Continuing Education Activity
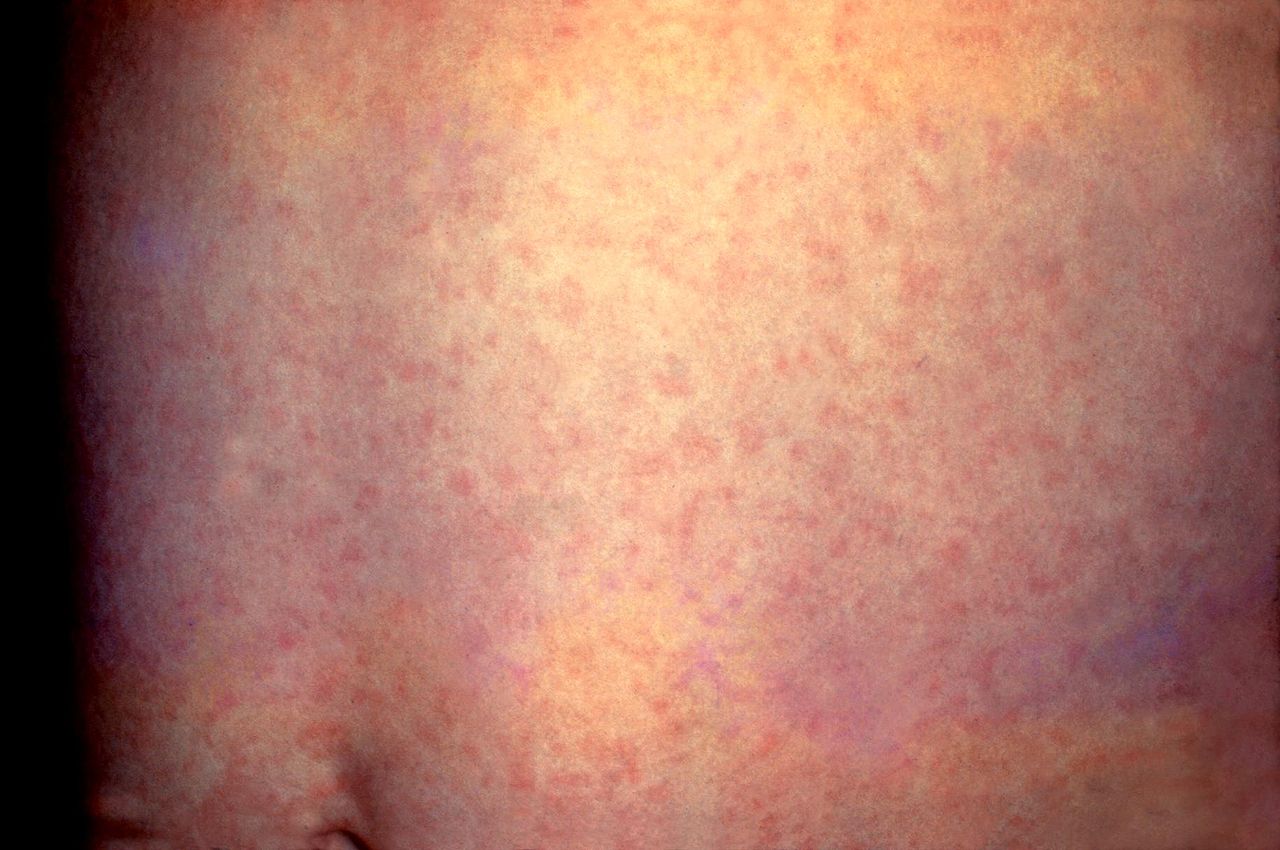
Rubella, also known as German Measles, is a viral illness characterized by maculopapular rash, lymphadenopathy, and fever. It is a highly contagious but generally mild disease, and most cases do not lead to significant consequences. However, maternal infection during the first trimester of pregnancy can cause a fetal malformation syndrome known as congenital rubella syndrome. This activity reviews the presentation and management of congenital rubella syndrome and highlights the critical role of the interprofessional care team in caring for patients with this condition.
Objectives:
- Explain the features commonly noted in patients with congenital rubella.
- Explain how to diagnose congenital rubella.
- Explain how to treat congenital rubella.
- Describe how an optimally functioning interprofessional team would coordinate care to enhance outcomes for patients with congenital rubella.
Introduction
Rubella, also known as German Measles, is a viral illness characterized by maculopapular rash, lymphadenopathy, and fever. It is a highly contagious but generally mild disease, without consequences in most cases. However, maternal infection during the first trimester of pregnancy can cause a fetal malformation syndrome called congenital rubella syndrome.
Etiology
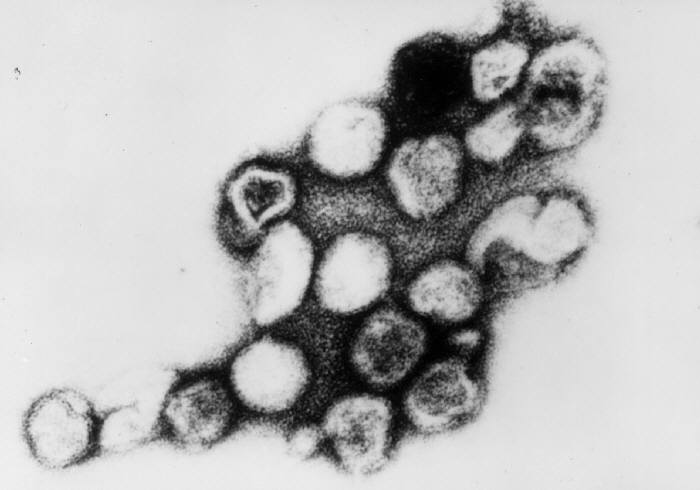
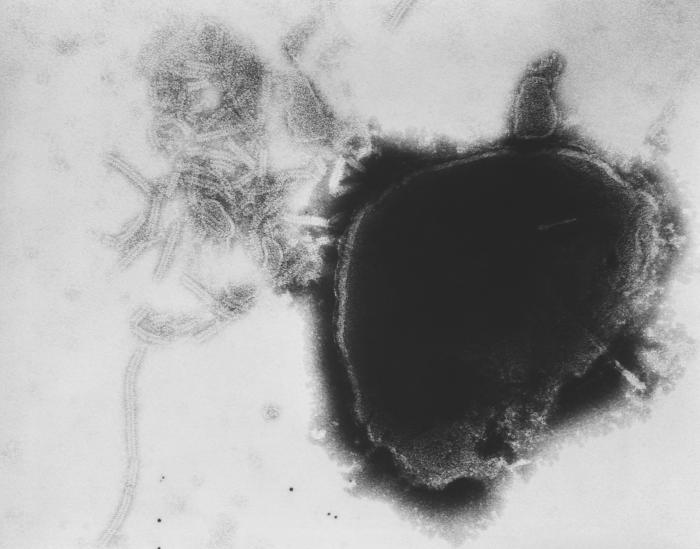
The enveloped, positive-stranded RNA virus known as Rubella virus is classified as a Rubivirus in the Togaviridae family.
Epidemiology
Congenital rubella syndrome is a global public health concern with more than 100,000 cases reported annually worldwide. Natural rubella infection during pregnancy is one of the few known causes of autism.
Before the rubella vaccine was licensed in the United States in 1969, rubella was a common disease that occurred primarily among young children. However, rubella was eliminated from the United States in 2004. Since elimination, fewer than 10 cases have been reported annually in the United States, and most cases were imported from outside the country.[1]
Rubella continues to be a commonly transmitted infection in many parts of the world. Many rubella cases are not recognized, as the rash resembles many other illnesses and up to half of all infections may be subclinical.
Humans are the only source of infection. Transmission is through direct or droplet contact from nasopharyngeal secretions. Once inhaled, the virus replicates in the respiratory mucosa and cervical lymph nodes before reaching the target organs via systemic circulation. The infectious period extends approximately 8 days before to 8 days after the rash onset.[2]
Maternal rubella during pregnancy can cause miscarriage, fetal death or congenital rubella syndrome.[2] Few infants with congenital rubella continue to spread the virus in nasopharyngeal secretions and urine for a year or more. Rubella virus also has been recovered from lens aspirates in children with congenital cataracts for several years.
Pathophysiology
Pathogenesis of congenital rubella syndrome is multifactorial[2] and include the following:
- Non-inflammatory necrosis of chorionic epithelium and in endothelial cells which are then transported to fetal circulation and fetal organs.
- Intracellular actin assembly is inhibited by rubella infection, leading to inhibition of mitosis and restricted development of precursor cells.
- Upregulation of cytokines and interferon in infected cells which could contribute to congenital defects.
History and Physical
Few or no obvious clinical manifestations occur at birth with mild forms of the disease. The incidence of congenital infection with rubella is high during the early and late weeks of gestation (U-shaped distribution), with chances of birth defects much higher if the infection occurs early in pregnancy.
Congenital defects occur in up to 85% of neonates if maternal infection occurs during the first 12 weeks of gestation, in 50% of neonates if infection occurs during the first 13 to 16 weeks of gestation, and 25% if infection occurs during the latter half of the second trimester.
Serious birth defects include the following[3][4]:
- Congenital heart defects (patent ductus arteriosus, peripheral pulmonary artery stenosis, ventricular septal defects, atrial septal defects)
- Auditory (sensorineural hearing impairment)
- Ophthalmologic (cataracts, pigmentary retinopathy, microphthalmos, chorioretinitis)
- Neurologic (microcephaly, cerebral calcifications, meningoencephalitis, behavioral disorders, mental retardation)
- Hematologic (thrombocytopenia, hemolytic anemia, petechiae/purpura, dermal erythropoiesis causing “blueberry muffin” rash)
- Neonatal manifestations (low birth weight, interstitial pneumonitis, radiolucent bone disease leading to “celery stalking” of long bone metaphyses, hepatosplenomegaly)
- Delayed onset of insulin-dependent diabetes and thyroid disease.
Evaluation
Maternal screening with rubella titers in early pregnancy is considered standard of care in the United States. Rubella-like illness in early pregnancy should be evaluated to confirm the diagnosis. Laboratory diagnosis is based on observation of seroconversion with use of RV-IgG and IgM titers. Maternal counseling and termination of pregnancy are options in such cases.
Prenatal fetal diagnosis is based on detection of viral genome in amniotic fluid, fetal blood or chorionic villus biopsies.
Postnatal diagnosis of congenital rubella infection is done by detecting RV-IgG antibodies in neonatal serum using ELISA. This approach has sensitivity and specificity of nearly 100% in infants less than three months of age. Confirmation of infection is made by detection of rubella virus in nasopharyngeal swabs, urine and oral fluid using polymerase chain reaction (PCR).[2]
Congenital infection can also be confirmed by stable or increasing serum concentrations of rubella-specific IgG over the first year of life. It is difficult to diagnose congenital rubella in children older than one year of age.
Postnatal confirmation of congenital infection is important despite the absence of clinical features of congenital rubella syndrome. This is to develop a specific follow-up care plan for early detection of long-term neurological and ocular complications.[5]
Treatment / Management
Prenatal management of the mother and fetus depends on gestational age at onset of infection. If infection happens before 18 weeks gestation, the fetus is at high risk for infection and severe symptoms. Termination of pregnancy could be discussed based on local legislation. Detailed ultrasound examination and assessment of viral RNA in amniotic fluid is recommended.
For infections after 18 weeks of gestation, pregnancy could be continued with ultrasound monitoring followed by neonatal physical examination and testing for RV-IgG.[2]
Limited data suggest a benefit of intramuscular Immune Globulin (IG) for maternal rubella infection leading to decrease in viral shedding and risk of fetal infection.
Although symptoms associated with congenital rubella syndrome can be treated, there is no cure for the syndrome; hence, prevention should be the goal.
Control Measures
Children with congenital rubella syndrome should be considered contagious until at least one year of age unless two negative cultures are obtained one month apart after 3 months of age. Neonates should be isolated. Hand hygiene is of utmost importance for reducing disease transmission from the urine of children with congenital rubella infection.[6][7][8]
Differential Diagnosis
- Parvovirus b19 infections
- Pediatric contact dermatitis
- Pediatric cytomegalovirus infection
- Pediatric enterovirus infections
- Pediatric mycoplasma infections
Pearls and Other Issues
Significant progress has been reported in the prevention of congenital rubella syndrome since the identification of teratogenic potential of rubella virus. However, more efforts are required to eliminate it. Since no treatment is available for congenital rubella syndrome, it is important for women to get vaccinated before they get pregnant. MMR vaccine is a live attenuated vaccine, and due to its theoretical teratogenic risk, women who are pregnant and not vaccinated should wait to get MMR until after they have given birth. Although, several publications have reported the absence of congenital rubella syndrome after vaccination during pregnancy.
The antibody response rate to a single dose is more than 95%; after two doses, the response rate is almost 100%. Rubella vaccine is generally well tolerated with benign adverse effects like fever, rash, and transient lymphadenopathy.
Even though rubella has become a rare disease in developed countries, lack of vaccination may lead to significant public health problems.
Enhancing Healthcare Team Outcomes
Once an infant with congenital rubella is diagnosed, an interprofessional team of nurses and clinicians should be involved in its care because of the diverse manifestations and family education requirements. Children with congenital rubella syndrome should be considered contagious until at least one year of age unless two negative cultures are obtained one month apart after 3 months of age. A birth the Neonate should be isolated. The nurse should emphasize the importance of hand hygiene for reducing disease transmission from the urine of children with congenital rubella infection. More important, all healthcare workers should encourage parents to have their children vaccinated against rubella.