Continuing Education Activity
Streptococcus pyogenes is a major human-specific bacterial pathogen that causes a wide array of manifestations ranging from mild localized infections to life-threatening invasive infections. Ineffective treatment of S. pyogenes infections can result in the postinfectious sequela acute rheumatic fever and post-streptococcal glomerulonephritis. Moreover, it causes invasive infections like necrotizing fasciitis and toxic shock syndrome that is associated with and high morbidity and mortality. This activity describes the bacterium Streptococcus pyogenes (S. pyogenes) and reviewed the epidemiology, clinical manifestations of S. pyogenes infections, evaluation, and management of clinical infections caused by S. pyogenes.
Objectives:
- Identify the etiology of S. pyogenes.
- Outline the appropriate history, physical, and evaluation of Streptococcal pharyngitis.
- Review the management options available for Streptococcal pharyngitis.
- Describe the interprofessional team strategies for improving care coordination and communication to improve the outcome of severe invasive infections caused by S. pyogenes.
Introduction
Streptococcus pyogenes is a major human-specific bacterial pathogen that causes a wide array of manifestations ranging from mild localized infections to life-threatening invasive infections.[1] Ineffective treatment of S. pyogenes infections can result in the postinfectious sequela acute rheumatic fever and post-streptococcal glomerulonephritis. Moreover, it causes invasive infections like necrotizing fasciitis and toxic shock syndrome that is associated with and high morbidity and mortality.
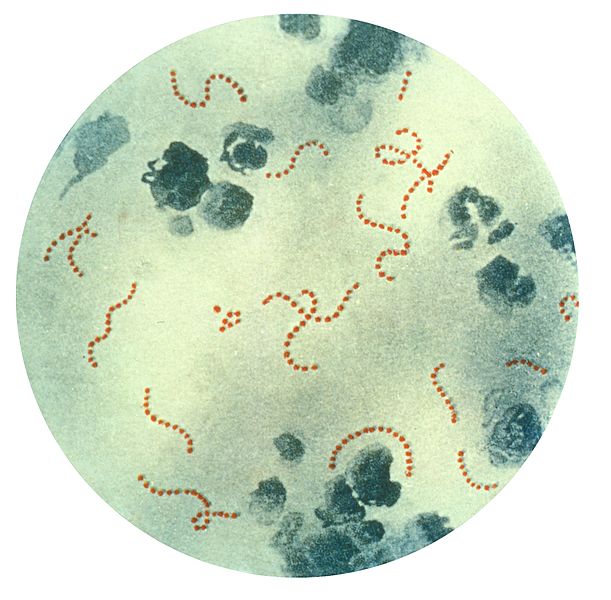
Streptococci are gram-positive, catalase-negative, coagulase-negative cocci that occur in pairs or chains. They are divided into three groups by the type of hemolysis on blood agar: beta-hemolytic (complete lysis of red cells), a hemolytic (green hemolysis), and gamma-hemolytic (no hemolysis). Beta-hemolytic streptococci are characterized as group A streptococci (Streptococcus pyogenes) and group B streptococci (Streptococcus agalactiae).
Etiology
S. pyogenes is a gram-positive, catalase-negative, oxidase negative, β-hemolytic streptococci. It is a facultative anaerobe, grows best in 5 to 10% carbon dioxide, and forms pinpoint colonies on blood agar plates. Lancefield serological grouping system is used to differentiate group A streptococci (GAS) from other streptococci. The type A antigen of S. pyogenes is a polysaccharide which comprised of N-acetylglucosamine attached to a rhamnose polymer backbone.[2] M protein is the major surface protein presents on S. pyogenes cell wall, and GAS strains are further divided into different serotypes based on the antigenic characteristics of the M protein. More than 80 different serotypes have been identified on the basis of M protein.[2]. Depending upon the postinfectious sequelae, S. pyogenes are categorized into two classes: Class I and Class II. Class I strains cause rheumatic fever while class II strains result in acute glomerulonephritis.[3]
S. pyogenes usually colonizes, pharynx, anus, and genital mucosa. Infections caused by S. pyogenes are highly contagious. Transmission can occur through airborne droplets, hand contact with nasal discharge or with objects or surfaces contaminated with bacteria, skin contact with contaminated lesions, or contaminated food sources. GAS Strains may acquire access to the skin via abrasions and skin lesions and may lead to erysipelas or cellulitis.[2] GAS can cause infection in muscle and fascia resulting in myositis and necrotizing fascitis usually following a mild trauma and can result in toxic shock syndrome. S. pyogenes can cause the infection of the vaginal mucosa and uterus causing septicemia.[2] Skin lesions have been identified as the most common predisposing factor for severe S. pyogenes infections.[4] Crowded settings like military camps, nursing houses, and schools cause ease of transmission of the organism and result in epidemics of group A streptococci infection.
Epidemiology
The frequency of the infections caused by S. pyogenes varies in different parts of the world, depending upon clinical manifestations of the infections. GAS has always been associated with serious diseases that result in high morbidity and mortality. GAS infections declined by the mid of the 20th century. However, by the end of 1980, severe group A streptococcus (GAS) infections remerged.[5] Over the last two decades, non-suppurative and suppurative complications of the S. pyogenes infection have increased. This increase in disease burden can be attributed to the multitude of factors including, change of virulence and resistance to antibiotics.[6][7] GAS infections and its complications vary between poorly developed and well-developed countries. In under-developed countries, the prevalence of rheumatic heart disease (RHD) and the incidence of deaths associated with RHD are high. Conversely, in well-developed countries, the incidence of deaths due to invasive GAS infection is high.
The global burden of severe S. pyogenes infections is 18.1 million cases, with 1.78 million new cases per year. The worldwide prevalence of RHD is at least 15.6 million cases, with the incidence of 282,000 new cases per year. Approximately 233,000 deaths per year are attributed to RHD. Each year approximately 663,000 new cases of invasive GAS disease have been reported with 163,000 deaths per year.[8] 616 million cases of sore throat infection worldwide per year can be attributed to S. pyogenes; also, 111 million cases of skin infection in children of developing countries. [1]. In the United States, 15% to 30% of cases of pharyngitis in children and 5% to 20% pharyngitis cases per year in adults are due to S. pyogenes. Moreover, the resurgence of cases of ARF in the children of middle class families of the United States has been observed.[9]
Throat infection is more common in temperate areas, and its incidence increases in late winter and early spring. Impetigo is more prevalent in children of humid climates. It has also been observed that the severity of invasive skin infections caused by GAS escalated from January to April and correlates with the host susceptibility to acquiring a serious infection.[10]
Toxicokinetics
Multiple virulence factors are responsible for clinical manifestations of the S. pyogenes. Bacterial capsule consisted of hyaluronic acid provides protection against phagocytosis. M protein, lipoteichoic acid, and protein F are responsible for the attachment of the bacteria to host cells. M protein is also responsible for inhibiting opsonization by binding to complement regulators and to fibrinogen. M protein is the most important virulence factor for S. pyogenes since experiments have shown that M mutants cannot survive in phagocyte-containing human blood.[11] S. pyogenes also produce exotoxins, like a pyrogenic (erythrogenic) toxin, which is responsible for the rash of scarlet fever and toxic shock syndrome. Other virulent factors include streptokinase, streptodornase, hyaluronidase, and streptolysins, which help in the invasion of tissues.
History and Physical
History and physical findings will vary depending upon the type of infection acquired; nonetheless, an accurate history and proper clinical evaluation are required to reach an accurate clinical diagnosis of S. pyogenes infection.
Sore throat is usually a major complaint in the case of streptococcus pharyngitis. The most common clinical findings for Streptococcal pharyngitis include sudden onset of fever, malaise, pharyngeal exudate, tender cervical lymphadenopathy and, enlarged tonsils.[12]
In children, impetigo is one of the most common skin infections. S. pyogenes cause non-bullous impetigo. Typically the itchy reddish rash appears around mouth or nose that becomes fluid-filled blister later on. Blisters rupture easily and are covered with honey-colored crust. The lesions are usually well-localized and affect exposed areas of the body: face and lower extremities. There are typically no systemic manifestations of the impetigo.
Patient with scarlet fever usually presents with high-grade fever, sore throat, strawberry-like tongue, and a blanchable, papular, non-confluent rash. The rash typically lasts for 7 to 10 weeks, follows by desquamation. Desquamation can only be observed on the palms and soles.[13]
Soft tissue invasive infections due to S. pyogenes mostly present with shock and multiorgan failure.
Necrotizing fasciitis due to group A streptococcus (S. pyogenes) is a deep-seated infection of the subcutaneous tissue that causes rapid destruction of fascia and fat. Systemically or locally immunocompromised individuals are at increased risk for developing necrotizing fasciitis. Other risk factors include surgical procedures, burns, blunt trauma, minor laceration, and childbirth. Localized pain, necrosis of the infected skin lesion, swelling, redness, edema, increased heart rate, and fever are the typical manifestations of necrotizing fasciitis. In the advanced stage of the disease, a picture of septic shock can be present.[14]
Evaluation
Streptococcus pyogenes, also known as group A streptococcus (GAS) is a leading cause of pharyngitis in children and adolescents. Clinicians should use clinical and epidemiological findings to determine the likelihood of GAS pharyngitis. Infectious Disease Society of American (IDSA) recommends that a rapid antigen detection test (RADT) should be used as the first-line measure to assist the clinicians in the diagnosis of GAS pharyngitis. It is recommended to obtain throat cultures in children with negative RADT results to prevent the development of complications.[15] A combined approach using validated clinical criteria such as modified Centor score or the FeverPAIN score along with RADT is an effective strategy to reduce the cost of unnecessary testing and unwarranted antibiotics.
The gold standard test for the detection of GAS is throat culture; however, it is not cost-effective and can delay the treatment.[16] The pyrrolidinyl arylamidase activity (PYR) test is used to distinguish S. pyogenes from other beta-hemolytic streptococci and tests for the presence of the enzyme pyrrolidinyl aminopeptidase.
Anti-streptolysin O (ASO) and anti-DNase B (ADB) titers indicate the previous streptococcal infection and can be used for the diagnosis of post-streptococcal complications.
Treatment / Management
The drug of choice for treatment of bacterial pharyngitis is oral penicillin for 10 days or IM benzathine penicillin. This treatment is cost-effective and has a narrow spectrum of activity.
In patients with penicillin allergy, macrolides and first-generation cephalosporins can be used.[17][18] However, some strains of S. pyogenes have developed resistance to macrolides and macrolides are used as third-line of treatment for Streptococcal throat infection.[19]
Severe invasive S. pyogenes infections can be treated with vancomycin or clindamycin.[20] Intravenous antibiotic therapy and surgery for the removal of necrotic tissue are recommended in the case of soft tissue skin infection by S. pyogenes.
Differential Diagnosis
Streptococcal pharyngitis should be differentiated from throat infections due to parainfluenza virus, rhinovirus, coxsackievirus, adenovirus, etc), Mycoplasma species, Corynebacterium diphtheria, and Epstein-Barr virus.
Scarlet fever can be confused with measles and rubella. However, the absence of symptoms of upper respiratory tract infection and confluent rash in measles can help to differentiate these diseases.
Impetigo by S. pyogenes needs to be differentiated from impetigo infection by staphylococcus aureus. S. pyogenes cause non-bullous impetigo while S. aureus leads to bullous impetigo.
Prognosis
According to a report of the World Health Organization (WHO) GAS is the ninth leading infectious etiology of human mortality. The majority of deaths are due to invasive infections and RHD, especially in third world countries.[8] Severe GAS infections are high in affluent countries ranging from 14% to 19%.[21] Streptococcal pharyngitis typically resolves in 7 to 10 days. However, poor compliance with treatment can result in post-infection complications.
Complications
Complications of S. pyogenes infections can be divided into suppurative and non-suppurative complications.
Suppurative complications include peritonsillar abscess, peritonsillar cellulitis, retropharyngeal abscess, otitis media and sinusitis, uvulitis, cervical lymphadenitis, meningitis, and brain abscess, arthritis, endocarditis, osteomyelitis, and liver abscess.
Non-suppurative complications are rheumatic fever, post-streptococcal glomerulonephritis, PANDAS (pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections), Sydenham chorea, and other autoimmune movement disorders.[19]
Deterrence and Patient Education
Patients must be counseled about the importance of completing the course of antibiotics. They should be advised to follow up with a health care provider and to maintain personal hygiene. The act of handwashing can severely decrease the chance of acquiring skin infections due to S. pyogenes.
Pearls and Other Issues
Ineffective treatment of skin or pharyngeal infection with group A streptococcus leads to acute rheumatic fever. Prevention of recurrent episodes of ARF and the development of potential serious outcomes of rheumatic heart disease require secondarily prophylaxis of penicillin. Secondary prophylaxis is the most effective method of reducing the incidence of ARF and RHD. Nevertheless, primary prophylaxis is gaining popularity throughout the globe. Primary prevention comprises of prompt treatment of streptococcal throat or skin infection via a single injection of benzathine penicillin or oral penicillin for 10 days after confirmation of S. pyogenes infection. Not only does prompt antibiotic treatment reduce the burden of ARF, but it also reduces the incidence of suppurative complications like otitis media.
Enhancing Healthcare Team Outcomes
While the general health care provider is almost always involved in the care of patients with streptococcal infection, caring for patients with the severe streptococcal disease, it is important to consult with an interprofessional team of specialists that include a general surgeon, plastic surgeon, radiologist, infectious disease, and speciality trained nurses.
Necrotizing fasciitis is a life-threatening condition, and due to the complexity of this disease, a team approach is required. Since necrotizing fasciitis is a surgical emergency, it is required that the patient should be admitted to a surgical intensive care unit, where the medical staff is skilled in performing debridement and, if needed, reconstructive surgery. Emergent surgical consultation is required to explore and debride the necrotic tissue. In addition, surgical exploration identifies the aetiology and extent of necrosis. CT and MRI may be helpful to locate the primary foci of infection. Hemodynamic stability should be maintained.
In patients with toxic shock syndrome, monitoring of cardiac output is important. Due to the high incidence of acute respiratory distress syndrome (55%) in patients with severe Streptoccoal soft tissue infection, intubation, and ventilatory support are needed. Greater than 50% of patients with severe soft tissue infections can develop acute renal failure; hence, dialysis may be needed.