoplakia (a condition triggered by the Ebstein-Barr virus), angioedema, aphthous stomatitis, herpes gingivostomatitis, herpes labialis, measles (Koplik spots), perioral dermatitis, Steven-Johnsons syndrome, histiocytosis, blastomycosis, lymphohistiocytosis, diphtheria, esophagitis, syphilis, and streptococcal pharyngitis.
Prognosis
The prognosis for oral candidiasis is quite good when receiving appropriate and effective treatment. When patients relapse, it is usually due to poor patient compliance with therapy, the failure to appropriately remove and clean dentures, or the inability to resolve any underlying or predisposing factors to infection.[23]
Complications
Although unlikely in an immunocompetent host, oral candidiasis can lead to pharyngeal involvement, which presents as dysphagia and respiratory distress. A significant concern for immunocompromised patients is the systemic dissemination of the disease. Candidal esophagitis is a prevalent complication of oral candidiasis in those with HIV/AIDS.
Deterrence and Patient Education
Patients with oral candidiasis should receive counseling regarding the future spread of the disease. They must also understand the importance of diagnosing and treating any immunosuppressive conditions.
- Patients using steroid inhalers must be advised to rinse their mouth with water every time after application.[12]
- Oral candidiasis has been linked to malnutrition, iron, and vitamin deficiency; patients must be advised on appropriate nutrition.[3]
- Patients must receive appropriate advice regarding dentures and dental hygiene, which can prevent the development of oral candidiasis.
- High sugar intake favors the multiplication of Candida; reducing sugar intake may be advised.
Enhancing Healthcare Team Outcomes
Candida species are found in the oral cavity of immunocompetent individuals as a commensal population, and a shift to pathological activity is triggered by a decrease in the host's immunity, e.g., extremes of age, immunocompromising diseases, long-term steroids, and antibiotic treatment.[3][5] It is essential to emphasize that oral candidiasis is not a single entity; it does not only present as acute pseudomembranous candidiasis, commonly known as oral thrush, but erythematous forms also exist.
Each type of oral candidiasis has a different clinical presentation, so the efforts of an interprofessional healthcare team are beneficial in such cases. Patients may be asymptomatic and unaware of the infection or report oral burning, discomfort, and changes in taste. The diagnosis of oral candidiasis is based on history taking, assessment of risk factors, and clinical examination, and further evaluation is usually indicated for refractory cases. General practitioners and dentists are usually the ones who diagnose and treat cases of oral candidiasis. Pediatricians also play a crucial role in managing cases in neonates and infants, who commonly develop oral thrush.[5] In addition, in breastfeeding infants, mothers must also receive treatment, and nurses can participate in identifying symptoms of thrush in this group. All interprofessional team members, including dental nurses, must provide oral and denture hygiene instructions for all types of oral candidiasis but particularly for those directly linked to the use of dentures, and document all observations and interactions in the patient's healthcare record, so everyone on the team has access to the same data.[20][12]
Depending on the underlying immunosuppressing condition, oncologists and infectious disease specialists may provide consultations. As oral candidiasis is often the first sign of a systemic immunocompromising condition, referring patients with suspected or diagnosed underlying conditions to the appropriate specialist is crucial. The pharmacist should educate the patient on the importance of medication compliance, verify medication dosing, check for drug-drug interactions, and report any concerns to the healthcare team. Patients with diabetes mellitus should be urged to monitor their blood sugar levels. Also, the patient should receive instructions to quit smoking. Patients who take inhaled steroids should be asked to perform water gargles after each use and follow up with the clinician. Nurses administer medications for inpatients and provide significant counseling to reinforce the points above. Only with an interprofessional collaborative team approach with open communication between team members can oral candidiasis treatment achieve optimal patient results. [Level 5]