[1]
Saccocci M, Taramasso M, Maisano F. Mitral Valve Interventions in Structural Heart Disease. Current cardiology reports. 2018 May 17:20(6):49. doi: 10.1007/s11886-018-0982-y. Epub 2018 May 17
[PubMed PMID: 29770888]
[2]
Chiu P, Goldstone AB, Woo YJ. Would evolving recommendations for mechanical mitral valve replacement further raise the bar for successful mitral valve repair? European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2018 Oct 1:54(4):622-626. doi: 10.1093/ejcts/ezy284. Epub
[PubMed PMID: 30165483]
[3]
Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, Detaint D, Capps M, Nkomo V, Scott C, Schaff HV, Tajik AJ. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. The New England journal of medicine. 2005 Mar 3:352(9):875-83
[PubMed PMID: 15745978]
[4]
LaPar DJ, Kron IL. Should all ischemic mitral regurgitation be repaired? When should we replace? Current opinion in cardiology. 2011 Mar:26(2):113-7. doi: 10.1097/HCO.0b013e3283439888. Epub
[PubMed PMID: 21245751]
Level 3 (low-level) evidence
[5]
Harb SC, Griffin BP. Mitral Valve Disease: a Comprehensive Review. Current cardiology reports. 2017 Aug:19(8):73. doi: 10.1007/s11886-017-0883-5. Epub
[PubMed PMID: 28688022]
[6]
Salem A, Abdelgawad AME, Elshemy A. Early and Midterm Outcomes of Rheumatic Mitral Valve Repair. The heart surgery forum. 2018 Aug 14:21(5):E352-E358. doi: 10.1532/hsf.1978. Epub 2018 Aug 14
[PubMed PMID: 30311884]
[7]
Shuhaiber J, Anderson RJ. Meta-analysis of clinical outcomes following surgical mitral valve repair or replacement. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2007 Feb:31(2):267-75
[PubMed PMID: 17175161]
Level 2 (mid-level) evidence
[8]
Zhou YX, Leobon B, Berthoumieu P, Roux D, Glock Y, Mei YQ, Wang YW, Fournial G. Long-term outcomes following repair or replacement in degenerative mitral valve disease. The Thoracic and cardiovascular surgeon. 2010 Oct:58(7):415-21. doi: 10.1055/s-0029-1240925. Epub 2010 Oct 4
[PubMed PMID: 20922625]
[9]
Castleberry AW, Williams JB, Daneshmand MA, Honeycutt E, Shaw LK, Samad Z, Lopes RD, Alexander JH, Mathew JP, Velazquez EJ, Milano CA, Smith PK. Surgical revascularization is associated with maximal survival in patients with ischemic mitral regurgitation: a 20-year experience. Circulation. 2014 Jun 17:129(24):2547-56. doi: 10.1161/CIRCULATIONAHA.113.005223. Epub 2014 Apr 17
[PubMed PMID: 24744275]
[10]
Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, Iung B, Otto CM, Pellikka PA, Quiñones M, American Society of Echocardiography, European Association of Echocardiography. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2009 Jan:22(1):1-23; quiz 101-2. doi: 10.1016/j.echo.2008.11.029. Epub
[PubMed PMID: 19130998]
[11]
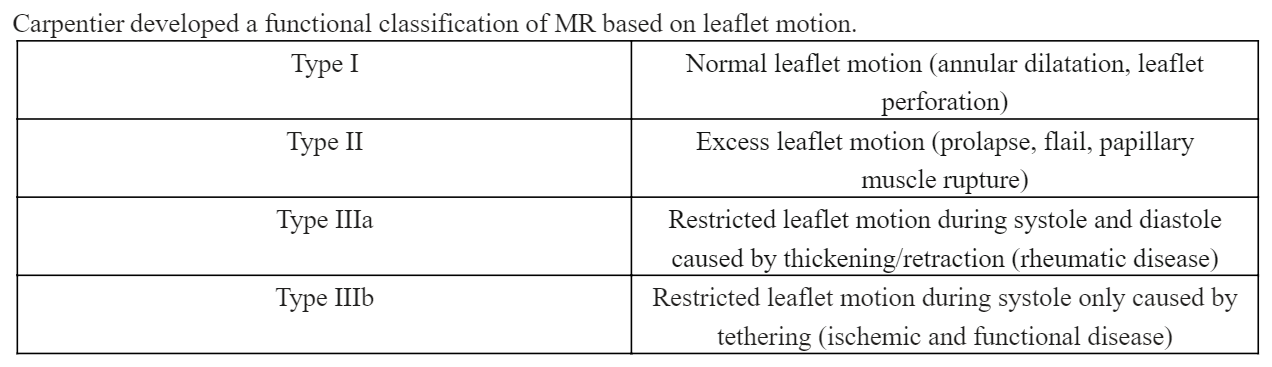
Carpentier A, Relland J, Deloche A, Fabiani JN, D'Allaines C, Blondeau P, Piwnica A, Chauvaud S, Dubost C. Conservative management of the prolapsed mitral valve. The Annals of thoracic surgery. 1978 Oct:26(4):294-302
[PubMed PMID: 380485]
[12]
Mentias A, Naji P, Gillinov AM, Rodriguez LL, Reed G, Mihaljevic T, Suri RM, Sabik JF, Svensson LG, Grimm RA, Griffin BP, Desai MY. Strain Echocardiography and Functional Capacity in Asymptomatic Primary Mitral Regurgitation With Preserved Ejection Fraction. Journal of the American College of Cardiology. 2016 Nov 1:68(18):1974-1986. doi: 10.1016/j.jacc.2016.08.030. Epub 2016 Aug 31
[PubMed PMID: 27591831]
[13]
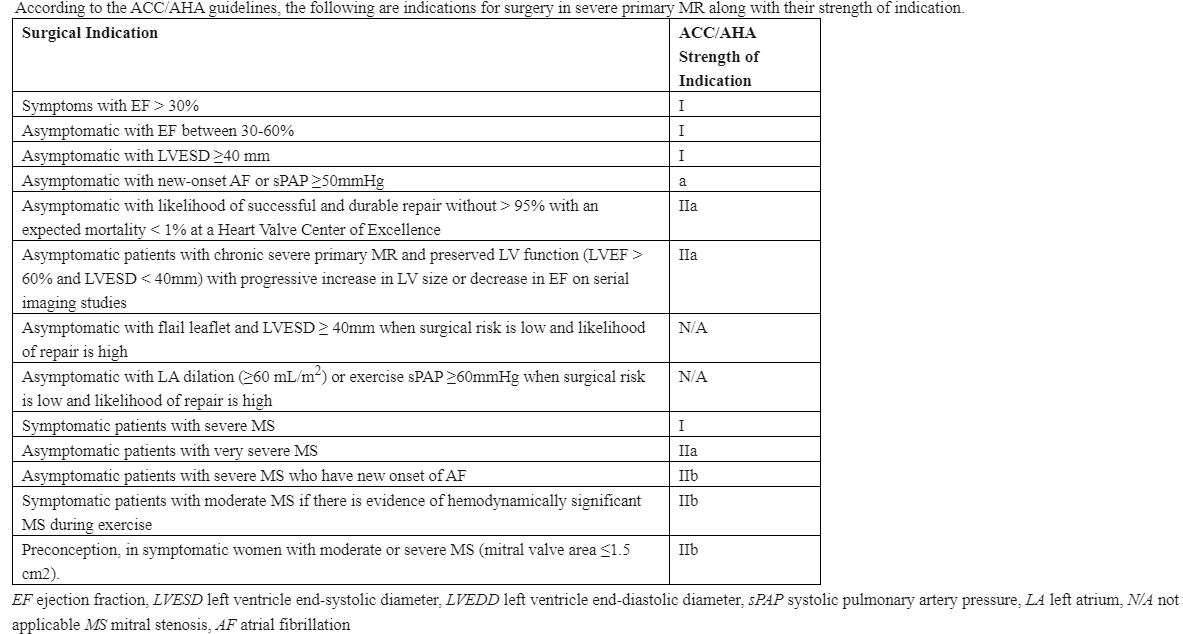
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O'Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2017 Jul 11:70(2):252-289. doi: 10.1016/j.jacc.2017.03.011. Epub 2017 Mar 15
[PubMed PMID: 28315732]
Level 1 (high-level) evidence
[14]
Wu AH, Aaronson KD, Bolling SF, Pagani FD, Welch K, Koelling TM. Impact of mitral valve annuloplasty on mortality risk in patients with mitral regurgitation and left ventricular systolic dysfunction. Journal of the American College of Cardiology. 2005 Feb 1:45(3):381-7
[PubMed PMID: 15680716]
[15]
Chevalier P, Burri H, Fahrat F, Cucherat M, Jegaden O, Obadia JF, Kirkorian G, Touboul P. Perioperative outcome and long-term survival of surgery for acute post-infarction mitral regurgitation. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2004 Aug:26(2):330-5
[PubMed PMID: 15296892]
[16]
Gatti G, Morra L, Castaldi G, Maschietto L, Gripshi F, Fabris E, Perkan A, Benussi B, Sinagra G, Pappalardo A. Preoperative Intra-Aortic Counterpulsation in Cardiac Surgery: Insights From a Retrospective Series of 588 Consecutive High-Risk Patients. Journal of cardiothoracic and vascular anesthesia. 2018 Oct:32(5):2077-2086. doi: 10.1053/j.jvca.2017.12.008. Epub 2017 Dec 6
[PubMed PMID: 29325843]
Level 2 (mid-level) evidence
[17]
Haddad F, Denault AY, Couture P, Cartier R, Pellerin M, Levesque S, Lambert J, Tardif JC. Right ventricular myocardial performance index predicts perioperative mortality or circulatory failure in high-risk valvular surgery. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2007 Sep:20(9):1065-72
[PubMed PMID: 17566702]
[18]
Pinzani A, de Gevigney G, Pinzani V, Ninet J, Milon H, Delahaye JP. [Pre- and postoperative right cardiac insufficiency in patients with mitral or mitral-aortic valve diseases]. Archives des maladies du coeur et des vaisseaux. 1993 Jan:86(1):27-34
[PubMed PMID: 8338397]
[19]
Kennedy JL,LaPar DJ,Kern JA,Kron IL,Bergin JD,Kamath S,Ailawadi G, Does the Society of Thoracic Surgeons risk score accurately predict operative mortality for patients with pulmonary hypertension? The Journal of thoracic and cardiovascular surgery. 2013 Sep;
[PubMed PMID: 22982034]
[20]
Carpentier A, Chauvaud S, Fabiani JN, Deloche A, Relland J, Lessana A, D'Allaines C, Blondeau P, Piwnica A, Dubost C. Reconstructive surgery of mitral valve incompetence: ten-year appraisal. The Journal of thoracic and cardiovascular surgery. 1980 Mar:79(3):338-48
[PubMed PMID: 7354634]
[21]
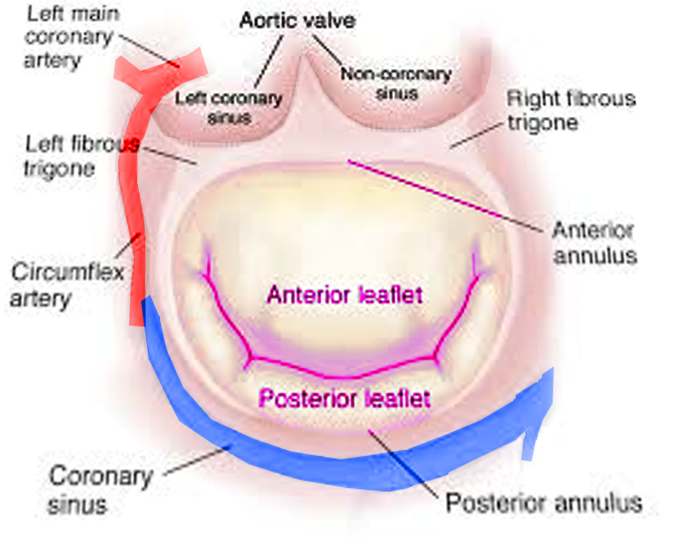
Lawrie GM. Structure, function, and dynamics of the mitral annulus: importance in mitral valve repair for myxamatous mitral valve disease. Methodist DeBakey cardiovascular journal. 2010 Jan-Mar:6(1):8-14
[PubMed PMID: 20360652]
[22]
Gazoni LM,Fedoruk LM,Kern JA,Dent JM,Reece TB,Tribble CG,Smith PW,Lisle TC,Kron IL, A simplified approach to degenerative disease: triangular resections of the mitral valve. The Annals of thoracic surgery. 2007 May;
[PubMed PMID: 17462375]
[23]
Algarni KD,Suri RM,Schaff H, Minimally invasive mitral valve surgery: Does it make a difference? Trends in cardiovascular medicine. 2015 Jul;
[PubMed PMID: 25640311]
[24]
Colli A, Manzan E, Zucchetta F, Bizzotto E, Besola L, Bagozzi L, Bellu R, Sarais C, Pittarello D, Gerosa G. Transapical off-pump mitral valve repair with Neochord implantation: Early clinical results. International journal of cardiology. 2016 Feb 1:204():23-8. doi: 10.1016/j.ijcard.2015.11.131. Epub 2015 Nov 23
[PubMed PMID: 26655529]
[25]
Flameng W, Herijgers P, Bogaerts K. Recurrence of mitral valve regurgitation after mitral valve repair in degenerative valve disease. Circulation. 2003 Apr 1:107(12):1609-13
[PubMed PMID: 12668494]
[26]
Chikwe J, Goldstone AB, Passage J, Anyanwu AC, Seeburger J, Castillo JG, Filsoufi F, Mohr FW, Adams DH. A propensity score-adjusted retrospective comparison of early and mid-term results of mitral valve repair versus replacement in octogenarians. European heart journal. 2011 Mar:32(5):618-26. doi: 10.1093/eurheartj/ehq331. Epub 2010 Sep 16
[PubMed PMID: 20846993]
Level 2 (mid-level) evidence
[27]
Vassileva CM, Ghazanfari N, Spertus J, McNeely C, Markwell S, Hazelrigg S. Heart failure readmission after mitral valve repair and replacement: five-year follow-up in the Medicare population. The Annals of thoracic surgery. 2014 Nov:98(5):1544-50. doi: 10.1016/j.athoracsur.2014.07.040. Epub 2014 Sep 22
[PubMed PMID: 25249161]
[28]
Silaschi M, Chaubey S, Aldalati O, Khan H, Uzzaman MM, Singh M, Baghai M, Deshpande R, Wendler O. Is Mitral Valve Repair Superior to Mitral Valve Replacement in Elderly Patients? Comparison of Short- and Long-Term Outcomes in a Propensity-Matched Cohort. Journal of the American Heart Association. 2016 Jul 28:5(8):. doi: 10.1161/JAHA.116.003605. Epub 2016 Jul 28
[PubMed PMID: 27468927]
[29]
Coutinho GF, Garcia AL, Correia PM, Branco C, Antunes MJ. Negative impact of atrial fibrillation and pulmonary hypertension after mitral valve surgery in asymptomatic patients with severe mitral regurgitation: a 20-year follow-up. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2015 Oct:48(4):548-55; discussion 555-6. doi: 10.1093/ejcts/ezu511. Epub 2015 Jan 5
[PubMed PMID: 25564214]
[30]
Kernis SJ, Nkomo VT, Messika-Zeitoun D, Gersh BJ, Sundt TM 3rd, Ballman KV, Scott CG, Schaff HV, Enriquez-Sarano M. Atrial fibrillation after surgical correction of mitral regurgitation in sinus rhythm: incidence, outcome, and determinants. Circulation. 2004 Oct 19:110(16):2320-5
[PubMed PMID: 15477410]
[31]
Badhwar V, Rankin JS, Damiano RJ Jr, Gillinov AM, Bakaeen FG, Edgerton JR, Philpott JM, McCarthy PM, Bolling SF, Roberts HG, Thourani VH, Suri RM, Shemin RJ, Firestone S, Ad N. The Society of Thoracic Surgeons 2017 Clinical Practice Guidelines for the Surgical Treatment of Atrial Fibrillation. The Annals of thoracic surgery. 2017 Jan:103(1):329-341. doi: 10.1016/j.athoracsur.2016.10.076. Epub
[PubMed PMID: 28007240]
Level 1 (high-level) evidence
[32]
Gillinov M, Soltesz EG. Atrial fibrillation in the patient undergoing mitral valve surgery: A once-in-a-lifetime opportunity. The Journal of thoracic and cardiovascular surgery. 2018 Mar:155(3):995-996. doi: 10.1016/j.jtcvs.2017.09.125. Epub 2017 Oct 9
[PubMed PMID: 29089092]
[33]
Gallerstein PE, Berger M, Rubenstein S, Berdoff RL, Goldberg E. Systolic anterior motion of the mitral valve and outflow obstruction after mitral valve reconstruction. Chest. 1983 May:83(5):819-20
[PubMed PMID: 6839827]
[34]
David TE, Ivanov J, Armstrong S, Christie D, Rakowski H. A comparison of outcomes of mitral valve repair for degenerative disease with posterior, anterior, and bileaflet prolapse. The Journal of thoracic and cardiovascular surgery. 2005 Nov:130(5):1242-9
[PubMed PMID: 16256774]
[35]
Jouan J. Mitral valve repair over five decades. Annals of cardiothoracic surgery. 2015 Jul:4(4):322-34. doi: 10.3978/j.issn.2225-319X.2015.01.07. Epub
[PubMed PMID: 26309841]
[36]
Bolling SF, Li S, O'Brien SM, Brennan JM, Prager RL, Gammie JS. Predictors of mitral valve repair: clinical and surgeon factors. The Annals of thoracic surgery. 2010 Dec:90(6):1904-11; discussion 1912. doi: 10.1016/j.athoracsur.2010.07.062. Epub
[PubMed PMID: 21095334]
[37]
Bridgewater B, Hooper T, Munsch C, Hunter S, von Oppell U, Livesey S, Keogh B, Wells F, Patrick M, Kneeshaw J, Chambers J, Masani N, Ray S. Mitral repair best practice: proposed standards. Heart (British Cardiac Society). 2006 Jul:92(7):939-44
[PubMed PMID: 16251225]
[38]
Chikwe J, Toyoda N, Anyanwu AC, Itagaki S, Egorova NN, Boateng P, El-Eshmawi A, Adams DH. Relation of Mitral Valve Surgery Volume to Repair Rate, Durability, and Survival. Journal of the American College of Cardiology. 2017 Apr 24:():. pii: S0735-1097(17)30677-0. doi: 10.1016/j.jacc.2017.02.026. Epub 2017 Apr 24
[PubMed PMID: 28476349]