[1]
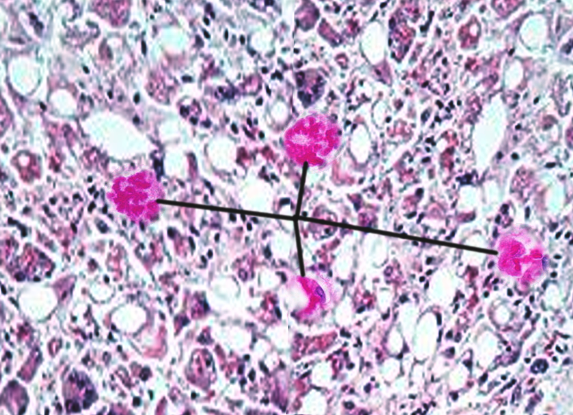
Zatloukal K, French SW, Stumptner C, Strnad P, Harada M, Toivola DM, Cadrin M, Omary MB. From Mallory to Mallory-Denk bodies: what, how and why? Experimental cell research. 2007 Jun 10:313(10):2033-49
[PubMed PMID: 17531973]
[2]
Aishima S, Fujita N, Mano Y, Iguchi T, Taketomi A, Maehara Y, Oda Y, Tsuneyoshi M. p62+ Hyaline inclusions in intrahepatic cholangiocarcinoma associated with viral hepatitis or alcoholic liver disease. American journal of clinical pathology. 2010 Sep:134(3):457-65. doi: 10.1309/AJCP53YVVJCNDZIR. Epub
[PubMed PMID: 20716803]
[3]
Afifiyan N, Tillman B, French BA, Sweeny O, Masouminia M, Samadzadeh S, French SW. The role of Tec kinase signaling pathways in the development of Mallory Denk Bodies in balloon cells in alcoholic hepatitis. Experimental and molecular pathology. 2017 Oct:103(2):191-199. doi: 10.1016/j.yexmp.2017.09.001. Epub 2017 Sep 19
[PubMed PMID: 28935395]
[4]
Basaranoglu M, Turhan N, Sonsuz A, Basaranoglu G. Mallory-Denk Bodies in chronic hepatitis. World journal of gastroenterology. 2011 May 7:17(17):2172-7. doi: 10.3748/wjg.v17.i17.2172. Epub
[PubMed PMID: 21633525]
[5]
French SW, Mendoza AS, Peng Y. The mechanisms of Mallory-Denk body formation are similar to the formation of aggresomes in Alzheimer's disease and other neurodegenerative disorders. Experimental and molecular pathology. 2016 Jun:100(3):426-33. doi: 10.1016/j.yexmp.2016.03.010. Epub 2016 Apr 9
[PubMed PMID: 27068270]
[6]
Golob-Schwarzl N, Bettermann K, Mehta AK, Kessler SM, Unterluggauer J, Krassnig S, Kojima K, Chen X, Hoshida Y, Bardeesy NM, Müller H, Svendova V, Schimek MG, Diwoky C, Lipfert A, Mahajan V, Stumptner C, Thüringer A, Fröhlich LF, Stojakovic T, Nilsson KPR, Kolbe T, Rülicke T, Magin TM, Strnad P, Kiemer AK, Moriggl R, Haybaeck J. High Keratin 8/18 Ratio Predicts Aggressive Hepatocellular Cancer Phenotype. Translational oncology. 2019 Feb:12(2):256-268. doi: 10.1016/j.tranon.2018.10.010. Epub 2018 Nov 12
[PubMed PMID: 30439626]
[7]
French SW, Bardag-Gorce F, Li J, French BA, Oliva J. Mallory-Denk body pathogenesis revisited. World journal of hepatology. 2010 Aug 27:2(8):295-301. doi: 10.4254/wjh.v2.i8.295. Epub
[PubMed PMID: 21161012]
[8]
Mahajan V, Klingstedt T, Simon R, Nilsson KP, Thueringer A, Kashofer K, Haybaeck J, Denk H, Abuja PM, Zatloukal K. Cross β-sheet conformation of keratin 8 is a specific feature of Mallory-Denk bodies compared with other hepatocyte inclusions. Gastroenterology. 2011 Sep:141(3):1080-1090.e1-7. doi: 10.1053/j.gastro.2011.05.039. Epub 2011 May 27
[PubMed PMID: 21699779]
[9]
Aigelsreiter A, Neumann J, Pichler M, Halasz J, Zatloukal K, Berghold A, Douschan P, Rainer F, Stauber R, Haybaeck J, Denk H, Lackner C. Hepatocellular carcinomas with intracellular hyaline bodies have a poor prognosis. Liver international : official journal of the International Association for the Study of the Liver. 2017 Apr:37(4):600-610. doi: 10.1111/liv.13325. Epub 2017 Jan 12
[PubMed PMID: 27885796]
[11]
Yuan QX, Marceau N, French BA, Fu P, French SW. Mallory body induction in drug-primed mouse liver. Hepatology (Baltimore, Md.). 1996 Sep:24(3):603-12
[PubMed PMID: 8781332]
[12]
Bardag-Gorce F, Oliva J, Villegas J, Fraley S, Amidi F, Li J, Dedes J, French B, French SW. Epigenetic mechanisms regulate Mallory Denk body formation in the livers of drug-primed mice. Experimental and molecular pathology. 2008 Apr:84(2):113-21. doi: 10.1016/j.yexmp.2007.12.004. Epub 2008 Jan 11
[PubMed PMID: 18281034]
[13]
Livneh I, Cohen-Kaplan V, Cohen-Rosenzweig C, Avni N, Ciechanover A. The life cycle of the 26S proteasome: from birth, through regulation and function, and onto its death. Cell research. 2016 Aug:26(8):869-85. doi: 10.1038/cr.2016.86. Epub 2016 Jul 22
[PubMed PMID: 27444871]
[14]
Denk H, Franke WW, Eckerstorfer R, Schmid E, Kerjaschki D. Formation and involution of Mallory bodies ("alcoholic hyalin") in murine and human liver revealed by immunofluorescence microscopy with antibodies to prekeratin. Proceedings of the National Academy of Sciences of the United States of America. 1979 Aug:76(8):4112-6
[PubMed PMID: 386356]
[15]
Shasthry SM, Rastogi A, Bihari C, Vijayaraghavan R, Arora V, Sharma MK, Sarin SK. Histological activity score on baseline liver biopsy can predict non-response to steroids in patients with severe alcoholic hepatitis. Virchows Archiv : an international journal of pathology. 2018 Apr:472(4):667-675. doi: 10.1007/s00428-018-2330-4. Epub 2018 Mar 7
[PubMed PMID: 29516163]
[16]
Harada M. Autophagy is involved in the elimination of intracellular inclusions, Mallory-Denk bodies, in hepatocytes. Medical molecular morphology. 2010 Mar:43(1):13-8. doi: 10.1007/s00795-009-0476-5. Epub 2010 Mar 26
[PubMed PMID: 20340001]
[17]
Harada M, Hanada S, Toivola DM, Ghori N, Omary MB. Autophagy activation by rapamycin eliminates mouse Mallory-Denk bodies and blocks their proteasome inhibitor-mediated formation. Hepatology (Baltimore, Md.). 2008 Jun:47(6):2026-35. doi: 10.1002/hep.22294. Epub
[PubMed PMID: 18454506]
[18]
Ke PY. Diverse Functions of Autophagy in Liver Physiology and Liver Diseases. International journal of molecular sciences. 2019 Jan 13:20(2):. doi: 10.3390/ijms20020300. Epub 2019 Jan 13
[PubMed PMID: 30642133]
[19]
Nikam A, Patankar JV, Somlapura M, Lahiri P, Sachdev V, Kratky D, Denk H, Zatloukal K, Abuja PM. The PPARα Agonist Fenofibrate Prevents Formation of Protein Aggregates (Mallory-Denk bodies) in a Murine Model of Steatohepatitis-like Hepatotoxicity. Scientific reports. 2018 Aug 28:8(1):12964. doi: 10.1038/s41598-018-31389-3. Epub 2018 Aug 28
[PubMed PMID: 30154499]
[20]
Oliva J, Bardag-Gorce F, Li J, French BA, Nguyen SK, Lu SC, French SW. Betaine prevents Mallory-Denk body formation in drug-primed mice by epigenetic mechanisms. Experimental and molecular pathology. 2009 Apr:86(2):77-86. doi: 10.1016/j.yexmp.2008.11.002. Epub 2008 Nov 24
[PubMed PMID: 19073172]