Definition/Introduction
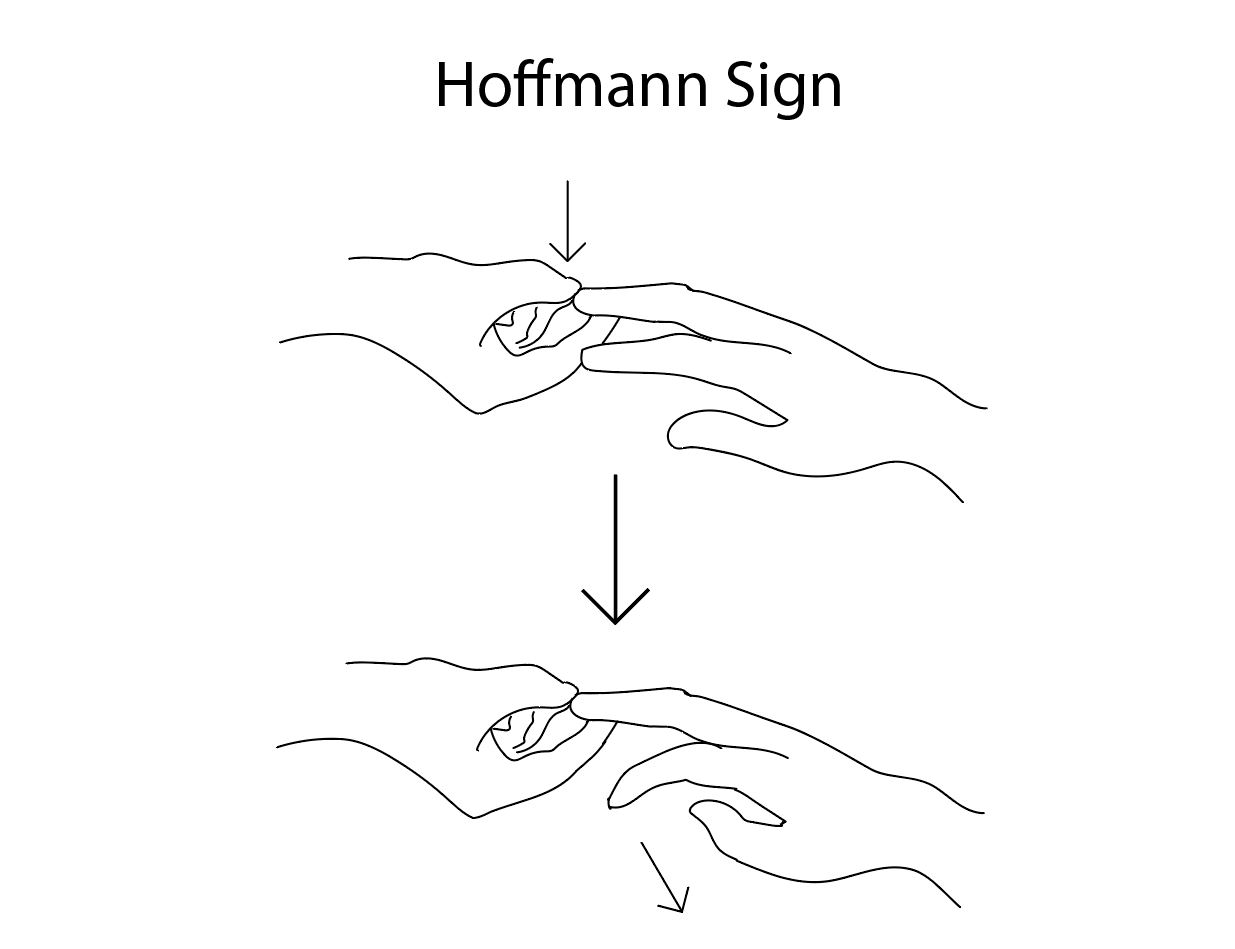
The German neurologist Johann Hoffman first postulated this sign. It was described by his assistant Hans Curschmann in 1911 and has become a standard part of the common neurologic exam.[1] The Hoffman sign is an involuntary flexion movement of the thumb and or index finger when the examiner flicks the fingernail of the middle finger down (see Diagram. Hoffmann Sign). The reflexive pathway causes the thumb to flex and adduct quickly. A positive Hoffman sign indicates an upper motor neuron lesion and corticospinal pathway dysfunction likely due to cervical cord compression. However, up to 3% of the population has been found to have a positive Hoffman without cord compression or upper motor neuron disease.[2]