Introduction
The acromioclavicular (AC) joint articulates the lateral end of the clavicle with the acromion as it projects anteriorly off the scapula. The AC joint provides stability and motion to the shoulder complex. It is a commonly injured shoulder joint, ranging from sprains to frank tears, occasionally requiring surgery.[1][2]
Structure and Function
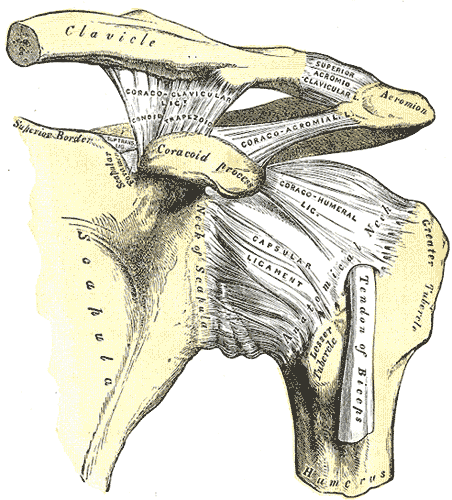
The acromioclavicular joint is a diarthrodial joint defined by the lateral clavicle articulating with the acromion process as it projects anteriorly off the scapula. The AC joint is a plane type synovial joint, which under normal physiological conditions allows only gliding movement. As it attaches the scapula to the thorax, it allows an additional range of motion to the scapula and assists in arm movement such as shoulder abduction and flexion. It also enables the transmission of forces from the upper arm to the rest of the skeleton.
The AC joint is surrounded by a capsule and lined by a synovial membrane. In between the osseous portions lies an intra-articular cartilaginous disk. Lastly, the articulating surfaces are lined with fibrocartilage, as opposed to hyaline cartilage.
Three main ligaments stabilize the joint. The acromioclavicular ligament (AC) has both superior, inferior, anterior, and posterior components. The superior and posterior ligaments are the strongest, and it mainly serves to provide horizontal stability. The coracoclavicular ligaments (CC) complex consists of the conoid and trapezoid ligaments. They insert on the posteromedial and anterolateral region of the undersurface of the distal clavicle, respectively. It mainly serves to provide vertical stability. The coracoacromial ligament is a strong triangular band that connects the coracoid process to the acromion and also provides vertical stability.[3][4][5]
Blood Supply and Lymphatics
Branches from the suprascapular artery, which originates from the subclavian artery, and thoracoacromial arteries, which originates from the axillary artery, form the 2 main blood vessels that provide vascular supply to the acromioclavicular joint.
Nerves
The AC joint is innervated by articular branches of the suprascapular, axillary, and lateral pectoral nerves. These nerves arise from the brachial plexus. Cutaneous innervation to the AC joint is through the sensory branch of the suprascapular nerve. This branch runs superiorly to the supraspinatus muscle towards the AC joint. However, pain arising from the AC joint may be referred to the neck, trapezius, lateral deltoids, and shoulder.
Clinical Significance
Injuries to the AC joint are common. They can present as sprains or dislocations. However, sprains are more common. The most common etiology is direct trauma to the AC joint or lateral trauma providing an axial load on the joint space. This can occur from motor vehicle accidents, sports or accidental trauma. Falling on the outstretched hand or elbow can also cause AC joint injuries. AC joint injuries account for over 40% of all shoulder injuries. Note that AC dislocations are different from “shoulder dislocation,” which refers to the dislocation of the glenohumeral joint.[6]
Patients will generally present reporting pain over the acromioclavicular joint and a mechanism consistent with that injury. They will describe pain over the joint, possibly radiating to the shoulder or neck and made worse with movement or use of the arm. On exam, the provider may observe swelling, bruising, or deformity. There may be tenderness to palpation over the area. There may be limited active or passive range of motion of the shoulder or neck. The examiner should assess for anterior-posterior or superior-inferior mobility and laxity. In dislocations, the deformities may be obvious. It is important to evaluate the entire clavicle and shoulder for additional injuries in addition to performing a full neurovascular examination.
A special test may assist in the evaluation of a suspected AC joint injury. Pain with any of these test may suggest AC pathology. The adduction or cross-arm test has the patient either actively or passively adduct their arm across the body in the axial plane. Pain at the AC joint is a positive test, and it has the greatest sensitivity for AC joint pathology. In performing the shear test, the examiner applies an external force to the AC joint by simultaneously pushing the scapula from a posterior direction and the clavicle from an anterior direction. In the one-handed shear test, also known as Paxinos test, the examiners place their thumb on the posterior acromion and fingers on the mid-clavicle. The examiner then tries to squeeze the thumb and fingers together.
Radiographic evaluation of the acromioclavicular joint is standard for suspected AC-joint injury or undifferentiated shoulder pain in the setting of trauma. Standard AP, lateral, and axillary radiographs should be obtained. If the diagnosis is uncertain, the Zanca view is the most accurate view for examining the AC joint. This is an antero-posterior view with the beam directed at the AC joint with 10 degrees of cephalic tilt. In grade 1 AC joint sprain, which is most common, radiographs will be normal. Disruption of the joint will be seen in grade 2 through 6. If there is continued uncertainty, ultrasound or MRI may be utilized to provide additional diagnostic information.
Dislocations are staged according to the Rockwood classification of acromioclavicular and coracoclavicular joint injuries.
- I: AC ligament sprain; CC ligament intact; no radiographic abnormalities
- II: AC ligament is torn; CC ligament sprain; clavicle elevated but not superior to the border of the acromion, or there is a less than 25% increase in the CC interspace
- III: AC and CC ligaments are torn; clavicle is elevated above the border of the acromion, or there is a 25% to 100% increase in the CC interspace
- IV: AC and CC ligaments are torn; posterior displacement of the distal clavicle into the trapezius
- V: AC and CC ligaments are torn; superior displacement of the distal clavicle by more than 25 mm
- VI: AC and CC ligaments are torn; inferolateral displacement in a subacromial or subcoracoid displacement behind the coracobrachialis or biceps tendon
The prognosis of acromioclavicular joints dislocations is generally favorable. Grade I and II sprains are self-limited and are managed with conservative therapy including a brief period of rest, sling, ice, anti-inflammatory medications, physical therapy, and a graded return to activity. Treatment for grade III dislocations is controversial and is determined based on the occupation of the patient, their goals, and the consulting orthopedic surgeon. Grade IV to VI are rare, but require surgical correction due to the risk of comorbid injuries. Surgically managed injuries have a longer recovery and higher risk of complications.
The most common complications from acromioclavicular joint injuries is residual pain, affecting 30% to 50% of individuals. Primary or secondary osteoarthritis are commonly seen in the acromioclavicular joint. Incidence of AC joint osteoarthritis increases with age. It can be through overuse, chronic degeneration, or through prior trauma (secondary osteoarthritis). This leads to narrowing of the articular disc and degeneration of the cartilage. Osteoarthritis may lead to osteophytic lesions and subacromial impingement and compression of nearby structures.[7][8]