Continuing Education Activity
Hemorrhoids are a common condition that can cause significant discomfort. Among the available treatment options, rubber band ligation (RBL) is a widely utilized and minimally invasive procedure for addressing this issue. Initially described by Blaisdel and popularized by Barron in 1963, RBL is effective for grades 1 and 2 internal hemorrhoids. This simple procedure is typically performed in an office without bowel preparation or sedation. RBL involves placing a rubber band around the hemorrhoid, inducing ischemia in the hemorrhoidal tissue; this leads to tissue detachment and ulcer formation, promoting healing and tissue attachment to the rectal wall. Comparative studies show RBL's superiority over other treatments like sclerotherapy and infrared coagulation. The procedure is performed just above the dentate line due to the lack of somatic sensitivity in this area, minimizing discomfort. Office-based procedures aim to alleviate symptoms, reduce hemorrhoidal tissue size and vascularity, and enhance tissue attachment, minimizing the chances of postoperative prolapse. While these interventions are generally well-tolerated and associated with reduced pain, discussions about complications, recurrence rates, and the potential need for repeated procedures are essential for patients and healthcare providers.
This activity describes hemorrhoid banding, exploring its historical context, procedural details, and comparative advantages. Communication and collaboration among the interprofessional care team, including physicians, nurses, and support staff, contribute to improved patient care.
Objectives:
Identify appropriate candidates for hemorrhoid banding based on the severity of their condition and response to conservative treatments.
Differentiate between various treatment options for hemorrhoids and choose rubber band ligation when appropriate for grades 1, 2, and 3 hemorrhoids that fail conservative therapy.
Implement the rubber band ligation procedure with precision and attention to detail, including proper placement of rubber bands, positioning, and use of the anoscope.
Coordinate with the interprofessional team to optimize patient care, emphasizing each team member's role.
Introduction
Hemorrhoids, a widespread medical concern, frequently lead to discomfort and distress. Among the various treatment options, rubber band ligation (RBL) is a predominant minimally invasive procedure to manage this condition.[1] Acknowledged as the gold standard, RBL is particularly effective for symptomatic grade 1, 2, and 3 hemorrhoids that do not respond to conservative treatments.[2] This technique, which has a rich history of successful application, offers an efficient means of treating internal hemorrhoids, particularly those classified as grades 1 and 2. Initially described by Blaisdel and later popularized by Barron in 1963, RBL is widely recognized for its effectiveness in alleviating symptoms and improving patients' quality of life.[3][4] Comparative studies have shown that RBL is superior to other treatment modalities, such as sclerotherapy and infrared coagulation, underscoring its effectiveness and popularity in the medical community.[5]
One of the notable advantages of RBL is its simplicity and minimal invasiveness, as this procedure is typically performed in an office without the need for bowel preparation or sedation. The procedure involves the placement of a rubber band, which induces ischemia in the hemorrhoid, eventually leading to the formation of an ulcer and the detachment of the problematic tissue. Consequently, this method promotes healing and the attachment of scar tissue to the rectal wall. Furthermore, the procedure is performed on tissue above the dentate line, which lacks somatic sensitivity, thereby minimizing discomfort and ensuring that patients tolerate the procedure well.
The primary objectives of office-based procedures for hemorrhoid management are to mitigate patient symptoms by reducing the size or vascularity of the hemorrhoidal tissue and facilitating scar tissue attachment to the rectal wall. Achieving these goals minimizes the chances of postoperative prolapse and enhances patient comfort. While these office-based interventions are generally well-tolerated and associated with reduced pain and discomfort, discussions surrounding recurrence rates and the potential need for repeated procedures are essential considerations for patients and healthcare providers.[6][7]
Anatomy and Physiology
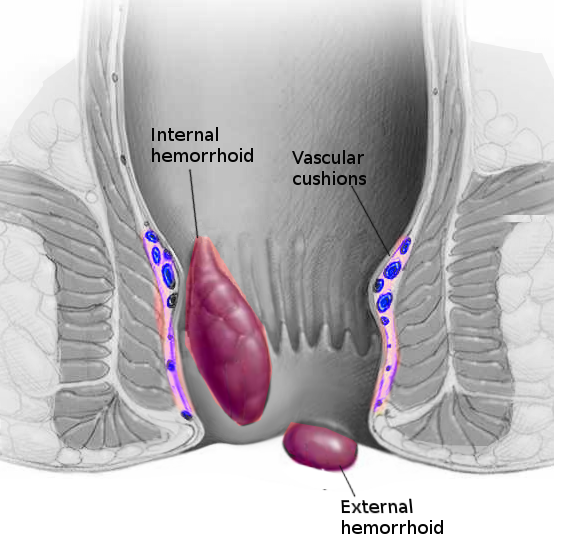
Hemorrhoids are classified by their anatomic origin and position relative to the dentate line. They are categorized into internal, external, and mixed hemorrhoids, each with distinct characteristics. Understanding hemorrhoids' anatomical and pathophysiological aspects is crucial for diagnosing and managing this condition.
Internal Hemorrhoids
Internal hemorrhoids are situated above the dentate line and are vascular cushions originating from the superior hemorrhoidal cushion. They contain an extensive network of arteriovenous shunts and small vascular sinusoids. They are composed primarily of elastic and connective tissue and are enclosed by the Trietz suspensory ligament surrounding the entire corpus cavernosum recti.[8] They are covered by columnar epithelium that receives visceral innervation. Therefore, these hemorrhoids are less sensitive to pain and irritation.
Their 3 primary positions, left lateral, right anterior, and right posterior, correspond to the terminal branches of the middle and superior hemorrhoidal veins. Internal hemorrhoids drain through the superior rectal vein into the portal system. Internal hemorrhoids contribute approximately 15% to 20% of the resting anal pressure and provide important sensory information, enabling the differentiation between solid, liquid, and gas. Since they are arterial, as confirmed by blood gas results, they respond to physiological processes such as Valsalva maneuvers, leading to the filling of the sinusoids and an increase in resting anal pressure.
Internal hemorrhoids are categorized based on the extent of prolapse from the anal canal:
- Grade 1 - does not prolapse below the dentate line, seen during anoscopy
- Grade 2 - prolapse out of the anal canal but reduce spontaneously
- Grade 3 - prolapse out of the anal canal and require manual reduction
- Grade 4 - irreducible and may strangulate
External Hemorrhoids
External hemorrhoids are below the dentate line, typically around the anal verge. They are covered by skin, anoderm, and squamous epithelium. They receive somatic innervation from the sensory branches of the pudendal nerve and are very sensitive to pain and irritation. Unlike internal hemorrhoids, external hemorrhoids are mainly venous and have similar vascular sinusoids but are notably larger. Due to the slower blood flow in these veins, external hemorrhoids are susceptible to thrombosis. External hemorrhoids drain through the inferior rectal vein into the inferior vena cava.
Mixed Hemorrhoids
Mixed hemorrhoids are the confluence of internal and external hemorrhoids; they straddle the dentate line. Venous anastomoses exist between them and the middle rectal vein, connecting the portal and systemic circulations.
Pathophysiology of Hemorrhoids
The development of hemorrhoids is attributed to several factors, including straining during bowel movements, an imbalanced diet, and poor bowel habits. These factors can lead to increased vascularity, inflammation, hypertonicity of the anal sphincter, and potential imbalances in connective tissue enzymes. As a result, the Treitz muscle may deteriorate, causing the downward displacement of hemorrhoidal cushions. This process contributes to the dilation of arteriovenous anastomoses and the blood pooling in the veins, ultimately leading to the formation of hemorrhoidal disease.
Indications
The selection criteria for choosing between a minimally invasive treatment and a surgical procedure for managing hemorrhoids is not always straightforward. Based on several surveys conducted among surgeons, it is clear that there is an overlap of indications, which highlights the complexity of the decision-making process.
Hemorrhoid band ligation is a commonly accepted treatment for grade 1, grade 2, and selected cases of grade 3 internal hemorrhoids when the patient complains of bleeding or prolapse of hemorrhoids.[1] Band ligation may also be considered for bleeding in severely anemic patients with grade 4 hemorrhoids unfit for surgery, such as patients with cirrhosis and portal hypertension.[9]
Contraindications
RBL is contraindicated in the following conditions:
- Large grade 4 hemorrhoids
- Inflammatory and infectious conditions in the anorectal region (eg, perianal abscess, Crohn disease, proctitis, colitis)
- Due to the increased risk of complications and the possibility of spontaneous healing, conservative treatment of proctologic diseases in patients with Crohn disease has been recommended. Although there may be potential for surgery in carefully selected patients, definitive conclusions have not been made.[10]
- Acutely thrombosed hemorrhoids [11]
- Chronic anal fissure (Surgery is a more appropriate treatment.)
- Hypertrophied anal papilla
- Insufficient tissue to pull into the band ligator
- Anticoagulated state
- Patients who are unlikely to follow up
Equipment
An anoscope or proctoscope is inserted into the anus and allows visualization of the hemorrhoids and identification of the dentate line.
There are several different RBL systems available. Some banders utilize a grasper or forceps, while others use suction to pull internal hemorrhoids into the banding instrument. Two of the suction devices are described below.
Endoscopic suction ligator:
- This method involves suctioning the symptomatic hemorrhoid into a ligating drum connected to an endoscope. The ring is released through a trigger passed through the endoscope's biopsy channel.
- This may provide effective ligation with fewer sessions.
- A single-handed nonendoscopic ligating device has also demonstrated successful outcomes and is a cost-effective alternative to the endoscopic device.
Wall suction ligator:
- This uses a vacuum suction with the ligator attached to a wall suction.
- This can be performed in fewer sessions than the standard forceps technique.
- No assistant is required to perform a ligation with this device.
Personnel
Depending on the type of band ligator used, RBL can be performed by the clinician alone or with an assistant.
Preparation
Patient Preparation
- This is typically straightforward, and while some surgeons may advise an enema before the procedure, it is not universally necessary.
- In most cases, there is no requirement for preoperative intravenous antibiotics.
- If done correctly, the procedure should require no anesthesia, local or intravenous.
Equipment and Setup
- The necessary equipment should be gathered: anoscope or proctoscope and a banding system, including the ligator and rubber bands.
- The treatment area should be adequately lit to ensure optimal visualization during the procedure.
Patient Assessment
- The patient's hemorrhoid symptomatology should be evaluated, noting acute bleeding and other relevant issues.
- The hemorrhoids' size, position, and severity should be determined, with the most prominent identified for the initial treatment.
- The patient should be assessed for which position would be the best and safest for the procedure. The patient's positioning can vary based on several factors, including the surgeon's preference, body habitus, and any comorbidities the patient may have. Options include the prone jackknife, lithotomy, or lateral decubitus positions. Selection depends on what best suits the individual patient, with considerations made to ensure their comfort and safety, especially in cases where patients have morbid obesity, which may necessitate the lithotomy position instead of the jackknife.
Technique or Treatment
RBL for hemorrhoids grade 1, 2, and 3 can successfully be treated in an office setting with rubber band ligation.[12][13] The patient is carefully positioned for the procedure. A scope is introduced into the rectum, the dentate line is located, and the hemorrhoids are identified. The largest hemorrhoidal column should be treated first. The procedure is conducted through an anoscope, placing small rubber band rings on the internal hemorrhoids using a band ligation device. Traditionally, forceps have been used for this purpose, although alternative methods, such as suction ligators, have been developed as previously discussed. When utilizing a forceps ligator, an assistant must stabilize the scope while the clinician performs the ligation. The internal hemorrhoid is gently grasped about 1 to 2 cm proximal to the dentate line using forceps, and the patient is asked to provide feedback regarding any pain or sensation. The presence of pain indicates that a more proximal point in the anal canal should be selected. Once it is determined that the appropriate tissue has been grasped, any excess tissue is drawn towards the tip or drum of the handheld ligator gun apparatus, and the trigger is activated to release the rubber band. These rubber rings are then advanced down to the neck of the hemorrhoid. A critical technical aspect is to ensure that the bands are placed at least 5 mm above the dentate line to prevent them from being positioned on somatically innervated tissue. Misapplication of the band below the dentate line or associated spasms can lead to severe pain, necessitating the immediate removal of the band by cutting it if severe pain occurs during placement.
Typically, only 1 hemorrhoidal column is treated at a time to minimize excessive tissue necrosis. However, if the patient tolerates the procedure with minimal discomfort, multiple hemorrhoids can be banded during the same session, with up to 3 bands in a single column safely applied. If further sessions are required, repeat banding procedures can be conducted at 3- to 4-week intervals to allow any swelling and ulcerations to subside. Thorough documentation of the procedure, including findings, steps, and patient responses, is essential.
Successful ligation induces thrombosis within the hemorrhoid, leading to localized submucosal scarring. The banded hemorrhoidal tissues rapidly undergo ischemia and subsequent necrosis over the following 3 to 5 days, causing an area of ulceration. Complete healing usually takes several weeks later. Patients should receive clear post-treatment instructions, including guidance on managing pain and necessary precautions. They should be informed that anal or rectal tightness sensations can be considered normal. Additionally, a follow-up appointment should be scheduled to monitor the patient's progress and evaluate the effectiveness of the RBL treatment.[14]
Complications
There are several complications associated with RBL of hemorrhoids. They can be classified as minor or severe. Mild bleeding, pain, and delayed bleeding are the most common complications. Delayed bleeding typically presents 8 to 14 days after banding as the tissue sloughs. This is usually self-limiting in nature.[7] In addition, vaso-vagal symptoms, slippage of bands, priapism, difficulty in urination, anal fissure, and chronic longitudinal ulcers are typically considered minor complications. Massive bleeding, thrombosed hemorrhoids, severe pain, urinary retention requiring catheterization, pelvic sepsis, fistula, and death are major complications that are less commonly reported.[15]
Pelvic sepsis after RBL is rare; however, it is a potentially fatal complication.[16] Clinical suspicion must remain high as early intervention is critical. Patients should be educated to seek medical attention if they have increasing pain, fever, or urinary retention, which could be an early indicator of pelvic sepsis. The treatment for pelvic sepsis includes intravenous fluid resuscitation and antibiotics, as well as the removal of the rubber band and possible debridement of necrotic tissue in the operating room. The sepsis must be treated early as the infection can develop into a necrotizing soft tissue infection or Fournier gangrene. Severe bleeding, urinary retention, anal incontinence, and anal stenosis are less likely after rubber-band ligation than operative hemorrhoidectomy.[1]
Clinical Significance
RBL for the treatment of hemorrhoids is easy to do, inexpensive, and has few serious complications. RBL is a widely accepted practice that is generally well tolerated and has demonstrated high success rates with decreased recurrence rates. Multiple studies and clinical trials continue to support this, as shown below:
- RBL has been studied in several large series. One study examining long-term outcomes of RBL included 805 patients who underwent 2114 ligations (median of 2 ligations in each patient).[17] There was a 71% success rate in this cohort. Success rates were similar for all degrees of hemorrhoids. The authors noted a higher failure rate when placing 4 or more bands.
- A meta-analysis of 12 trials reported cessation of bleeding after RBL in up to 90% of patients; 84% of those with grade 3 hemorrhoids reported symptomatic improvement.[13]
- In a substantial case series involving 750 consecutive patients with grade 2 and 3 hemorrhoids, a cure rate of 93% and a recurrence rate of 11% were observed 2 years following RBL, regardless of the hemorrhoid grade.
- A Cochrane review compared the efficacy of RBL and excisional hemorrhoidectomy based on the hemorrhoid grade. The review concluded that for grade 3 hemorrhoids, excisional hemorrhoidectomy was superior to RBL in terms of effectiveness (p = 0.01). However, for grade 2 hemorrhoids, no significant difference was observed (P = 0.32).[18]
Enhancing Healthcare Team Outcomes
Healthcare professionals, including physicians, advanced practitioners, nurses, pharmacists, and other team members, play distinct yet interrelated roles to ensure comprehensive patient-centered care when performing hemorrhoid banding. Physicians and advanced practitioners must exhibit clinical proficiency in diagnosing hemorrhoids, formulating appropriate treatment plans, and performing RBL precisely. Their responsibilities include obtaining informed consent, addressing patient concerns, and offering postprocedure guidance. Nurses are pivotal in educating patients about the procedure, providing preprocedural and postprocedural care, and monitoring patients for potential complications, ensuring patient safety and comfort. Pharmacists ensure the judicious use of medications for pain management and symptom relief. Effective interprofessional communication, encompassing concise information exchange and shared care protocols, is fundamental to harmonizing patient care. Collaborative care coordination aligns each professional's efforts toward optimizing patient outcomes, enhancing patient safety, and fostering cohesive teamwork.
Nursing, Allied Health, and Interprofessional Team Interventions
The following are the outlines of the nursing roles in RBL of hemorrhoids:
- Monitor the patient before, during, and after the procedure
- Monitor the patient in the postoperative period
- Check for bleeding after the procedure
- Assess the patient's pain levels before, during, and after the procedure