Introduction
The lymphatic system is a system that drains the leaked tissue fluid back into the circulation. Its components are lymphatic vessels, lymphatic organs, lymph nodes, and widely scattered lymphoid tissue within the connective tissue. Lymph is the tissue fluid flowing through these lymphatic channels.
Lymphatic vessels contain valves that prevent the backflow of transported lymph.[1] The lymphatic vessels are so thin that the mere presence of valves gives the lymphatic channels the beaded appearance. Lymph flow from the peritoneum navigates through the thoracic duct to the intrathoracic lymph nodes.[2] This extracellular fluid then returns to the bloodstream.[3] Lymph is usually colorless, but that flowing from the intestinal organs is whitish (milky) due to the massive deposition of fat droplets within it and referred to as chyle. The lymphatic system in the gastrointestinal (GI) tract helps regulate the transport of chyle and balance interstitial fluid. A stimulant, such as feeding, activates lymph flow in the GI tract. It is also activated by cholecystokinin (CCK), glucagon, endothelin, bradykinin, substance-P, dopamine, serotonin, and many more. Lymph flow in the GI tract can also be inhibited by anti-diuretic hormone (ADH), vasoactive intestinal polypeptide (VIP), and acetylcholine. The lymphatic system in the intestines mainly functions to provide homeostasis in the GI tract by filtering fluids, blood cells, and plasma proteins that enter the tissue from the blood.[4] The regions above and below the umbilicus drain into axillary lymph nodes and superficial inguinal nodes, respectively. Thus a watershed line is formed horizontally passing through the umbilicus where the lymphatic channels do not cross.[5] The superficial inguinal nodes also receive lymph from the buttocks, penis, scrotum, labium majus, and the lower parts of the anal canal and vagina. This system eventually leads to the external iliac nodes, and finally, the lumbar aortic nodes. The pre-aortic nodes encompass the following nodes: celiac, superior mesenteric, and inferior mesenteric. These nodes drain lymph from the GI tract, spleen, gallbladder, pancreas, and liver. The para-aortic nodes, also known as the lumbar aortic nodes, drain lymph from the kidneys, suprarenal glands, testes, ovaries, uterus, and uterine tubes.
The lymphatic vessels are present in all the tissues except the bone marrow, eyeball, central nervous system, epidermis, cartilage, internal ear, teeth, cornea, and placenta.
Structure and Function
Structure
The lymph capillaries are very fine vessels that form a massive network throughout the body. They begin as blind sacs in the spaces between the cells and carry the leaked tissue fluid along with the cell debris. The lymph passes through lymph nodes where it gets filtered of foreign particles like bacteria and virus and finally returns to the bloodstream. The lymph nodes are almost kidney-shaped, covered by a fibrous capsule that dips down deeper into the tissue in the form of trabeculae. The substance within will be mainly by vast aggregation of lymphocytes in the form of follicles, macrophages, and surrounded by the reticular network. Its concave part is the hilum where an artery, a vein, few nerves, and one efferent vessel are visible. Lymph vessels that carry lymph towards lymph nodes are afferent vessels, are 4 to 5 in number, and they open on the convex surface of the lymph node.
The larger lymphatics contain smooth muscle cells within their walls, and this contributes to the pump-like action that helps in the movement of lymph. Lymph vessels appear beaded because of numerous valves within their wall. These valves prevent backflow. The largest ducts, such as the thoracic and right lymphatic ducts, demonstrate a muscle layer with longitudinal and circular layers that are poorly distinguished.[6] The endothelial cell line the walls of these vessels. When observed under an electron microscope, these endothelial cells contain extremely thin cytoplasm, while the basement membrane is almost absent. There are no pericytes. The lumen of the lymphatics is prevented from collapsing by the presence of fine collagenous filaments that is known as anchoring filaments. These filaments link endothelium to supporting tissue, which is around it, thus preventing the collapse of the lymphatic lumen. They have high permeability, which helps even the absorption of larger molecules.
In the abdomen, they have an extensive network of vessels, which all finally drain into a large sack called cisterna chyle. Usually, they are so thin that they can be seen only by a microscope, except the largest one, the thoracic duct and right lymphatic duct by which the lymph finally reaches the bloodstream.
Lymphatic Drainage Functions
- It provides an immune response by producing T and B lymphocytes.
- It helps to trap foreign microorganisms for ultimate ingestion.[4]
- It carries large proteins to the bloodstream since the blood capillaries do not allow for the absorption of these large molecules.
- It maintains the blood volume by bringing the leaked tissue fluid back into circulation.
- It also eliminates the cell debris from the damaged tissue by filtering and phagocytosis by the lymph nodes.
- It is one of the pathways used by cancer cells to metastasize to other parts of the body.[1]
Embryology
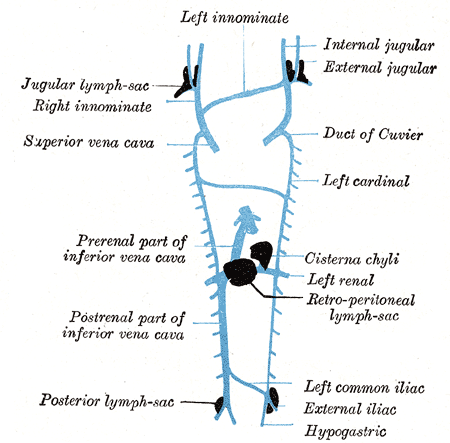
The lymphatic channels have a lining of endothelial cells.[1] The mesenteric lymph sacs appear to derive from the mesenteric vein. New studies show that although these lymph sacs come from the mesenteric vein, some groups of lymphatic endothelial cells are found along the vein but do not actually grow from the vein itself. There is a debate on whether the lymphatic vessels arise from venous or non-venous origins. One study showed that in zebrafish, non-venous cells lie in the embryonic veins that can give rise to lymphatic vessels. Some cells may also differentiate into lymphatic endothelial cells from surrounding mesenchymal cells. The origin of the formation of new lymphatic cells requires further studies, which will even further help in treating diseases related to the lymphatic system.[7]
Blood Supply and Lymphatics
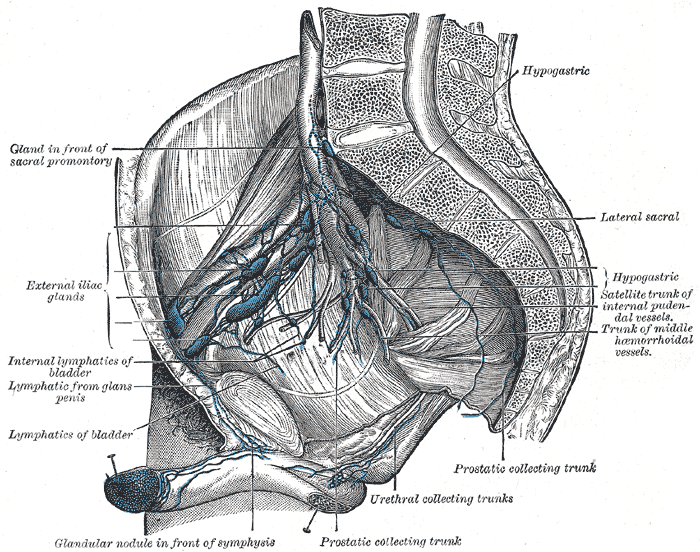
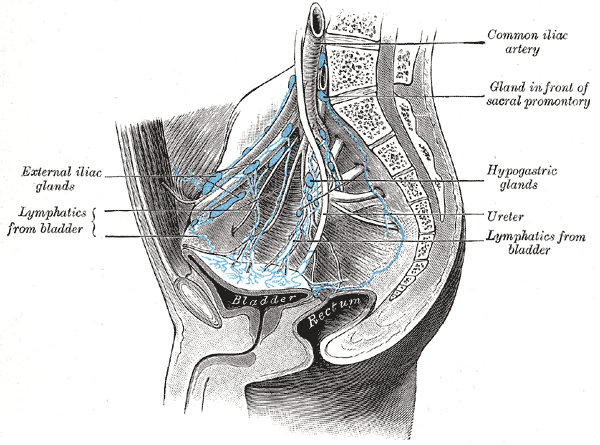
The inguinal lymph nodes are groups of lymph nodes that lie below the inguinal ligament. They classify into two groups, superficial and deep inguinal groups of lymph nodes. Each further divides into upper medial, upper lateral and lower vertical groups. The skin, fasciae, and abdominal wall drain into the superficial inguinal group of lymph nodes. The upper medial group of the superficial inguinal lymph nodes drains the anterior abdominal wall below the umbilicus, up to the perineum, external genitalia, and anal canal. The upper lateral group drains the skin and fasciae of the upper part of the thigh, buttock, and even the lower part of the back. The lower vertical group drains the skin and the fasciae of the lower limb. All the superficial lymph nodes drain later into deep inguinal lymph nodes. The deep inguinal lymph nodes drain not only the superficial inguinal nodes but also deep lymphatics of the lower limb along with the glans penis. All deep nodes finally drain into the external iliac group of lymph nodes.
On the other hand, the abdominal organs, and other deeper structures drain into abdominal lymph nodes like the pre-aortic, para-aortic, common iliac, internal and external iliac groups of lymph nodes.
The lymphatic drainage of the stomach has gained much importance, primarily because of its cancer spread.[8] The carcinoma of the stomach mainly spreads through this route, thus increasing its relevance clinically, especially for staging and surgical resection. The lymphatic drainage of the stomach is initially into the hepatic, left gastric, pancreaticosplenic, gastroepiploic, and pyloric groups of lymph nodes. Finally, all these will drain into the celiac group, which opens into the cisterna chyli.[9]
The liver drains its lymph into the hepatic, caval, posterior mediastinal, and celiac lymph nodes.[6] The lymphatic drainage of the kidneys is to the aortic and caval groups of lymph nodes. Nevertheless, it is not limited to these nodes, as it has been observed to have a distant reach like celiac, iliac, and even thoracic duct directly. Hence it becomes quite a challenge to treat a renal carcinoma patient.[10]
The abdomen is also the site of the largest secondary lymphoid organ, the spleen. This spleen is seen in the left hypochondrium, wedged between the diaphragm and the stomach. It is directed downwards, forwards and laterally along the long axis of the 10th rib. Its hilum is closely related to the tail of the pancreas and covered by a lienorenal ligament. The spleen plays an essential supporting role in the immune system by fighting bacteria and viruses. It facilitates interactions between antigen-presenting cells (APCs) and lymphocytes. APCs regulates the T and B cell responses to the antigenic targets.[11]
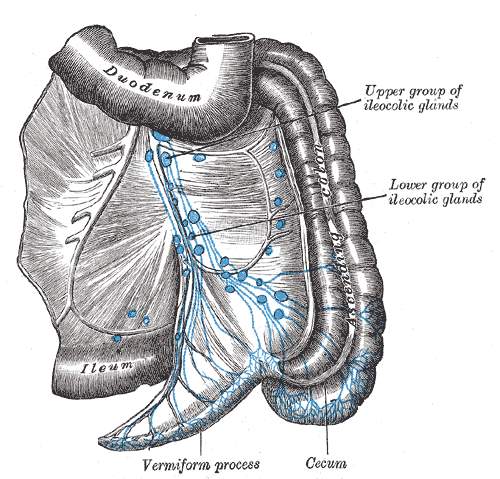
The gut is a potential site of exposure to microorganisms. Hence we find a wide distribution of lymphocytes within the wall of intestine sometimes well aggregated in the form of follicles and sometimes well scattered throughout the mucosa. This is known as a gut-associated lymphoid system (GALT), which is seen especially in the esophagus, intestines, and appendix. In the lamina propria and submucosa of ileum, the lymphocytes become highly aggregated to form lymphoid nodules know as Peyer’s patches. There are around 30 patches, and each patch consists of approximately 100 to 200 nodules seen with the naked eyes. The Peyer’s patches are dome-shaped, covered by epithelium containing M cell, and are devoid of villi. No absorptive cells are seen here.
The lymphatic drainage of the pelvic organs like the female reproductive organs (uterus, cervix, and vagina) is into the internal and external iliac nodes. However, the ovary and the fallopian tube drain into the paraaortic nodes.[12]
The thoracic duct is the large lymphatic vessel, and the principal lymphatic vessel, which drains most of the body, including chyle from the abdomen, begins from the abdomen just below the diaphragm in the form of saccular dilation, the Cisterna Chyli (Chyle Cistern).[13]
Surgical Considerations
Typically, lymphatic drainage in the large and small intestines flows to intraabdominal sentinel lymph nodes. The lymph is then transported to the thoracic duct, and ultimately to the intrathoracic lymph nodes. A study on rats found that following removal of the visceral lymphatic system, the intrathoracic lymph nodes were the first to drain the bowel, most likely through the lymphatic system of the anterior chest wall and diaphragm. This study shows there is a chance that lymph can travel through channels of the diaphragm and parietal surfaces, avoiding any association with the superior mesenteric lymph nodes. This has yet to be studied in human visceral and peritoneal lymph drainage. These findings create a new outlook on the metastatic spread of malignant cells. If this is explored in humans undergoing bowel resection, new treatments can be implemented to aid in enhancing the lymph flow from the peritoneal space to the diaphragm and anterior chest wall via alternate routes.[2]
Clinical Significance
Multiple factors can obstruct lymph flow. One factor depends on how hydrated the interstitial compartment is. Fluid crosses through the interstitial space across cells to eventually reach the lymphatic vessels. In instances of inflammation, filtration through the interstitium increases, which allows for the quick transfer of proteins and other molecules to the lymphatic system. When there is a decrease in the flow or dehydration of fluid across the interstitial space, it backs up into the extracellular space leading to swelling or lymphedema. Others include external forces such as impairment in gut motility, causing impingement on the flow and internal forces where the lymphatic system has a deficit in contractility.[4]
Lymphatic obstruction can lead to immunosuppression, meaning that it cannot perform its function of clearing foreign antigens from the gastrointestinal tract. This failure leads to inflammation of the gastrointestinal tract, playing a role in the pathogenesis of Crohn disease.[14]
Obstruction of lymphatics of the scrotum can lead to scrotal lymphedema, also known as scrotal elephantiasis. It usually occurs in tropical regions where filariasis (Wucheria bancrofti) is endemic.[15] Other causes of lymphedema are granulomatous, disorders of fluid balance, neoplastic, and idiopathic.[16]
A cavity of clear serous fluid, called a seroma, can accumulate in the abdominal wall after surgery; this is due to a disruption of the lymphatic flow.[17]
Consequently, when there is blockage of venous flow in the small intestine, studies have shown that the fluid accumulated is shunted to the lymphatic system, leading to inflammation in the intestines.[4]
Hypothetically, malignant cells travel to the sentinel lymph nodes initially.[18] Sentinel lymph nodes function in transporting malignant cells to distal sites in the body. These nodes usually undergo biopsy first to determine the staging and prognosis of cancer in the body.[4]
Other Issues
Diseases of the lymphatic system in the abdomen rarely occur. When they do, they can be a product of either primary or secondary causes. Primary causes are essentially due to a disruption in the development of the lymphatic system itself. These causes encompass congenital or developmental conditions. Secondary causes can be due to a result of other diseases.
One primary cause of disease in the abdominal lymphatic system is lymphangiomas. Lymphangiomas are benign, thin-walled cystic masses. They mostly occur in the mediastinal and axillary regions, but 5% occur in the mesentery, retroperitoneum, and abdominal viscera. The pathogenesis of lymphangiomas is hypothesized as a failure of newly developing tissue of lymphatic origin to connect to the main lymphatic system causing increased growth of lymphatic sinusoids. The mesentery is the most common site of occurrence.
Another primary cause is generalized systemic lymphangiomatosis. This disease happens in children and is an abnormality of the developing lymphatic system and increased growth affecting all body systems.
One example of a secondary cause of disease in the abdominal lymphatic system is lymphangiectasia due to parasitic infections. Components of the parasite block the lymphatic drainage, creating fluid build-up and an inability of the lymphatic vessels to contract.[19]