Definition/Introduction
Lasegue sign or straight leg raising test (SLRT) is a neurodynamic exam to assess nerve root irritation in the lumbosacral area.[1] It is an integral element to the neurological exam for patients presenting with low back pain with or without radicular pain. The other less commonly used name is Lazarevic sign.
Historical Evolution
Traditionally, Ernest-Charles Lasegue (1816-1883) is considered the first physician who verbally described this sign and emphasized its importance in patients with sciatica.[2] Albeit, he did not write it in his publications.[3] Publication of the sign was by one of Lasegue's students, JJ Forst, who described it in his doctoral thesis titled Contribuition a l’etude Clinique de la Sciatique in 1881. Both Lasegue and Forst proposed that the sharp pain elicited by the test was due to compression of the sciatic nerve by muscular contraction.[2] Historically, Lazarevic (1851-1891) was the first physician who published this sign in 1880 with a sound pathophysiological explanation.[2] The latter suggested sciatic nerve stretching as the cause of pain while doing the test. His explanation had backing by Lucien de Beurmann cadaveric experiment in 1884.[2][4] Several modifications were introduced to SLRT, and different methods were implemented to provoke pain in irritated nerve roots. These modifications intended to improve SLRT accuracy and some other tests could be complementary.[5][6] Of note, although there is no general agreement on interpreting the results of SLRT and its variants[7], performing a combination of tests can enhance their accuracy.[5]
Anatomy Related to SLRT
In the lumbar region, the nerve roots cross the intervertebral disc above the neural foraminae through which they exit.[6] The neural foramen is bounded by the pedicle superiorly, ligamentum flavum posteriorly, and the vertebral body with disc anteriorly. Within the neural foramen, the nerve root is surrounded by loose areolar tissue and lightly tethered to adjacent solid structures. This arrangement allows the nerve roots some room for movement while the limbs move. In other words, in normal conditions, there is a slack nerve root pathway within the foramen. The normal average excursion of lumbosacral nerve roots is about 4 to 6 mm, decreasing with age.[8][9][10] This range of motion grants normal individuals a greater degree of hip flexion (with an extended knee) than patients with nerve root irritation, lumbar disc prolapse, for instance. In cases of disc prolapse, the already existing slack nerve root pathway is taken up by the pathology. The loss of nerve root movement is mainly due to adhesion secondary to the local inflammation and could be due to mechanical compromise as well. Both mechanisms work together to reduce the SLR angle. During SLRT, first the tension, and then the movement appears distally followed by proximally, along the course of sciatic nerve and nerve roots as the hip is flexed.
Causes of Pain While Performing SLRT[11]
- Stretching of the sciatic nerve
- Displacement of the medulla and conus medullaris
- Nerve compression leads to sensitization at the dorsal root ganglion and posterior horn, which in turn leads to the lowering of the pain threshold.
Causes of Positive SLRT
- Nerve root irritation - Intervertebral disc prolapse being the most common cause
- Intraspinal tumor
- Inflammatory radiculopathy
Examination Techniques
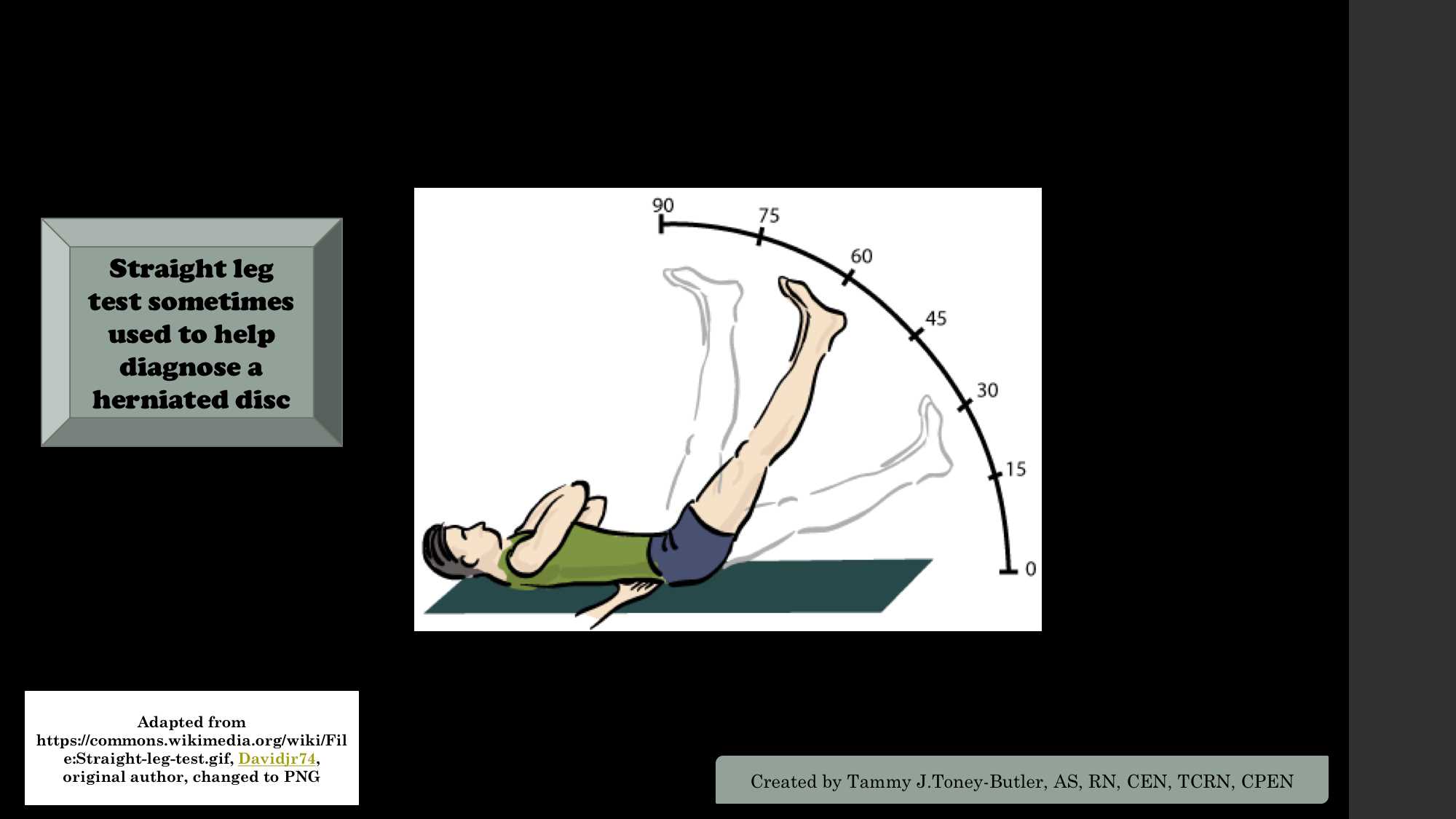
The original method of examination described by JJ Forst[2][6]:
Patient positioning is supine for this test. The involved lower limb is raised with the knee extended. This should evoke pain. The examiner then repeats the maneuver with the leg flexed at the knee and the thigh flexed on the pelvis. This should not evoke pain.
Currently, the following technique is popular in practice[6][12]:
The patient should be informed about the steps of the test, what to expect during the exam and to describe the pain distribution. The patient should be examined in a neutral supine position with the head slightly extended. During the exam, the hips and legs should stay neutral. No hips abduction or adduction is allowed as well as no leg internal or external rotation is permitted. The affected leg is then passively and slowly raised by the ankle with the knee fully extended. Upon eliciting pain, the examiner stops further leg elevation and records the range of motion along with the area of pain distribution.
It is noteworthy that ankle dorsiflexion during SLRT may exaggerate the pain; notwithstanding, it is not part of the Lasegue sign.[13]
Criteria for a true positive SLRT[14][15]
- Radicular leg pain should occur (radiating below the knee).
- Pain occurs when the leg is between 30 and 60 or 70 degrees from horizontal.
What findings should not qualify as a positive SLRT?
- Pain occurring in the low back alone.
- Pain occurring in the posterior thigh alone.
- Pain occurring at an angle less than 30 degrees - May indicate non-organicity or hip joint pathology.
- Pain occurring at an angle more than 70 degrees from the horizontal - More likely cause is tight hamstring or gluteal muscles.
- Pain occurs in a normal person at an angle of 80 to 90 degrees.
Issues of Concern
SLRT modifications and variants: the accuracy of SLRT can be better if it is interpreted with other nerve root tension tests:
- Crossed SLRT[6][16]: AKA well-leg raising test or Fajersztajn sign. When the contralateral leg is lifted, the patient experiences pain on the affected side. This test is more specific than ipsilateral SLRT. It becomes positive, usually in severe compression and centrally located prolapse. Fajersztajn believed that this sign is due to disc prolapse in the axilla of the root.[15]
- Reverse SLRT[17]: AKA femoral stretch or Ely test. While the patient is in a prone position, the leg is lifted off the table with both hip and knee joints extended. Some authors may allow knee flexion. This maneuver may reproduce radicular pain in case of upper lumbar radiculopathy, far lateral lumbar disc, or femoral neuropathy. The pain will present in the femoral nerve distribution on the side of the lesion.
- Braggard test[18][19]: AKA Sciatic stretch test or Flip test. While raising the leg, the foot is held in a dorsiflexed position so that the sciatic nerve is stretched more, thereby increasing the intensity of pain or making it possible to elicit the sign early.
- Reverse flip test: While raising the leg, the foot is held in a plantar-flexed position; this will lessen the pain. But if the patient is complaining of an increase in pain, it can suggest malingering.
- Bowstring sign[15]: Also known as the popliteal compression test or posterior tibial nerve stretch sign. The patient can be examined in sitting or in a supine position. The examiner flexes the knee and applies pressure on the popliteal fossa, evoking sciatica. Some examiners do it after SLRT by flexing the knee to relieve the buttock pain. The pain would be reproduced by a quick snap on the posterior tibial nerve in the popliteal fossa.
Less frequently used nerve root irritation tests:
For the sake of completion, other tests and signs of nerve root tension or irritation are discussed succinctly below:
- Sitting SLRT (Bechterew test)[20]: the patient is made to sit at the edge of a table with both hip and knee flexed, then made to extend the knee joint or elevate the extended knee, which reproduces the radicular pain. They may be able to extend each leg alone, but extending both together causes radicular pain.
- Distracted SLRT: the sitting SLRT is performed without the patient's awareness. The patient is distracted as if the surgeon is examining the foot or pulsation, and slowly, the examiner extends the knee. If the patient is experiencing true radiculopathy, the same pain will be reproduced. Otherwise, we can assume that the patient may be malingering.
- Neri's sign[19]: while bending forward, the patient flexes the knee to avoid stretching the nerve.
- The buckling sign[19]: the patient may flex the knee during SLRT to avoid sciatic nerve tension.
- Sicard sign: passive dorsiflexion of ipsilateral great toe just at the angle of SLRT will produce more pain.
- Kraus-Weber test: the patient may be able to do a sit-up with the knees flexed but not extended.
- Minor sign: the patient may rise from a seated position by supporting himself/herself on the unaffected side, bending forward, and placing one hand on the affected side of the back.
- Bonnet phenomenon: the pain may be more severe or elicited sooner if the test is carried out with the thigh and leg in a position of adduction and internal rotation.
Clinical Significance
Interpretation of SLRT
- Pain radiating down the buttock to the lateral thigh and medial calf - L4 nerve root irritation
- Pain radiating down the buttock to the posterior thigh and lateral calf - L5 nerve root irritation
- Pain radiating down the buttock to the posterior thigh and calf, and lateral foot - S1 nerve root irritation
Interpretation of Positive Reverse SLRT
- L2, L3, or L4 root irritation
- Femoral nerve irritation
Sensitivity and Specificity of the Test
The sensitivity of ipsilateral SLRT is 72 to 97%, and specificity is 11 to 66%, whereas the crossed SLRT sensitivity is 23 to 42% which is less than ipsilateral SLRT but more specific (85 to 100%).[21]
Tests to Confirm Non-organicity While Performing SLRT
- Pain occurring at an angle less than 30 degrees
- A significant discrepancy between the supine and sitting SLRT
- Touch-me-not or Waddell sign - Widespread and excessive tenderness
- Back pain on pressing down on the top of the head
- Overreaction during testing
- Non-dermatomal and non-myotomal neurologic signs
- Pain during simulated spinal rotation: The patient’s hands remain to the sides with hips rotated. There will not be any spine rotation with this maneuver. But the patient will complain of pain.
Nursing, Allied Health, and Interprofessional Team Interventions
A female nurse or chaperone must be present with a female patient while performing SLRT by a male doctor. If the patient is wearing a sari or skirt, she may feel inhibition to raise the leg, which can lead to resistance in the movement and further misinterpretation of SLRT; this is reasonably avoidable with the presence of a chaperone.
The patient may be in severe pain, for which he or she may need proper counseling during the examination, and positioning should be done without hurting the patient further.
Proper communication between the doctor and nurse will help in eliciting SLRT properly without creating false positives.
Nursing, Allied Health, and Interprofessional Team Monitoring
The nurse should provide comfort and explain the test to the patient. During the test, the nurse should observe the patient for pain or discomfort.