[1]
Zibis A, Mitrousias V, Galanakis N, Chalampalaki N, Arvanitis D, Karantanas A. Variations of transverse foramina in cervical vertebrae: what happens to the vertebral artery? European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2018 Jun:27(6):1278-1285. doi: 10.1007/s00586-018-5523-2. Epub 2018 Feb 17
[PubMed PMID: 29455293]
[2]
Yuan SM. Aberrant Origin of Vertebral Artery and its Clinical Implications. Brazilian journal of cardiovascular surgery. 2016 Feb:31(1):52-9. doi: 10.5935/1678-9741.20150071. Epub
[PubMed PMID: 27074275]
[3]
Meila D, Tysiac M, Petersen M, Theisen O, Wetter A, Mangold A, Schlunz-Hendann M, Papke K, Brassel F, Berenstein A. Origin and course of the extracranial vertebral artery: CTA findings and embryologic considerations. Clinical neuroradiology. 2012 Dec:22(4):327-33. doi: 10.1007/s00062-012-0171-0. Epub 2012 Sep 1
[PubMed PMID: 22941252]
[4]
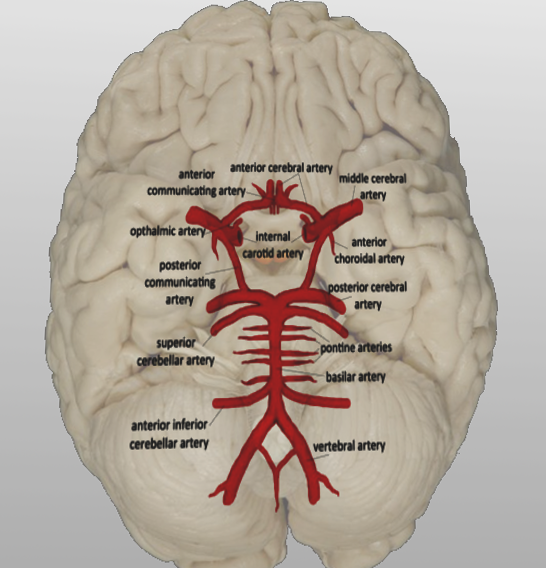
Menshawi K, Mohr JP, Gutierrez J. A Functional Perspective on the Embryology and Anatomy of the Cerebral Blood Supply. Journal of stroke. 2015 May:17(2):144-58. doi: 10.5853/jos.2015.17.2.144. Epub 2015 May 29
[PubMed PMID: 26060802]
Level 3 (low-level) evidence
[5]
Komiyama M, Morikawa T, Nakajima H, Nishikawa M, Yasui T. High incidence of arterial dissection associated with left vertebral artery of aortic origin. Neurologia medico-chirurgica. 2001 Jan:41(1):8-11; discussion 11-2
[PubMed PMID: 11218642]
[6]
Gabrielli R, Rosati MS. Ataxia and vertigo due to anomalous origin of the left vertebral artery. Journal of vascular surgery. 2013 Sep:58(3):803. doi: 10.1016/j.jvs.2012.04.045. Epub
[PubMed PMID: 23972248]
[7]
Lacout A, Khalil A, Figl A, Liloku R, Marcy PY. Vertebral arteria lusoria: a life-threatening condition for oesophageal surgery. Surgical and radiologic anatomy : SRA. 2012 May:34(4):381-3. doi: 10.1007/s00276-011-0867-x. Epub 2011 Sep 8
[PubMed PMID: 21901375]
[8]
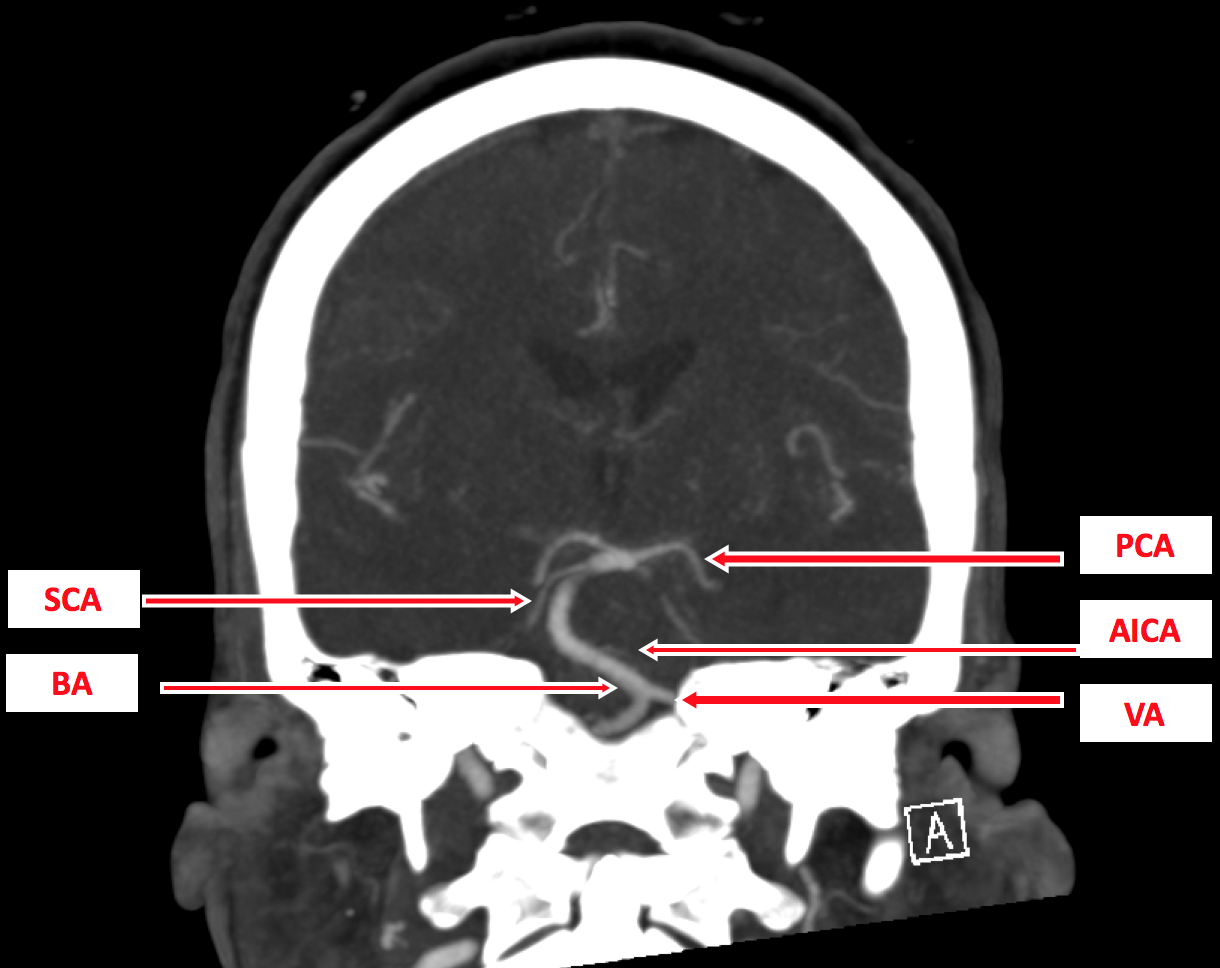
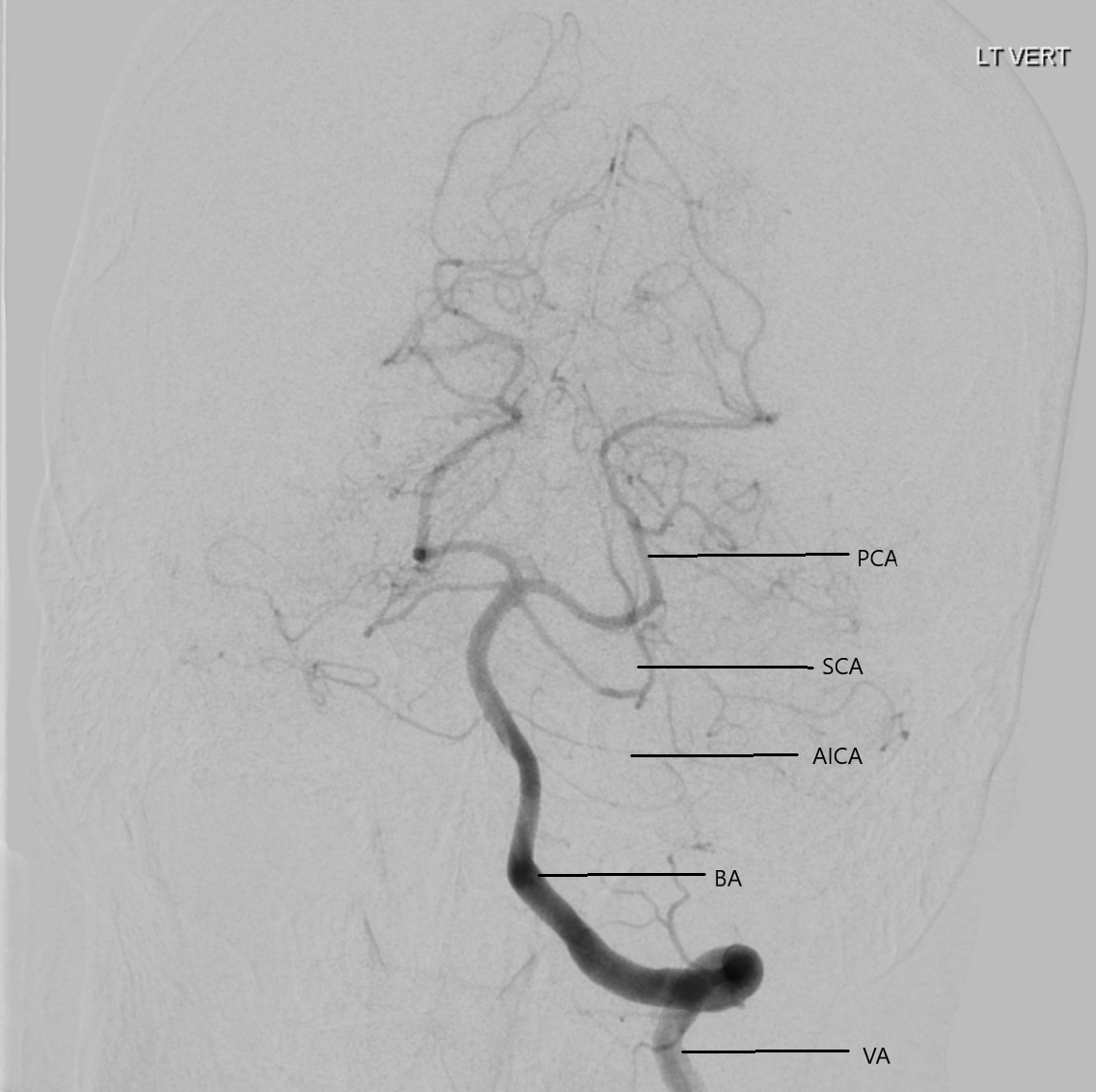
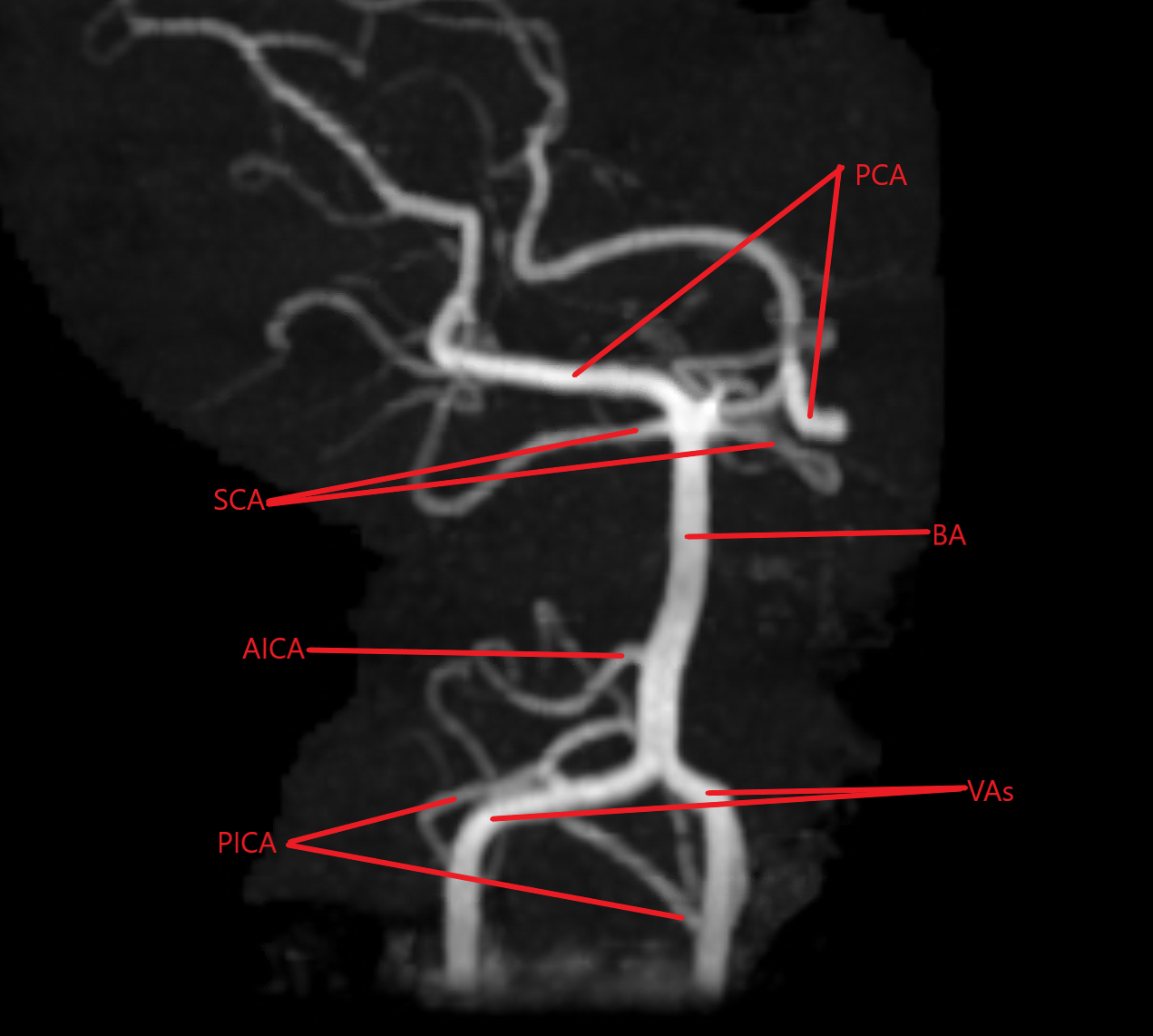
Ghandehari K, Ghandehari K. Interesting basis of vertebrobasilar arterial territory. Iranian journal of neurology. 2012:11(3):111-4
[PubMed PMID: 24250875]
[9]
Isaji T, Yasuda M, Kawaguchi R, Aoyama M, Niwa A, Nakura T, Matsuo N, Takayasu M. Posterior inferior cerebellar artery with an extradural origin from the V(3) segment: higher incidence on the nondominant vertebral artery. Journal of neurosurgery. Spine. 2018 Feb:28(2):154-159. doi: 10.3171/2017.5.SPINE161286. Epub 2017 Dec 1
[PubMed PMID: 29192876]
[10]
Zhou R, Liu D, Yu K, Chen Y, Li L, Xu J, Zhou H. Carotid and vertebral arterial variations in Alzheimer's disease. Current Alzheimer research. 2015:12(4):368-76
[PubMed PMID: 25817257]
[11]
Park JH, Kim JM, Roh JK. Hypoplastic vertebral artery: frequency and associations with ischaemic stroke territory. Journal of neurology, neurosurgery, and psychiatry. 2007 Sep:78(9):954-8
[PubMed PMID: 17098838]
[13]
Eskander MS, Drew JM, Aubin ME, Marvin J, Franklin PD, Eck JC, Patel N, Boyle K, Connolly PJ. Vertebral artery anatomy: a review of two hundred fifty magnetic resonance imaging scans. Spine. 2010 Nov 1:35(23):2035-40. doi: 10.1097/BRS.0b013e3181c9f3d4. Epub
[PubMed PMID: 20938397]
[14]
Cakmak O, Gurdal E, Ekinci G, Yildiz E, Cavdar S. Arcuate foramen and its clinical significance. Saudi medical journal. 2005 Sep:26(9):1409-13
[PubMed PMID: 16155658]
[15]
Cushing KE,Ramesh V,Gardner-Medwin D,Todd NV,Gholkar A,Baxter P,Griffiths PD, Tethering of the vertebral artery in the congenital arcuate foramen of the atlas vertebra: a possible cause of vertebral artery dissection in children. Developmental medicine and child neurology. 2001 Jul;
[PubMed PMID: 11463182]
[16]
Koutsouraki E, Avdelidi E, Michmizos D, Kapsali SE, Costa V, Baloyannis S. Kimmerle's anomaly as a possible causative factor of chronic tension-type headaches and neurosensory hearing loss: case report and literature review. The International journal of neuroscience. 2010 Mar:120(3):236-9. doi: 10.3109/00207451003597193. Epub
[PubMed PMID: 20374094]
Level 3 (low-level) evidence
[17]
Zibis AH, Mitrousias V, Baxevanidou K, Hantes M, Karachalios T, Arvanitis D. Anatomical variations of the foramen transversarium in cervical vertebrae: findings, review of the literature, and clinical significance during cervical spine surgery. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2016 Dec:25(12):4132-4139
[PubMed PMID: 27554348]
[18]
Murlimanju BV, Prabhu LV, Shilpa K, Rai R, Dhananjaya KV, Jiji PJ. Accessory transverse foramina in the cervical spine: incidence, embryological basis, morphology and surgical importance. Turkish neurosurgery. 2011:21(3):384-7. doi: 10.5137/1019-5149.JTN.4047-10.0. Epub
[PubMed PMID: 21845576]
[20]
Neo M, Fujibayashi S, Miyata M, Takemoto M, Nakamura T. Vertebral artery injury during cervical spine surgery: a survey of more than 5600 operations. Spine. 2008 Apr 1:33(7):779-85. doi: 10.1097/BRS.0b013e31816957a7. Epub
[PubMed PMID: 18379405]
Level 3 (low-level) evidence
[21]
Lunardini DJ, Eskander MS, Even JL, Dunlap JT, Chen AF, Lee JY, Ward TW, Kang JD, Donaldson WF. Vertebral artery injuries in cervical spine surgery. The spine journal : official journal of the North American Spine Society. 2014 Aug 1:14(8):1520-5. doi: 10.1016/j.spinee.2013.09.016. Epub 2013 Oct 10
[PubMed PMID: 24411832]
[22]
Smith MD, Emery SE, Dudley A, Murray KJ, Leventhal M. Vertebral artery injury during anterior decompression of the cervical spine. A retrospective review of ten patients. The Journal of bone and joint surgery. British volume. 1993 May:75(3):410-5
[PubMed PMID: 8496209]
Level 2 (mid-level) evidence
[23]
Marks MP, Wojak JC, Al-Ali F, Jayaraman M, Marcellus ML, Connors JJ, Do HM. Angioplasty for symptomatic intracranial stenosis: clinical outcome. Stroke. 2006 Apr:37(4):1016-20
[PubMed PMID: 16497979]
Level 2 (mid-level) evidence
[24]
Mohammadian R, Sharifipour E, Mansourizadeh R, Sohrabi B, Nayebi AR, Haririan S, Farhoudi M, Charsouei S, Najmi S. Angioplasty and stenting of symptomatic vertebral artery stenosis. Clinical and angiographic follow-up of 206 cases from Northwest Iran. The neuroradiology journal. 2013 Aug:26(4):454-63
[PubMed PMID: 24007733]
Level 3 (low-level) evidence
[25]
Zhou Y, Wang L, Zhang JR, Zhou K, Shuai J, Gong ZL, Liu Y, Wei F, Han YF, Shen L, Yang QW. Angioplasty and stenting for severe symptomatic atherosclerotic stenosis of intracranial vertebrobasilar artery. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2019 May:63():17-21. doi: 10.1016/j.jocn.2019.02.017. Epub 2019 Mar 6
[PubMed PMID: 30850180]
[26]
Jenkins JS, Subramanian R. Vertebral and intracranial artery angioplasty. The Ochsner journal. 2003 Winter:5(1):36-9
[PubMed PMID: 22470254]
[29]
Brandt T, Morcher M, Hausser I. Association of cervical artery dissection with connective tissue abnormalities in skin and arteries. Frontiers of neurology and neuroscience. 2005:20():16-29. doi: 10.1159/000088131. Epub
[PubMed PMID: 17290108]
[30]
Klingelhöfer J, Conrad B, Benecke R, Frank B. Transcranial Doppler ultrasonography of carotid-basilar collateral circulation in subclavian steal. Stroke. 1988 Aug:19(8):1036-42
[PubMed PMID: 3041649]
[32]
Provenzale JM, Sarikaya B. Comparison of test performance characteristics of MRI, MR angiography, and CT angiography in the diagnosis of carotid and vertebral artery dissection: a review of the medical literature. AJR. American journal of roentgenology. 2009 Oct:193(4):1167-74. doi: 10.2214/AJR.08.1688. Epub
[PubMed PMID: 19770343]
[33]
Villablanca JP, Nael K, Habibi R, Nael A, Laub G, Finn JP. 3 T contrast-enhanced magnetic resonance angiography for evaluation of the intracranial arteries: comparison with time-of-flight magnetic resonance angiography and multislice computed tomography angiography. Investigative radiology. 2006 Nov:41(11):799-805
[PubMed PMID: 17035870]
[34]
Almeida JP, Medina R, Tamargo RJ. Management of posterior fossa arteriovenous malformations. Surgical neurology international. 2015:6():31. doi: 10.4103/2152-7806.152140. Epub 2015 Feb 25
[PubMed PMID: 25745586]
[35]
Machado MC, Kodaira S, Musolino NR. Persistence of intrasellar trigeminal artery and simultaneous pituitary adenoma: description of two cases and their importance for the differential diagnosis of sellar lesions. Arquivos brasileiros de endocrinologia e metabologia. 2014 Aug:58(6):661-5
[PubMed PMID: 25211451]
Level 3 (low-level) evidence
[36]
Lambert SL, Williams FJ, Oganisyan ZZ, Branch LA, Mader EC Jr. Fetal-Type Variants of the Posterior Cerebral Artery and Concurrent Infarction in the Major Arterial Territories of the Cerebral Hemisphere. Journal of investigative medicine high impact case reports. 2016 Jul-Sep:4(3):2324709616665409. doi: 10.1177/2324709616665409. Epub 2016 Sep 13
[PubMed PMID: 27660767]
Level 3 (low-level) evidence