[1]
Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN, Shaw GM. Spina bifida. Nature reviews. Disease primers. 2015 Apr 30:1():15007. doi: 10.1038/nrdp.2015.7. Epub 2015 Apr 30
[PubMed PMID: 27189655]
[2]
Brody BA, Kinney HC, Kloman AS, Gilles FH. Sequence of central nervous system myelination in human infancy. I. An autopsy study of myelination. Journal of neuropathology and experimental neurology. 1987 May:46(3):283-301
[PubMed PMID: 3559630]
[3]
Sepulveda W, Corral E, Ayala C, Be C, Gutierrez J, Vasquez P. Chromosomal abnormalities in fetuses with open neural tube defects: prenatal identification with ultrasound. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2004 Apr:23(4):352-6
[PubMed PMID: 15065184]
[4]
Au KS, Ashley-Koch A, Northrup H. Epidemiologic and genetic aspects of spina bifida and other neural tube defects. Developmental disabilities research reviews. 2010:16(1):6-15. doi: 10.1002/ddrr.93. Epub
[PubMed PMID: 20419766]
[5]
Shimoji K, Kimura T, Kondo A, Tange Y, Miyajima M, Arai H. Genetic studies of myelomeningocele. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2013 Sep:29(9):1417-25. doi: 10.1007/s00381-013-2197-2. Epub 2013 Sep 7
[PubMed PMID: 24013315]
[6]
Zaganjor I, Sekkarie A, Tsang BL, Williams J, Razzaghi H, Mulinare J, Sniezek JE, Cannon MJ, Rosenthal J. Describing the Prevalence of Neural Tube Defects Worldwide: A Systematic Literature Review. PloS one. 2016:11(4):e0151586. doi: 10.1371/journal.pone.0151586. Epub 2016 Apr 11
[PubMed PMID: 27064786]
Level 1 (high-level) evidence
[7]
Papp C, Adám Z, Tóth-Pál E, Török O, Váradi V, Papp Z. Risk of recurrence of craniospinal anomalies. The Journal of maternal-fetal medicine. 1997 Jan-Feb:6(1):53-7
[PubMed PMID: 9029387]
[8]
Greene ND, Massa V, Copp AJ. Understanding the causes and prevention of neural tube defects: Insights from the splotch mouse model. Birth defects research. Part A, Clinical and molecular teratology. 2009 Apr:85(4):322-30. doi: 10.1002/bdra.20539. Epub
[PubMed PMID: 19180568]
Level 3 (low-level) evidence
[9]
Avagliano L, Massa V, George TM, Qureshy S, Bulfamante GP, Finnell RH. Overview on neural tube defects: From development to physical characteristics. Birth defects research. 2019 Nov 15:111(19):1455-1467. doi: 10.1002/bdr2.1380. Epub 2018 Nov 12
[PubMed PMID: 30421543]
Level 3 (low-level) evidence
[10]
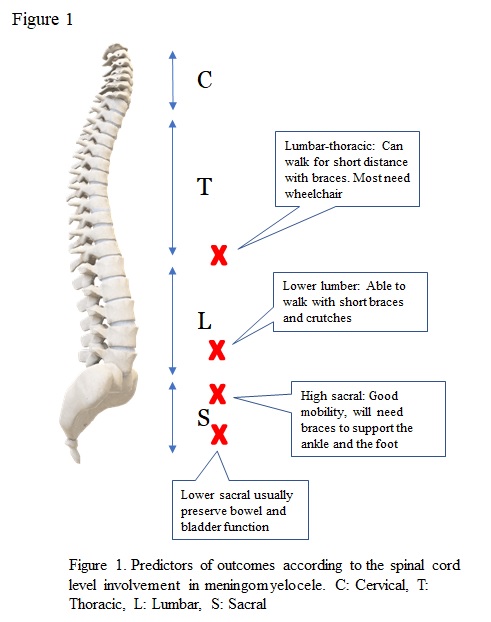
Williams EN, Broughton NS, Menelaus MB. Age-related walking in children with spina bifida. Developmental medicine and child neurology. 1999 Jul:41(7):446-9
[PubMed PMID: 10454227]
[11]
Naidich TP, McLone DG, Fulling KH. The Chiari II malformation: Part IV. The hindbrain deformity. Neuroradiology. 1983:25(4):179-97
[PubMed PMID: 6605491]
[12]
Nagler J, Levy JA, Bachur RG. Stridor in an infant with myelomeningocele. Pediatric emergency care. 2007 Jul:23(7):478-81
[PubMed PMID: 17666932]
[13]
Holinger PC, Holinger LD, Reichert TJ, Holinger PH. Respiratory obstruction and apnea in infants with bilateral abductor vocal cord paralysis, meningomyelocele, hydrocephalus, and Arnold-Chiari malformation. The Journal of pediatrics. 1978 Mar:92(3):368-73
[PubMed PMID: 632975]
[14]
Shaer CM, Chescheir N, Schulkin J. Myelomeningocele: a review of the epidemiology, genetics, risk factors for conception, prenatal diagnosis, and prognosis for affected individuals. Obstetrical & gynecological survey. 2007 Jul:62(7):471-9
[PubMed PMID: 17572919]
[15]
Danzer E, Flake AW. In utero Repair of Myelomeningocele: Rationale, Initial Clinical Experience and a Randomized Controlled Prospective Clinical Trial. Neuroembryology and aging. 2008 Mar:4(4):165-174
[PubMed PMID: 22479081]
Level 1 (high-level) evidence
[16]
Adzick NS, Thom EA, Spong CY, Brock JW 3rd, Burrows PK, Johnson MP, Howell LJ, Farrell JA, Dabrowiak ME, Sutton LN, Gupta N, Tulipan NB, D'Alton ME, Farmer DL, MOMS Investigators. A randomized trial of prenatal versus postnatal repair of myelomeningocele. The New England journal of medicine. 2011 Mar 17:364(11):993-1004. doi: 10.1056/NEJMoa1014379. Epub 2011 Feb 9
[PubMed PMID: 21306277]
Level 1 (high-level) evidence
[17]
Rendeli C, Nucera E, Ausili E, Tabacco F, Roncallo C, Pollastrini E, Scorzoni M, Schiavino D, Caldarelli M, Pietrini D, Patriarca G. Latex sensitisation and allergy in children with myelomeningocele. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2006 Jan:22(1):28-32
[PubMed PMID: 15703967]
[18]
McLone DG. Care of the neonate with a myelomeningocele. Neurosurgery clinics of North America. 1998 Jan:9(1):111-20
[PubMed PMID: 9405769]
[19]
Messing-Jünger M, Röhrig A. Primary and secondary management of the Chiari II malformation in children with myelomeningocele. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2013 Sep:29(9):1553-62. doi: 10.1007/s00381-013-2134-4. Epub 2013 Sep 7
[PubMed PMID: 24013325]
[20]
Hopson B, Rocque BG, Joseph DB, Powell D, McLain ABJ, Davis RD, Wilson TS, Conklin MJ, Blount JP. The development of a lifetime care model in comprehensive spina bifida care. Journal of pediatric rehabilitation medicine. 2018:11(4):323-334. doi: 10.3233/PRM-180548. Epub
[PubMed PMID: 30507593]
[21]
Wilson RD, Lemerand K, Johnson MP, Flake AW, Bebbington M, Hedrick HL, Adzick NS. Reproductive outcomes in subsequent pregnancies after a pregnancy complicated by open maternal-fetal surgery (1996-2007). American journal of obstetrics and gynecology. 2010 Sep:203(3):209.e1-6. doi: 10.1016/j.ajog.2010.03.029. Epub
[PubMed PMID: 20537307]
[22]
Chen CP. Prenatal diagnosis, fetal surgery, recurrence risk and differential diagnosis of neural tube defects. Taiwanese journal of obstetrics & gynecology. 2008 Sep:47(3):283-90. doi: 10.1016/S1028-4559(08)60125-4. Epub
[PubMed PMID: 18935990]
[23]
Mummareddy N, Dewan MC, Mercier MR, Naftel RP, Wellons JC 3rd, Bonfield CM. Scoliosis in myelomeningocele: epidemiology, management, and functional outcome. Journal of neurosurgery. Pediatrics. 2017 Jul:20(1):99-108. doi: 10.3171/2017.2.PEDS16641. Epub 2017 Apr 28
[PubMed PMID: 28452655]
[24]
Beuriat PA, Poirot I, Hameury F, Szathmari A, Rousselle C, Sabatier I, di Rocco F, Mottolese C. Postnatal Management of Myelomeningocele: Outcome with a Multidisciplinary Team Experience. World neurosurgery. 2018 Feb:110():e24-e31. doi: 10.1016/j.wneu.2017.09.169. Epub 2017 Oct 5
[PubMed PMID: 28987842]