[2]
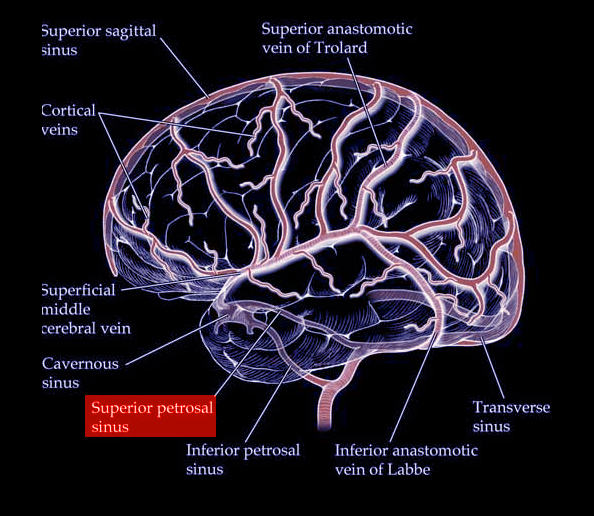
Mortazavi MM, Cox MA, Saker E, Krishnamurthy S, Verma K, Griessenauer CJ, Loukas M, Oskouian RJ, Tubbs RS. The superior petrosal sinus: a review of anatomy, embryology, pathology, and neurosurgical relevance. Neurosurgical review. 2018 Jul:41(3):713-718. doi: 10.1007/s10143-016-0785-9. Epub 2016 Sep 19
[PubMed PMID: 27647276]
[3]
BUTLER H. The development of certain human dural venous sinuses. Journal of anatomy. 1957 Oct:91(4):510-26
[PubMed PMID: 13475149]
[4]
PADGET DH. The cranial venous system in man in reference to development, adult configuration, and relation to the arteries. The American journal of anatomy. 1956 May:98(3):307-55
[PubMed PMID: 13362118]
[5]
Tanriover N, Abe H, Rhoton AL Jr, Kawashima M, Sanus GZ, Akar Z. Microsurgical anatomy of the superior petrosal venous complex: new classifications and implications for subtemporal transtentorial and retrosigmoid suprameatal approaches. Journal of neurosurgery. 2007 Jun:106(6):1041-50
[PubMed PMID: 17564177]
[7]
Miyamoto N, Naito I, Takatama S, Shimizu T, Iwai T, Shimaguchi H. Clinical and angiographic characteristics of cavernous sinus dural arteriovenous fistulas manifesting as venous infarction and/or intracranial hemorrhage. Neuroradiology. 2009 Jan:51(1):53-60. doi: 10.1007/s00234-008-0468-5. Epub 2008 Oct 25
[PubMed PMID: 18953532]
[8]
Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. Journal of neurosurgery. 1995 Feb:82(2):166-79
[PubMed PMID: 7815143]
[9]
Ng PP, Halbach VV, Quinn R, Balousek P, Caragine LP, Dowd CF, Higashida RT, Wilson C. Endovascular treatment for dural arteriovenous fistulae of the superior petrosal sinus. Neurosurgery. 2003 Jul:53(1):25-32; discussion 32-3
[PubMed PMID: 12823870]
[10]
Link MJ, Coffey RJ, Nichols DA, Gorman DA. The role of radiosurgery and particulate embolization in the treatment of dural arteriovenous fistulas. Journal of neurosurgery. 1996 May:84(5):804-9
[PubMed PMID: 8622154]