Continuing Education Activity
Phimosis is a term used to describe difficulty retracting the penile prepuce. There are both physiologic and pathologic forms of phimosis, which can complicate the use of the term. The physiologic form is common in children between 2 and 4 years of age, is a self-limiting, and resolves once the foreskin becomes more retractile. The pathologic form is usually due to balanitis xerotica obliterans (BXO), a cicatrizing skin condition histologically identical to lichen sclerosis. BXO has an insidious onset and may be associated with irritation, local infection, dysuria, and bleeding, which can precede atrophy and meatal stenosis. This activity reviews the evaluation, treatment and prognosis of physiologic and pathologic phimosis and highlights the role of an interprofessional team in evaluating and improving care for patients with this condition.
Objectives:
- Review the differences in the presentation of physiologic versus pathologic phimosis.
- Explain when an alternative process should be considered in patients who have been diagnosed with physiologic phimosis.
- Summarize the various differential diagnoses for phimosis.
- Describe the importance of an interprofessional approach to the management and surveillance of patients with phimosis.
Introduction
Phimosis is a term used to describe the difficulty in retracting the prepuce. The term is Greek in origin, with the literal translation of “muzzling.” However, its use interchangeably in several conditions can often lead to the notion of a pathological process where none exists. Often non-retractile foreskin is the presenting complaint of a patient, or their parent/guardian, as such it is best to establish whether the process is physiological or pathological.
Etiology
Physiological Phimosis
At birth, the prepuce is non-retractile and remains so for a variable length of time. First appearing in the eighth week of gestation as an epithelial ridge, by 16 weeks of gestation the prepuce is complete and encases the glans. At this stage, the epithelial lining of the glans and prepuce are contiguous, and these preputial adhesions are essentially a normal developmental process. Separation begins proximally by the process of desquamation with small spaces forming, which eventually coalesce to form the preputial sac.
Pathological Phimosis
The pathological process gives characteristic stenosis scarring and pallor of the preputial opening. It is typically caused by balanitis xerotica obliterans (BXO). BXO is a cicatrizing skin condition histologically identical to lichen sclerosis. It is a chronic skin condition with some evidence suggesting an autoimmune etiology. There has been controversy regarding BXO as a precipitant for penile cancer later in life.
Epidemiology
The natural history of non-retractile foreskin and preputial adhesions was extensively documented in the mid-twentieth century, firstly by Gairdner in 1949 and then Oster in 1968. Their combined studies show that in all but a small proportion of boys the foreskin will be retractile once the boys mature into their teenage years. These studies demonstrated that phimosis is present in 8% of 6- to 7-year-olds, 6% of 10- to 11-year-olds and 1% of 16- to 17-year-old boys. By contrast, preputial adhesions remain much more common throughout childhood and adolescence, but by 17-years of age, only 3% will have persisting adhesions. [1],[2]
VTrue pathological phimosis caused by BXO has a relatively stable incidence across all decades of life, with a spike in the third decade of life. Relatively rare in children under the age of 5, there is a peak childhood incidence between 9 and 11 years of age, with 0.6% of boys affected by years of age. Modern studies are questioning this doctrine, reporting varied incidence from 5% to 52% and children younger than 5 years as having BXO. [3]
Pathophysiology
In physiological phimosis, attempted retraction of the foreskin results in an apparent constriction ring a few millimeters proximal to the preputial orifice. The orifice on retraction has been described as akin to a flower, with a moist supple and unscarred appearance with pouting of the inner mucosa.
In contrast, BXO has a sclerotic constricting band 1 to 2 cm proximal to the distal end, and there may be glans involvement in a diffuse pattern with whitish discoloration of the peri-meatal area and an erythematous area being pathognomonic. [4]
Histopathology
BXO has the following characteristic histological features: hyperkeratosis with follicular plugging, atrophy of the stratum spongiosum with hydropic degermation of basal cells, hyalinosis, and a band-like chronic inflammatory cell infiltrate with the homogenization of collagen. [4]
History and Physical
In physiological phimosis, ballooning of the foreskin is a common presentation in childhood when the foreskin is still non-retractile. Typically occurring between 2 to 4 years of age, it is a self-limiting phenomenon that resolves once the foreskin becomes more retractile. Parents can be reassured that this does not have any effect on the child’s bladder or ability to void. [5]
BXO has an insidious onset; there may be associated irritation, local infection, dysuria, bleeding before atrophy phimosis, and meatal stenosis. The disease can also have a cyclical course with periods of remission. On rare occasions, patients can present with acute urinary retention or nocturnal enuresis from chronic outflow obstruction.
Evaluation
Laboratory tests and radiography are not typically required in the assessment of phimosis, and studies have demonstrated no evidence of obstruction from physiological phimosis. [5]
Pathological phimosis treated with surgery should have any surgically excised skin sent for histology to confirm the diagnosis and exclude any evidence of malignancy.
Treatment / Management
Treatment of physiological phimosis is not indicated, and reassurance and an explanation of the natural history of the healthy non-retractile foreskin should be given to concerned parents. Circumcision is the preferred treatment for pathological phimosis and represents the only absolute indication for this procedure in children.
Alternatives to circumcision are not suitable to treat phimosis due to BXO but are designed to achieve a fully retractile foreskin. These treatments can be particularly useful with patients experiencing balanoposthitis. Topical steroids have been extensively studied, and topical application to the foreskin can render it retractable at an earlier stage. A typical treatment course is 4 to 8 weeks, with regular attempts at retraction during this time. Given the low risk associated with short duration topical steroid use, this can be repeated if necessary. [6],[7]
An alternative surgical approach to circumcision is the preputioplasty; this approach allows preservation of the foreskin. Initially, postoperative appearances are similar to a dorsal slit procedure, but with regular retraction of the foreskin following the procedure, this resolves into a normal retractile prepuce. [8],[9]
Differential Diagnosis
Acute balanoposthitis is a purulent, pyogenic infection of the prepuce and represents the most severe form of posthitis. These conditions lead to erythema and edema of the prepuce. Dysuria is common, and minor bleeding may occur. These episodes typically resolve with antibiotic treatment and require no further intervention unless recurrent episodes occur.
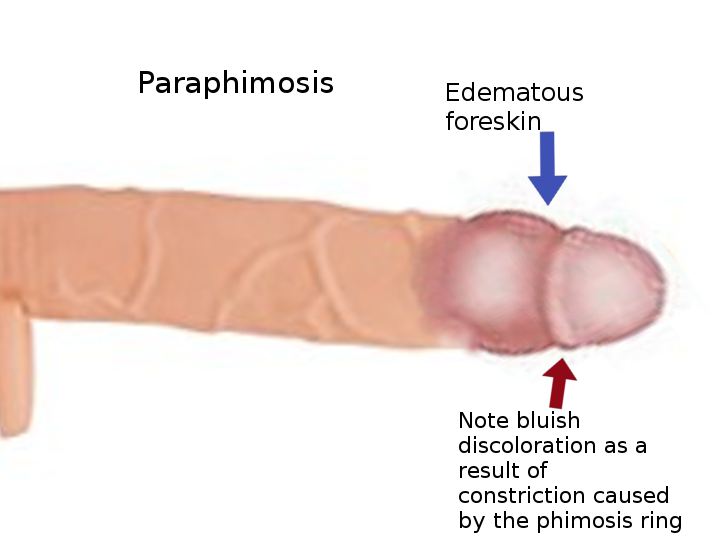
Paraphimosis is related to manipulation of the foreskin with failure to reduce the foreskin to its natural position. Presentation with pain and edema of both the prepuce and the glans is typical. Paraphimosis does not represent a disease process, and single episodes, once resolved, warrant no surgical intervention. Recurrent episodes are unusual and are an indication for circumcision.
Congenital megaprepuce is a rare condition. On examination, the outer preputial skin directly meets the abdominal wall dorsally, the scrotum ventrally with an absence of penile shaft skin. Micturition is always abnormal with the entire preputial sac filling with urine. This can be expressed to leave a more normal appearance. This condition must be treated with a modified circumcision; any attempt to treat this condition with a standard circumcision will result in the requirement for revision surgery complicated by the loss of outer preputial skin.
Preputial adhesions are a normal physiological feature and resolve spontaneously over time [1]. Surgical intervention plays a very minor role except in severe cases.
Pearls and Other Issues
- Although the prepuce is typically non-retractile at birth, physiological phimosis will resolve, resulting in a fully and easily retractable prepuce in approximately 99% of boys by the age of 16.
- Conservative treatment of physiological phimosis involves educating parents and children about the natural history of physiological phimosis.
- Alternatives to circumcision exist for physiological phimosis including topical steroid therapy and preputioplasty.
- Balanitis xerotica obliterans (BXO) remains an absolute indication for circumcision at all ages.
Enhancing Healthcare Team Outcomes
The management of phimosis is an interprofessional. Although the condition is often first seen by the primary caregiver or nurse practitioner, in many cases a referral to a urologist is recommended. Treatment of physiological phimosis is not indicated, and reassurance and an explanation of the natural history of the healthy non-retractile foreskin should be given to concerned parents. Circumcision is the preferred treatment for pathological phimosis and represents the only absolute indication for this procedure in children.
Alternatives to circumcision are not suitable to treat phimosis due to BXO but are designed to achieve a fully retractile foreskin. These treatments can be particularly useful with patients experiencing balanoposthitis. Topical steroids have been extensively studied, and topical application to the foreskin can render it retractable at an earlier stage. An alternative surgical approach to circumcision is the preputioplasty; this approach allows preservation of the foreskin. In most infants and children, the outcomes of phimosis treatment are good.[10] (Level 11)