Introduction
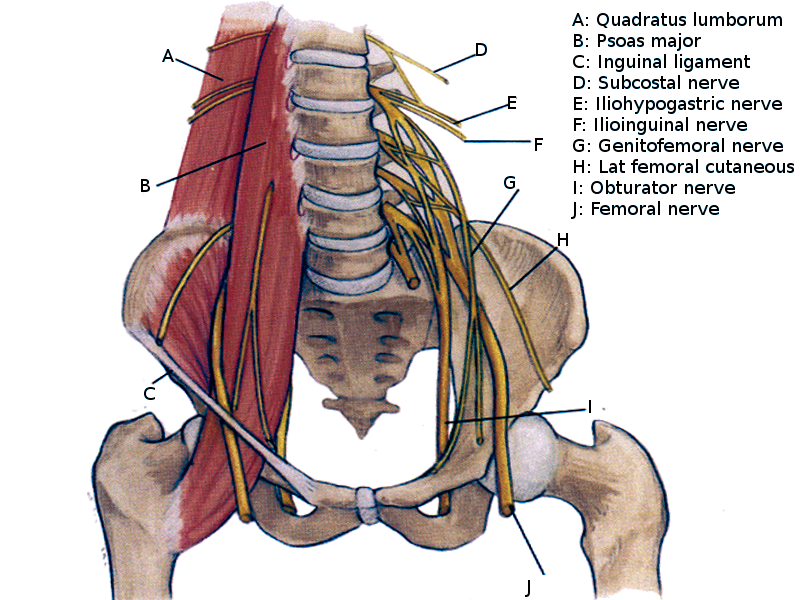
The lumbar plexus is an essential collection of nerves that arise from mostly the lumbar spinal cord. The term plexus refers to a “web” of nerves that is created just lateral to where T12-L5 exit the spinal cord via intervertebral foramina. The plexus exists bilaterally and allows nerves to combine with different levels to create multiple functioning nerves that serve to innervate various structures. This type of nerve web is significant for the formation of larger, longer nerves that target peripheral tissues that altogether primarily help to innervate the portions of lower extremities. The primary functions of these nerves are motor innervation and sensory nerves to the skin mainly in the lower extremities, although the superior nerves in the plexus do contribute to the lower abdomen and pelvis. The nerves arising from the lumbar plexus are vital for the functioning of the lower extremity and maintaining the ability to extend the knee, flex the hip, adduct the thigh, and more.
Embryology
The spinal cord forms from the neural plate. Peripheral nerves derive from neuroepithelial cells. These nerves help create the neurons, support cells, and axons that contribute to the peripheral nervous system.[1] These are important in the creation of peripheral nervous structures such as the lumbar plexus.
Morphology remains similar when comparing structures from a fetal lumbar plexus to an adult lumbar plexus. Specifically, nerve thickness, length, and spinal nerve branching are observed to remain the same throughout development.[2]
Blood Supply and Lymphatics
Blood supply to the lumbar plexus is complex. The plexus embeds itself in the posterior aspect of the psoas major muscle. Due to this anatomical relation to a large muscle, it can share its blood supply. The primary blood supply of the plexus comes from the lumbar branch of the iliolumbar artery, a branch of the internal iliac artery. The lumbar plexus has protection from ischemic damage due to multiple collateral arterial systems that it receives from small arteries of the psoas muscle. Therefore, ischemic injury to this area during aortoiliac surgery is uncommon.[3]
Nerves
The nerves arising from the lumbar plexus from superior to inferior are iliohypogastric, ilioinguinal, genitofemoral, lateral femoral cutaneous, femoral nerve, obturator, and nerve to the lumbosacral trunk.
The iliohypogastric nerve is created from spinal levels T12 and L1. It has motor innervation to the internal oblique muscle and the transverse abdominal muscles. Its sensory inputs are to the lateral gluteal area.
The ilioinguinal nerve derives from a branch of the L1 spinal nerve. It provides sensory inputs to the anterior superior and medial parts of the thigh. In males, the distal portions of the nerve become the anterior scrotal nerve that inputs sensory fibers to the root of the penis and the superior part of the scrotum. In females, the distal portions of the nerve are the anterior labial nerves that help to provide sensory inputs to the skin covering the mons pubis and the labia majora. It also provides some motor inputs to the internal oblique muscle and the transverse abdominal muscles.
The genitofemoral nerves arise from the superior aspects of L1 and L2 spinal nerves. The nerve separates into the genital and the femoral branch. The genital branch supplies the cremaster muscle and scrotal skin in men and supplies sensory to the mons pubis and the labia majora in women. The genitofemoral nerve's femoral branch provides sensory innervation the anterior, superior area of the thigh.
The lateral femoral cutaneous nerve comes from the L2 and L3 spinal nerves. It serves the singular function of supplying sensory innervation to much of the lateral portion of the thigh.
The femoral nerve ranks as the largest nerve that arises from the lumbar plexus. It is created from lumbar spinal nerves L2, L3, and L4. Its principal function is to supply motor and sensory innervation to the anterior compartment of the thigh. The nerve exits the plexus and enters the femoral triangle, passing just lateral to the femoral artery. The nerve has four major branches: muscular (motor), cutaneous, articular, and vascular. The motor branch supplies the muscles quadriceps femoris, sartorius, and articularis genu. The cutaneous branch is the primary sensory supply to the anterior thigh. A portion of the cutaneous branch become the saphenous nerve, which provides sensation the skin overlying the patella, and portions of the medial and anterior aspects of the distal lower extremity. The articular branch plays an essential role in the proprioceptive sensation of the knee. The vascular branch supplies the femoral artery and its smaller branches.
The obturator nerve arises from L2, L3, and L4 spinal nerves. It provides the primary motor supply to the medial (adductor) muscle compartment of the thigh. These muscles include external obturator, adductor longus, adductor brevis, adductor magnus, gracilis, and pectineus. It also has a sensory component that supplies the medial thigh that is inferior to the area supplied by the ilioinguinal nerve.
Muscles
The lumbar plexus provides innervation to several important muscles. Notable muscles include the psoas muscle, quadratus lumborum, lumbar transverse muscles, quadriceps femoris, transversus abdominis, and internal oblique muscles. Nerves that arise directly from the plexus are responsible for innervation to the psoas muscles, quadratus lumborum, and lumbar transverse muscles. The rest of the muscles receive innervation from nerves that form after exiting the lumbar plexus.
The innervation supplied to the quadriceps is necessary for the proprioception of the hip and knee. Innervation to the vastus lateralis, vastus intermedius, and the vastus medialis help provide proprioceptive information about the knee to the central nervous system. Innervation of the rectus femoris helps provide proprioceptive information to the central nervous about the hip.
Surgical Considerations
The lumbar plexus and its derivatives are essential to consider when performing surgery. An anterior abdominal approach surgery can result in iatrogenic injury to superficial branches of either the iliohypogastric nerve, ilioinguinal nerves, or genitofemoral nerve. Injury to these during surgery can result in paresthesias. Of these, the genitofemoral nerve is most difficult to identify intraoperatively.[4] Additionally, damage to the lumbar plexus is a well-documented iatrogenic injury following a minimally invasive lateral retroperitoneal transpsoas approach.[5] This injury to the lumbar plexus most commonly causes neuropraxia, with recovery within 3 months.[5]
It is crucial to note the use of nerve blocks to the ilioinguinal nerve, Iliohypogastric nerve, and genitofemoral nerve are considerations in the management of treatment-resistant groin pain, as well as surgery to this area.[6] Ultrasound-guided erector spinae block is more effective than ultrasound-guided ilioinguinal/ iliohypogastric blocks have in children requiring inguinal hernia surgery.[7] An ilioinguinal transversus abdominal plane nerve block has shown to provide more effective analgesia to patients undergoing an elective cesarean section.[8]
In joint surgery of either the hip or the knee can result in proprioceptive impairment.[9] Innervation to the musculature surrounding the joint, as well as innervation to the joint itself is vital for proprioceptive information sent to the central nervous system. It is important to consider this aspect of joint when planning rehabilitation techniques for patients status post hip or knee arthroplasty.[9]
Clinical Significance
Damage to the lumbar plexus or nerves proximal and distal to it can result in several pathologies. Lumbar disc herniation can result in occlusion of the intervertebral foramen, which can compress lumbar spinal nerves proximal to their entrance to the lumbar plexus. This condition can result in paresthesia and weakness of the areas innervated by nerves of the lumbar plexus. Commonly, peripheral nerves and the lumbar plexus can suffer damage due to trauma.[10]
An important reflex to note is the cremasteric reflex. The femoral portion of the genitofemoral nerve and the ilioinguinal nerve provide the afferent fibers for this reflex. The genital branch of the genitofemoral nerve supplies motor innervation to the cremaster muscle is responsible for the efferent. As the afferent portion is the sensory aspect, stroking the medial thigh should cause contraction of the cremasteric muscle result in the ascension of the scrotum. In patients with testicular torsion, the genital branch of the genitofemoral nerve will become entrapped, and this reflex will be absent.[11]
A common and significant nerve compression syndrome can arise from the lateral femoral cutaneous nerve, which is a branch of the lumbar plexus. This syndrome is called meralgia paresthetica and is caused usually by entrapment of the nerve as it passes under, or through the inguinal ligament.[12] This condition can present as a painful syndrome involving the anterolateral area of the thigh. Non-steroidal anti-inflammatory drugs (NSAIDs), narcotics, and anti-neuropathic pain medications can be used to treat this condition; however, if the patient remains symptomatic surgical decompression can be a consideration.[12]