Continuing Education Activity
Decompression sickness (DCS) occurs when depressurized gas (usually nitrogen) exits the solution phase in tissues and obstructs the circulation by forming bubbles. The settings that can precipitate this condition involve rapid tissue decompression, as happens after a quick ascent from deep-sea diving, emerging from a caisson, flying in an unpressurized aircraft, and performing an extra-vehicular activity in space. Proper decompression can prevent DCS.
Experts have classified the manifestations of this disorder into 3 types. Type I DCS presents with skin, musculoskeletal, or lymphatic involvement. Type II DCS manifests with symptoms of brain or spinal injury. Type III DCS presents with potentially fatal pulmonary complications.
This activity reviews the evaluation and management of Types I and II DCS and highlights the role of the interprofessional team in managing patients with these conditions.
Objectives:
Identify symptoms and signs indicative of decompression sickness in divers or individuals exposed to pressure changes.
Differentiate between types and severity of decompression sickness, categorizing manifestations and their corresponding treatments.
Select suitable treatment modalities based on the severity and clinical presentation of decompression sickness.
Collaborate with hyperbaric medicine specialists and emergency response teams in managing complex cases of decompression sickness.
Introduction
Decompression sickness (DCS) is a potentially life-threatening condition that occurs when dissolved gases (commonly nitrogen) form bubbles in the bloodstream and tissues. This condition predominantly affects individuals who experience rapid ambient pressure changes, such as scuba divers, high-altitude aviators, or individuals working in pressurized environments.
Gases exist in equilibrium with their dissolved forms when the tissues are under pressure, such as during deep-sea diving. A rapid ambient pressure reduction causes dissolved gases to come out of solution and form bubbles within the body. The bubbles can obstruct the blood vessels, trigger inflammation, and damage tissues, resulting in the complications seen in DCS.
DCS may be prevented by following safe diving practices, including appropriate ascent rates, adherence to decompression schedules, safety stops, and conservative dive planning. Treatment typically involves administering high-flow oxygen and, in more severe cases, hyperbaric oxygen therapy (HBOT). Early DCS recognition and intervention and good interprofessional coordination can enhance patient outcomes.
Etiology
DCS arises from a steep ambient pressure fall, causing tissue gases to come out of solution and form bubbles in the circulation. The gas is most commonly nitrogen, the most predominant atmospheric gas and frequently a component of divers' breathing gases. Nitrogen is usually inert but can cause vascular obstruction and inflammation when excessive amounts are introduced into the blood vessels.
Nitrogen's partial pressure increases with sea depth and diminishes with altitude. In the case of divers, prolonged deep-sea diving subjects their bodies to great nitrogen pressure, pushing the gas into the tissues. A slow ascent allows the gradual release of nitrogen from the tissues into the gaseous state. A quick ascent results in rapid decompression and fast evolution of nitrogen gas bubbles in the tissues and circulation. A similar phenomenon happens to aviators ascending into high altitudes in a depressurized aircraft and astronauts working outside a compressed spacecraft.
Individual factors that can increase a person's DCS risk include dehydration, patent foramen ovale, previous injury, cold ambient temperature, high body fat content, and recent alcohol consumption. Type I DCS, also known as the bends, manifests with skin, lymphatic, or musculoskeletal symptoms and is the most common presentation of this condition. Type II DCS involves the nervous system and is associated with right-to-left shunting of venous bubbles.[1][2]
Epidemiology
DCS is rare due to technological improvements and established diving safety protocols.[19] Estimates in sport diving are 3 cases per 10,000 dives. The incidence among commercial divers is higher, ranging from 1.5 to 10 per 10,000 dives. Dive duration and depth correlate with DCS incidence.[3] The DCS risk in males is 2.5 times higher than in females.
Pathophysiology
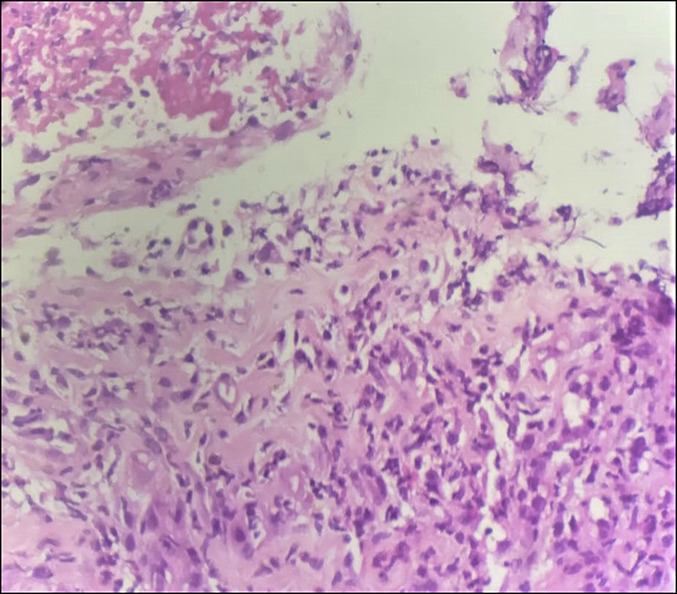
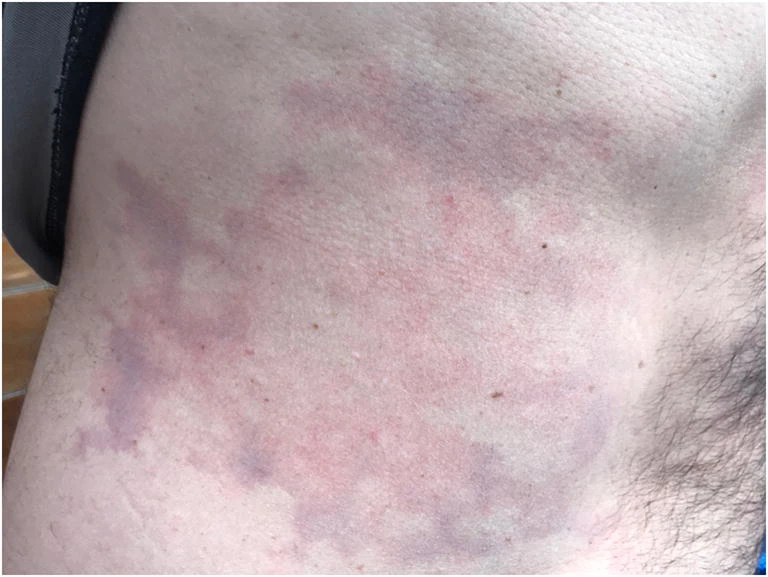
DCS symptoms arise from vascular obstruction and inflammation caused by gas bubbles. Ischemia and inflammation damage most tissues. Pruritic, netlike, red lesions (cutis marmorata) can form in the skin. Bone and joint necrosis manifest as pain in the affected areas. The lymph nodes may be swollen and painful.[3][4]
Vascular obstruction and inflammation can produce transient edema in the nervous system in mild cases. Severe DCS manifests with permanent white and gray matter lesions in the brain and spinal cord.[20]
Isolated inner-ear DCS, ie, inner-ear involvement without overt brain damage, is attributed to slower inert gas elimination in the inner ear than the brain. A slower washout allows more gas to accumulate and form bubbles in the inner ear. Patients at risk are those who switch from a helium-oxygen to a nitrogen-rich breathing gas mixture, which is done to reduce costs. A patent foramen ovale predisposes patients to isolated inner-ear DCS even without switching breathing gases.[21]
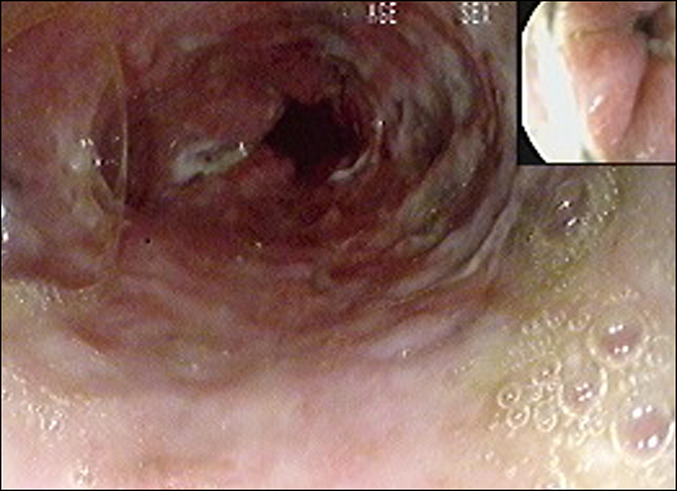
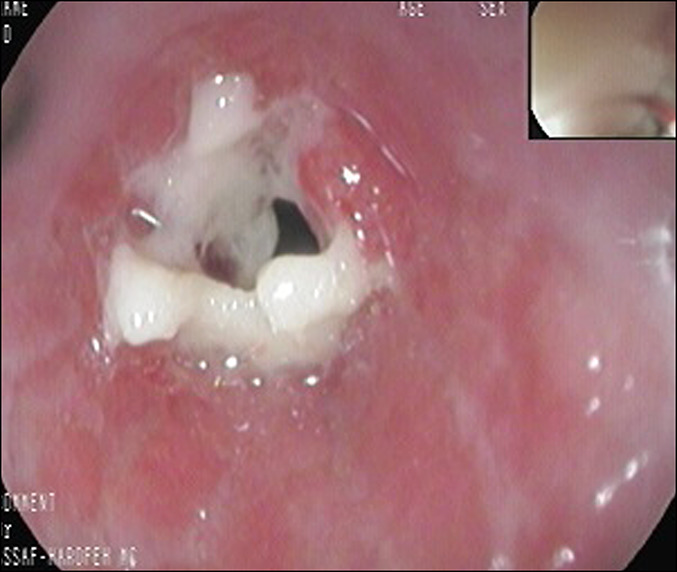
Occasionally, abdominal organs are involved due to vigorous gas decompression in the abdomen. Gut necrosis, pancreatic edema, and liver damage result from bubble formation in the tissues and portal and mesenteric vessels.[22][23]
History and Physical
About 75% of patients with DCS develop symptoms within the first hour after the precipitating event. Providers must perform a quick, focused evaluation and administer initial stabilization measures immediately. High-flow oxygen may be given to patients suspected of DCS, even with normal oxygen saturation. High-flow oxygen can help clear the nitrogen gas pockets in the tissues.
History is consistent with rapid decompression followed by manifestations in the skin, muscles, bones, joints, inner ear, brain, spine, and rarely, lungs within a few minutes to several hours. The shoulder is the most commonly involved joint in type I DCS, though any joint may be affected. Cutis marmorata may be localized or widespread. Patients may present with lymph node swelling and pain.
Type II DCS may have the above symptoms besides headache, visual and hearing impairment, nausea, tinnitus, and poor coordination. Some patients present with altered sensorium.
Rarely, patients with DCS develop abdominal pain, chest pain, or dyspnea, which may signify involvement of the abdomen, mediastinum, or lungs. Pulmonary DCS, also known as chokes, may resemble pulmonary embolism, asthma exacerbation, or myocardial infarction. The condition is potentially fatal if not managed immediately.
On physical examination, patients with DCS may initially have normal vital signs and not be in distress. Localized or generalized skin lesions may be observed. An eye exam may reveal a scotoma. Signs of barotrauma may be seen on otoscopy. A large enough patent foramen ovale will produce murmurs appreciable on auscultation. Extremity examination may reveal joint or muscle tenderness. Nystagmus may be elicited if the inner ear is affected. Depending on the sites involved, focal brain and spinal deficits may present as sensorimotor weakness and deep-tendon reflex abnormalities. Depending on the severity of neurologic damage, patients may be conscious or unconscious.
Pulmonary DCS may present with crackles or rales due to pulmonary edema. Individuals with a history of lung disease, eg, asthma, may have wheezing. Absent breath sounds may be due to pneumothorax, a complication of pulmonary DCS.
DCS is a purely clinical diagnosis. Recompression, if available, may relieve the symptoms immediately and serve as diagnostic confirmation. After giving initial treatment, the provider may take a more detailed history, eg, diving information, and look for other injuries such as wounds and fractures.[5][6]
Evaluation
DCS is a clinical diagnosis. A complete workup is unnecessary and may be detrimental due to the condition's potentially rapid course. However, a chest x-ray must be obtained immediately in a dyspneic patient suspected of pulmonary DCS. Untreated pneumothoraces are an absolute contraindication for HBOT.
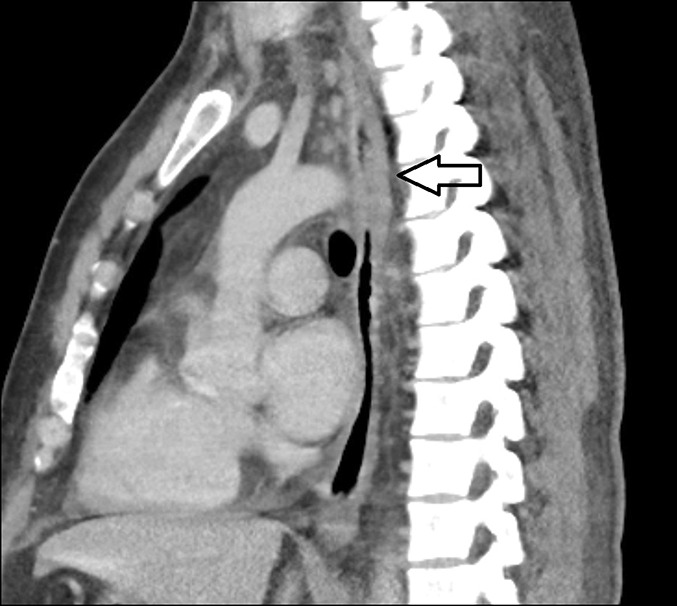
Imaging and laboratory test results are usually nonspecific. Chest radiography is normal in most patients but may show infiltrates or a collapsed lung in individuals with pulmonary DCS. Bone x-ray may show gas bubbles in the joints acutely. However, long-time divers or workers experiencing frequent compression-decompression cycles may have evidence of chronic bone and joint necrosis. Gas inclusions may appear in various abdominal and thoracic structures on computed tomography (CT) or magnetic resonance imaging (MRI). Brain and spinal CT and MRI may show edema, infarcts, intracranial hemorrhages, or gas pockets in CSF spaces. An echocardiogram may reveal a patent foramen ovale.
Lab results may be consistent with renal, hepatic, and pancreatic damage if abdominal organs are involved. C-reactive protein and white blood cell count may also be elevated.
Treatment / Management
Cardiovascular resuscitation must be administered to unconscious patients with no pulse or respiration, regardless of the cause. Patients suspected of DCS must be given 100% oxygen until HBOT is available. Providers must initiate intravenous fluid administration and continuous cardiac monitoring. A chest x-ray must be obtained as soon as possible to rule out pneumothorax and prepare the patient for HBOT. Recompression by HBOT must be initiated immediately. U.S. Navy protocols are widely adopted for this treatment.[24]
Evacuation by a pressurized aircraft is recommended for patients needing immediate transport to a definitive treatment center. An unpressured air vehicle, such as a helicopter, may be used as long as the altitude is limited to 300 meters or 1000 feet.
Conscious patients may be given oral fluids and electrolytes unless immediate abdominal or thoracic surgery is considered. Patients with delayed neurologic, pulmonary, or dermatologic symptoms may still benefit from HBOT. Deep venous thrombosis and thrombotic pulmonary embolism may be prevented in nonambulatory patients by administration of low-molecular-weight heparin. Other anticoagulants, non-steroidal anti-inflammatory drugs, and steroids are no longer recommended in DCS treatment. Aspirin can mask pain and other symptoms.
The patient must be placed upright or have their head elevated if vomiting occurs to prevent aspiration. The Trendelenburg and left lateral decubitus positions are no longer recommended for extended periods as they increase the risk of cerebral edema.
Differential Diagnosis
The following conditions may be confused with DCS Type I in patients presenting with musculoskeletal pain, skin rashes, and lymph node swelling:
- Systemic viral illness
- Systemic lupus erythematosus
- Acute leukemia
- Bacterial illnesses such as gonorrhea and syphilis
- Lymphoma
- Lyme disease
- Dehydration
On the other hand, DCS Type II may be confused with the following:[7][8]
- Inner ear barotrauma
- Stroke
- Drowning
- Thermal stress
- Nitrogen narcosis
- Meningococcemia
- Intracranial and intraspinal masses
- Multiple sclerosis
- Hypoglycemia
- Acute coronary syndrome
- Marine life toxin exposure
- Oxygen toxicity
A rapid, focused evaluation is the provider's primary tool to distinguish between these overlapping conditions and instituting treatment promptly.
Pertinent Studies and Ongoing Trials
Improving the models for predicting DCS risk is an ongoing area of research. Programming better models into dive computers and diving decompression tables can reduce DCS incidence and outcomes.[9][10]
Dive computers monitor depth, time, and dive profiles. Integrating advanced predictive models into dive computers allows for real-time nitrogen uptake and elimination calculations when diving. These models provide more accurate decompression profiles and alert divers about potential DCS risks.
On the other hand, diving decompression tables serve as guides for ascent rates and decompression stops. Advanced predictive models are continuously refined and incorporated into these tables to create safer dive profiles.
Treatment Planning
On-site interventions must be considered when treatment delay, transportation difficulties, and limited access to a recompression facility are anticipated. Immediate oxygen treatment, ie, within 4 hours of surfacing, improves outcomes and decreases recompression treatments. In-water recompression (IWR) on oxygen at a depth of 9 meters is one option that has shown success in the previous years. However, the procedure may cause oxygen-induced neurotoxicity, seizure, and subsequent drowning, so highly trained providers must administer it.[25]
The standard of care for DCS is the US Navy Treatment Table 6, with oxygen at 18 meters. Depending on patient presentation and oxygen availability, hyperbaric chamber treatment protocols for DCS differ.
Prognosis
The prognosis for DCS varies based on several factors, such as symptom range and severity, treatment promptness and adequacy, and individual health considerations. The prognosis of the condition is generally favorable for patients with mild symptoms, given timely and appropriate treatment, and in excellent health before the dive. Symptoms may resolve within days after prompt administration of high-flow oxygen and rest.
Poor prognostic factors include severe systemic symptoms, treatment delay, and poor baseline health. Long-term neurologic complications and death may result from delayed or inadequate recompression.
Complications
DCS can affect any organ system. Dermatologic lesions such as cutis marmorata and ulcers may heal without permanent sequelae, but the following complications may develop in other areas:
- Osteonecrosis, which may lead to bone fractures and chronic arthritis. The most commonly affected regions are the proximal femur, humerus, and tibia.[26]
- Permanent strokelike symptoms ranging from sensorimotor weakness to incontinence and comatose may result from severe neurologic damage.
- Survivors of pulmonary DCS may develop pulmonary fibrosis.
- Abdominal involvement may result in pancreatic, hepatic, and renal impairment. Gastrointestinal strictures may result in obstruction.
Early administration of high-flow oxygen and HBOT can reduce the severity of these complications.
Postoperative and Rehabilitation Care
Rehabilitation following DCS addresses the residual complications of the illness, which vary individually based on symptom severity, overall health, and treatment response. About 85% of DCS cases are Type I, with most patients recovering uneventfully. These individuals may benefit from medical follow-up, education about DCS prevention, and continued monitoring. Psychological support may be given if necessary or upon patient request.
People with more severe or widespread symptoms may require physical therapy, neurorehabilitation, occupational therapy, and nutritional guidance besides the above post-treatment recovery measures. Physical therapy revolves around improving joint mobility, strength, and flexibility. Neurorehabilitation focuses on regaining motor skills, coordination, and sensory function. Occupational therapy enhances the patient's functional independence and activities of daily living so they can resume normal activities. Nutritional guidance must be tailored to the patient's baseline health and physical progress. Patients may also benefit from counseling to help them recover from psychological trauma and cope with complications.
Deterrence and Patient Education
Efforts to prevent DCS must come from different parties. Individuals must comply with safe ascent protocols, schedule dives or flights appropriately, and limit dive or flight profiles according to their training. Inexperienced divers and pilots must attempt difficult tasks only in the presence of a highly experienced instructor. Hydration, body conditioning, adequate rest, alcohol avoidance, and proper gear maintenance allow them to stay alert and have better muscle control.[11]
Providers must emphasize the importance of the above measures when counseling patients engaging in activities that make them vulnerable to DCS. Clinicians must also remind patients to seek help immediately if they notice unusual symptoms after a dive or altitude exposure. Besides patient education, medical practitioners can help prevent DCS by careful patient screening. A patent foramen ovale, pre-existing lung disease, and poor physical conditioning can predispose individuals to severe DCS manifestations.[12][13]
Dive center owners may also help prevent DCS by regularly updating and maintaining diving equipment and computers. Dive operators must consider requiring medical clearance from prospective divers and having a medical team on-site. A protocol for transporting patients with DCS to the nearest recompression facility or emergency department must be established.
The community may contribute to DCS prevention by disseminating information, providing logistical and medical support, and promoting safe diving and flying practices.
Pearls and Other Issues
The following are the key points regarding DCS management:[14][15][16]
- Prevention is the best way to deal with DCS. Preventive efforts start with the individual, healthcare provider, dive operator, and community members.
- Early recognition is critical to management. Patients must be reminded to seek medical attention immediately if they notice unusual symptoms after a rapid decompression.
- Patients suspected of DCS may be given high-flow oxygen initially and HBOT definitively. Associated injuries must be investigated and appropriately treated.
- Recovery and prognosis depend on the extent of organ involvement, timing and adequacy of treatment, and baseline patient health status.
DCS is a purely clinical diagnosis with potentially grave complications if not addressed on time. The condition must be seen as emergent until proven otherwise.
Enhancing Healthcare Team Outcomes
The DCS multidisciplinary team comprises health professionals trained to recognize the condition quickly, provide immediate treatment, and help the patient resume normal routines. The members include the following:[17][18]
- Emergency medical technicians who may be the first rescuers
- Providers trained in emergency medicine and hyperbaric therapy
- Medical intensivists if the patient needs intensive care after initial treatment
- Specialists such as neurologists, pulmonologists, surgeons, gastroenterologists, nephrologists, hepatologists, and cardiologists may be consulted for specific complications
- Radiologists who can interpret imaging tests
- Nurses who will help coordinate care and educate patients
- Respiratory therapists who will administer respiratory care
- Pharmacists who can prepare and manage medications and ensure the right doses and formulations
- The rehabilitation team—composed of the physical therapist, occupational therapist, neurorehabilitation specialist, nutritionist, and psychological therapist—will help the patient transition to full recovery
- Primary care provider who will see the patient for outpatient follow-up
If a facility is not fully equipped to manage DCS, the Divers' Alert Network can provide referrals to hyperbaric facilities and 24/7 consultation with hyperbaric medicine-trained physicians. DAN's emergency hotline is +1-919-684-9111.