Introduction
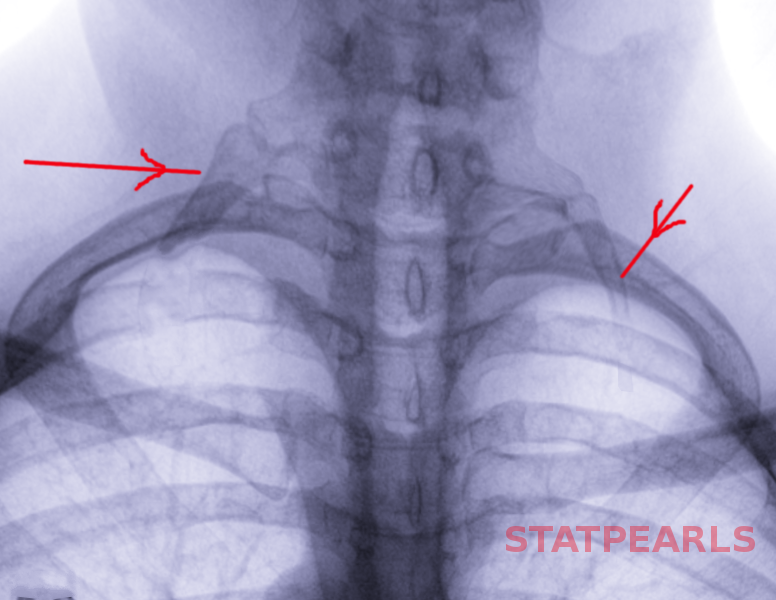
A cervical rib, also known as a "neck rib" or "supernumerary rib in the cervical region," is a congenital overdevelopment of the transverse process of a cervical spine vertebra. Cervical ribs tend to occur in approximately 0.5 to 1% of the population. They are commonly attached to the seventh cervical vertebra. They vary in size, shape, attachment sites, and can occur unilaterally or bilaterally. Most cervical ribs go unnoticed throughout life and are clinically irrelevant. However, in some cases, they can cause localized pain and compress surrounding structures, leading to necessary intervention.
Structure and Function
The cervical rib typically consists of a head, neck, and tubercle. It is attached posteriorly to the first rib by a fibrous band near in the insertion of the anterior scalene muscle. Cervical ribs must articulate with the transverse process to be considered a rib. Unilateral cervical ribs are found more frequently on the left side than the right side. Unilateral cervical ribs occur more frequently than bilateral cervical ribs.
There are four types of cervical ribs:
- Type 1: Complete rib that articulates with the first rib or manubrium
- Type 2: Incomplete rib with a free distal tip
- Type 3: Incomplete rib with a distal fibrous band attachment
- Type 4: Short piece of bone extending beyond the C7 transverse process
There is no physiological function of a cervical rib.
Embryology
The skeletal system originates from the mesoderm. The paraxial mesodermic cells give rise to somites on both sides of the neural tube and further subdivide into a ventral, sclerotome, and a dorsal, dermatome. The cells of the sclerotome convert into mesenchymal cells which will develop into future ribs. These cells are guided into the proper location by Hox genes and growth differentiation factor 11 (GDF11). Mutations in these genes have been thought to lead to abnormal development and patterning of ribs [1].
During early development, the costal element of the developed mesenchymal cells located in the incorrect place usually atrophy but when they fail to do so, they become ossified and present as an elongated transverse process or a complete rib. However, in some cases, it may be too small to reach the sternum and fuses anteriorly with T1 below the first rib.
Blood Supply and Lymphatics
After nerve compression, the next most common manifestation of a symptomatic cervical rib is compression of the subclavian artery. Subclavian artery compression is ordinarily associated with complete cervical ribs more often than incomplete ribs. Compressing the subclavian artery may lead to diminished distal pulse, prolongation of capillary refill, discoloration and decreased temperature of the distal upper extremity, and in severe cases, gangrenous changes at the fingertips [2]. A positive Adson test during hyperabduction of the shoulder is indicative of compression of the subclavian artery by a cervical rib.
Nerves
The presence of a cervical rib may also cause neurological manifestations. Incomplete cervical ribs, more often than complete cervical ribs, most commonly affect the inferior trunk of the brachial plexus, consisting of the C8 and T1 nerve roots [3]. This compression causes weakness in the motor strength of the muscles of the hand and forearm and can lead to clawing of the middle, ring, and little fingers. To correctly diagnose brachial plexus compression due to cervical ribs, one must rule out compression of the nerves in other locations including, carpal tunnel syndrome, ulnar nerve entrapment, and cervical disc herniation.
Muscles
The scalene muscles, in addition to cervical ribs, may cause thoracic outlet syndrome. A scalenectomy may be indicated during some instances of cervical rib resection.
Physiologic Variants
A cervical rib can be unilateral or bilateral; they most commonly present as an overdevelopment of the lateral process of the C7 vertebra. Nevertheless, there have been documented cases of cervical ribs originating from C5 and C6, as well as, multiple levels of cervical ribs.
Surgical Considerations
After conservative management of thoracic outlet syndrome due to cervical rib fails, surgical intervention is necessary. The mainstay of therapy is complete resection of the rib; the surgical approach is what varies. The most common approaches are the supraclavicular and transaxillary approaches with or without a first rib excision or scalenectomy [4]. A posterior approach may also be an option for specific indications.
The supraclavicular approach is primarily the preferred approach for arterial compression. It allows easy access to the proximal subclavian artery for visualization and control in the event of arterial aneurysm or stenosis along with the cervical rib compression. The supraclavicular approach limits the muscles and facial structures that have to be dissected to reach the cervical rib. Also, scalenectomy and removal of osseous and myofascial abnormalities are simplified — functional recovery results in almost all patients.
The transaxillary approach is the most common approach used but is reserved for subclavian/axillary venous occlusion or neurological compression. The advantage of using this approach is there is less manipulation of the brachial plexus and associated nerves, thus reducing perioperative complications [5]. The scar is less noticeable and less painful than the supraclavicular approach. Even muscular or obese patients can be candidates for access from the axilla.
The posterior approach is the choice during re-operation for decompression of the brachial plexus and vascular structures. The rib is removed posteriorly behind the nerve root with the arm adducted, thus limiting any contact between the rib and the nerve.
Resection of cervical ribs for thoracic outlet syndrome is considered a safe and effective procedure. The majority of short-term and long-term outcomes are promising, and the recurrence of symptoms is almost non-existent [6]. Of note, the first rib might have to undergo resection in conjunction with the cervical rib. There is no evidence for increased morbidity or mortality in patients who had both ribs removed in comparison to just the cervical rib.
Clinical Significance
In the majority of cases, cervical ribs are discovered incidentally on a chest or cervical X-ray. In rare cases, individuals may complain of symptoms caused by compression of local structures including the lower brachial plexus, subclavian artery, or subclavian vein; this is thoracic outlet syndrome. In the majority of thoracic outlet syndrome cases, neurological manifestations are the chief complaint. The result is numbness and tingling sensation in the little and ring finger in the distribution of the ulnar nerve (nerve roots C8 and T1). When the subclavian artery is compressed, the individual will experience diminished pulse and change of color and temperature in the affected arm. When the subclavian vein is compressed, the affected limb will be swollen and blue, as blood cannot return to the heart.
Cervical ribs are usually detected in middle-aged adults. Factors that predispose individuals to symptoms are trauma, overuse and poor posture. The compression of these structures by the cervical rib is usually against the scalene muscles. When the subclavian artery is compressed, turning the neck on the contralateral side may result in the loss of pulse in the affected arm (Adson maneuver). CT scan, nerve conduction studies, and an MRI may be needed to assess thoracic outlet syndrome further. Treatment of nerve compression is physical therapy. When conservative treatment fails, one may need to remove the cervical rib and excise the scalene muscles. A bypass graft may be required if the subclavian artery is completely occluded.
To be noted, in patients with abnormalities in Hox gene expression leading to cervical anomalies, the mutation has also been linked to oncogenesis. Germ cell tumors, astrocytoma, and acute lymphoblastic leukemia (ALL) were diagnosed in children with a higher rate of cervical rib and other cervical anomalies [7].