Continuing Education Activity
Osteochondritis dissecans of the knee is a relatively rare condition, categorized as a form of osteonecrosis that affects the subchondral bone. The condition tends to manifest as knee dysfunction and pain, predominantly affecting school-aged children and adolescents. More specifically, in osteochondritis dissecans, a piece of the subchondral bone and articular cartilage detaches from the underlying bone. The ensuing fragment may be either stable, indicating intact overlying articular cartilage, or unstable, which has significant prognostic implications. Osteochondritis dissecans is more prevalent in individuals aged 10 to 20, with a higher incidence in males than females. Juvenile osteochondritis dissecans occurs in patients with open growth plates or physes, whereas osteochondritis dissecans in adults applies to skeletally mature patients.
The exact cause of osteochondritis dissecans remains unclear, and individuals with this condition may either present with knee pain as a primary complaint or incidentally discover the findings during radiographs conducted for unrelated injuries. Clinicians typically rely on plain radiographs to diagnose and identify the condition, with magnetic resonance imaging as the primary staging tool. Over 50% of children with osteochondritis dissecans typically recover through conservative measures within 6 to 18 months, whereas adults often necessitate surgical intervention. If the condition is left untreated, affected patients may experience degenerative changes, chronic pain, and mechanical symptoms such as locking and clicking. This topic reviews the pathophysiology, diagnosis, and management of knee osteochondritis dissecans, providing healthcare professionals with crucial insights to enhance overall patient care for individuals grappling with this uncommon yet potentially debilitating cause of knee pain.
Objectives:
Identify the characteristic clinical manifestations of osteochondritis dessecans of the knee.
Implement evidence-based diagnostic and staging protocols, utilizing plain radiographs and MRI for osteochondritis dessecans of the knee.
Apply knowledge of surgical interventions for osteochondritis dissecans, tailoring approaches based on patient age and lesion characteristics.
Collaborate with specialists to optimize patient outcomes through shared decision-making and strategic treatment plans.
Introduction
Osteochondritis dissecans of the knee is a relatively rare condition, categorized as a form of osteonecrosis affecting the subchondral bone. The condition tends to manifest as knee dysfunction and pain, predominantly affecting school-aged children and adolescents. More specifically, in osteochondritis dissecans, a piece of the subchondral bone and articular cartilage detaches from the underlying bone. The ensuing fragment may be either stable, indicating intact overlying articular cartilage, or unstable, which has significant prognostic implications. Osteochondritis dissecans is more prevalent in individuals aged 10 to 20, with a higher incidence in males than females. Juvenile osteochondritis dissecans occurs in patients with open growth plates or physes, whereas adult osteochondritis dissecans applies to skeletally mature patients.
Although osteochondritis dissecans has been recognized for over a century, its exact cause of knee dysfunction and pain remains unclear.[1] Recently, the Research in Osteochondritis Dissecans of the Knee (ROCK) study group summarized the currently recognized pathophysiology of osteochondritis dissecans as an acquired subchondral lesion characterized by osseous resorption, collapse, and sequestrum formation.[1][2][3] König originally proposed the concept in 1887, suggesting an inflammatory etiology as a contributing factor in osteochondritis dissecans development. Despite the lack of evidence of an inflammatory component in histopathology, the term "osteochondritis" has persisted over the years.[4]
Individuals with this condition may either present with knee pain as a primary complaint or incidentally discover the findings during radiographs conducted for unrelated injuries.[1] Clinicians typically rely on plain radiographs to diagnose and identify the condition,[1] with magnetic resonance imaging (MRI) as the primary staging tool. The typical location for these lesions is the distal femur, especially in the lateral aspect of the medial femoral condyle. Initial treatment for stable lesions includes rest, nonsteroidal anti-inflammatory drugs, activity avoidance, and physical therapy. Skeletally immature patients often respond well to nonoperative treatment, whereas skeletally mature individuals with large lesions or the formation of intraarticular loose bodies may require surgical intervention. The most important prognostic factor involves the patient's skeletal age at the time of symptom onset.[5] Although over 50% of children with osteochondritis dissecans typically recover through conservative measures within 6 to 18 months, adults often necessitate surgical intervention.[6] If the condition is left untreated, affected patients may experience degenerative changes, chronic pain, and mechanical symptoms such as locking and clicking.
Etiology
Although the exact etiology of osteochondritis dissecans is unknown, current theories include repetitive micro-trauma, ischemia, and genetic predisposition.[7][8] Patients with extreme obesity and elevated body mass index (BMI) are at increased risk of developing osteochondritis dissecans. While universal agreement does not exist regarding the etiology of osteochondritis dissecans of the knee, repetitive trauma is considered the most commonly accepted cause.[1] Experts believe that the adult form is due to vascular insult.
Epidemiology
Osteochondritis dissecans is more commonly diagnosed in younger patients, with the highest incidence occurring between the ages of 12 and 19. Incidence rates in patients in this age group are 3.3 times higher than in adults aged 20 to 45.[3][5][9][10] The overall prevalence of osteochondritis dissecans is between 9.5 and 29 per 100,000 population. Males have a 2 to 4 times higher incidence of osteochondritis dissecans than females.[2][5][2][11][12] The overall prevalence of osteochondritis dissecans lesions, particularly in the knee, is estimated to be 15 to 29 per 100,000 patients.
Seventy-five percent of patients affected by osteochondritis dissecans have knee lesions, out of which 64% have knee lesions in the medial femoral condyle.[6] Furthermore, 32% of the knee lesions localize to the lateral condyle, while the remaining cases localize to the trochlea, patella, and tibial plateau. Osteochondritis dissecans is typically unilateral, but studies reveal that 7% to 25% of patients have bilateral disease.[9][10]
Pathophysiology
Osteochondritis dissecans typically affects highly active school-aged children and adolescents. Although the condition is commonly associated with repetitive trauma, it can also result from an isolated injury. The underlying pathophysiology begins with a disruption of the epiphyseal vessels, causing ischemia and necrosis at the trauma site. Consequently, softening, tearing, fissuring, and erosion of hyaline cartilage occurs. As the affected area advances, focal demineralization and repeated shear forces lead to detachment of the bone and overlying cartilage.[9] Experts suggest that repetitive axial loading, particularly with increased valgus or varus stress, may contribute to this stage. The lesions of osteochondritis dissecans can introduce irregularities in the articular surface, potentially resulting in degenerative arthritis.
History and Physical
History
Healthcare professionals should maintain a high index of suspicion, as the symptoms of osteochondritis dissecans can mimic other common causes of knee pain. Patients generally present with vague, poorly localized knee pain exacerbated by activity. Patients may experience stiffness and occasional swelling during or after activity as the disease progresses. Locking or catching may indicate advanced disease or a sizable loose body.
Clinicians should inquire about the history of trauma, the recent increase in activity level, previous knee injuries, and the presence of mechanical symptoms in their patients.
About 80% of affected patients report pain while performing weight-bearing activities.[13] In juvenile patients, the pain is often intermittent, associated with activity, and poorly localized around the anterior aspect of the joint. Adults with osteochondritis dissecans are more likely to present with effusion and limited range of motion or mechanical symptoms such as catching or locking.[2] Depending on the chronicity of the lesion, patients may report quadriceps dysfunction and intermittent knee instability.[6]
Physical Examination
Inspection: Examination of knee alignment may reveal genu varus, often associated with a lesion at the medial femoral condyle, or genu valgus, which is more common in cases of osteochondritis dissecans affecting the lateral femoral condyle.[13] Quadriceps atrophy or weakness may be evident, and a foreign body may be palpable.
Palpation: During joint palpation, the knee may be flexed with varying degrees to reveal effusion or bony tenderness along the femoral condyles. The patient's range of motion may be restricted due to pain, swelling, or the presence of a loose body compared to the contralateral knee.
Special tests: The Wilson sign can identify lesions of the lateral aspect of the medial femoral condyle. This test involves simultaneous internal rotation of the tibia and active extension of the knee from 90° to 30°. A positive test is indicated by pain elicited with internal rotation and relieved by external rotation, indicating impingement of the osteochondritis dissecans lesion by the medial tibial eminence.[13]
During the examination, the patient is seated with their knee bent over the examination table. The patient is then asked to actively straighten their knee while the clinician rotates the tibia medially. Patients with osteochondritis dissecans of the lateral aspect of the medial femoral condyle will typically feel greater pain at around 30° of flexion. When the patient experiences pain, the clinician can try rotating the tibia laterally. If this is done correctly, the pain should go away.
Although the presence of the Wilson sign is helpful, its absence does not rule out osteochondritis dissecans as a diagnosis. The Wilson sign is negative on radiographs in 75% of patients with osteochondritis dissecans. Therefore, clinicians should observe the patient's walking pattern, as it may unveil an antalgic gait or the foot of the affected side rotated laterally to alleviate weight-bearing pain.
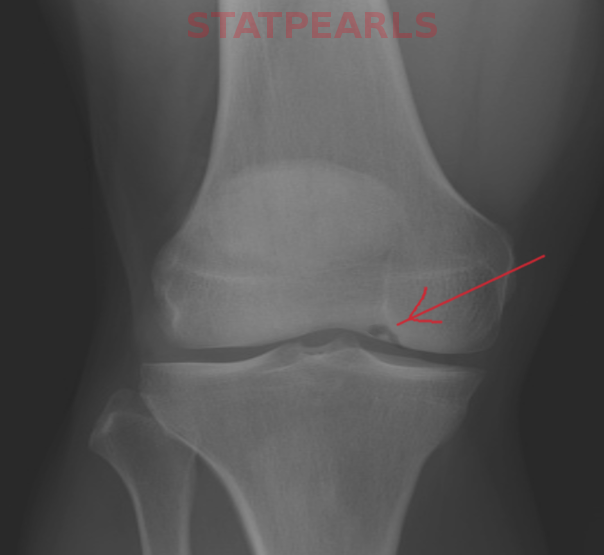
Evaluation
The initial assessment involves plain radiographs to locate the lesion, assess growth plates, and rule out other conditions. Patients should undergo standing anteroposterior, lateral, sunrise, and notch or tunnel views. Initial radiographs appear normal in patients with osteochondritis dissecans. The notch view, an anteroposterior projection with 30° to 50° of knee flexion, offers a more comprehensive evaluation of the posterior femoral condyles.[2] In the literature, common characteristics of lesions include distinct lucent areas of bone with varying density levels. These areas may or may not display calcifications and lucent lines that separate the fragment from the bone, depending on the severity of the lesion. For comparison, clinicians should consider obtaining radiographs of both knees, as up to 25% of patients may reveal bilateral osteochondritis dissecans.
Cahill and Berg proposed a classification based on the lesion's location, dividing the knee into 15 anatomical zones. [2] Although not frequently utilized in clinical practice, lesion localization in this manner provides important prognostic information. Less common, atypical locations such as the trochlea or patella may not respond as effectively to conservative management.[14]
MRI can evaluate unstable osteochondritis dissecans lesions, which may present as mechanical symptoms or knee effusion. Unstable osteochondritis dissecans lesions on MRI might exhibit increased T2 signal at the articulation of the host bone and the lesion or destruction of the overlying articular cartilage. The presence of multiple cyst-like foci or a single focus of more than 5 mm may also indicate instability of the osteochondritis dissecans lesion on MRI.[9][15]
Apart from assessing lesion stability, MRI proves valuable in the diagnostic evaluation of osteochondritis dissecans in cases of persistent pain despite negative radiographs, grading lesions identified on plain radiographs, and in differentiating normal ossification centers of the distal femur from osteochondritis dissecans in children. MRI without contrast is sufficient for providing diagnostic and staging information. Including gadolinium contrast becomes necessary when there are uncertainties about the stability of the lesion. Gadolinium can assist in assessing the adequacy of the blood supply to the bony fragment. Hefti et al developed a classification system based on MRI findings, as detailed in the Staging section later in this topic.[16][17] Small observational studies reveal that MRI has nearly 100% sensitivity and specificity for diagnosing and determining the degree of stability in adult patients with osteochondritis dissecans. These findings align with results from knee arthroscopy. Although the sensitivity is nearly 100% in skeletally immature patients, the specificity drops to 10% to 15%. In almost 70% of skeletally immature patients, the predictions made by MRI did not align with the arthroscopic stability findings.
Several studies have examined the correlation between MRI findings and the prognosis of osteochondritis dissecans lesions. De Smet et al have proposed certain MRI signs on T2-weighted scans that may be associated with unstable lesions, which are mentioned below.
- A line of intense signal equal to that of fluid at the fragment-bone interface measuring ≥5 mm in length.
- A discrete round focus of intense signal located deep to the osteochondritis dissecans lesion measuring ≥5 mm.
- A focal defect in the overlying articular cartilage that measures ≥5 mm in width.
- An intense signal equal to that of fluid that traverses both the articular cartilage and subchondral bone and extends into the lesion.[18][19]
A line of high signal intensity between the fragment and underlying bone is considered the most sensitive prognosticator of instability.[18][19] Unstable lesions are less likely to heal with nonoperative management.
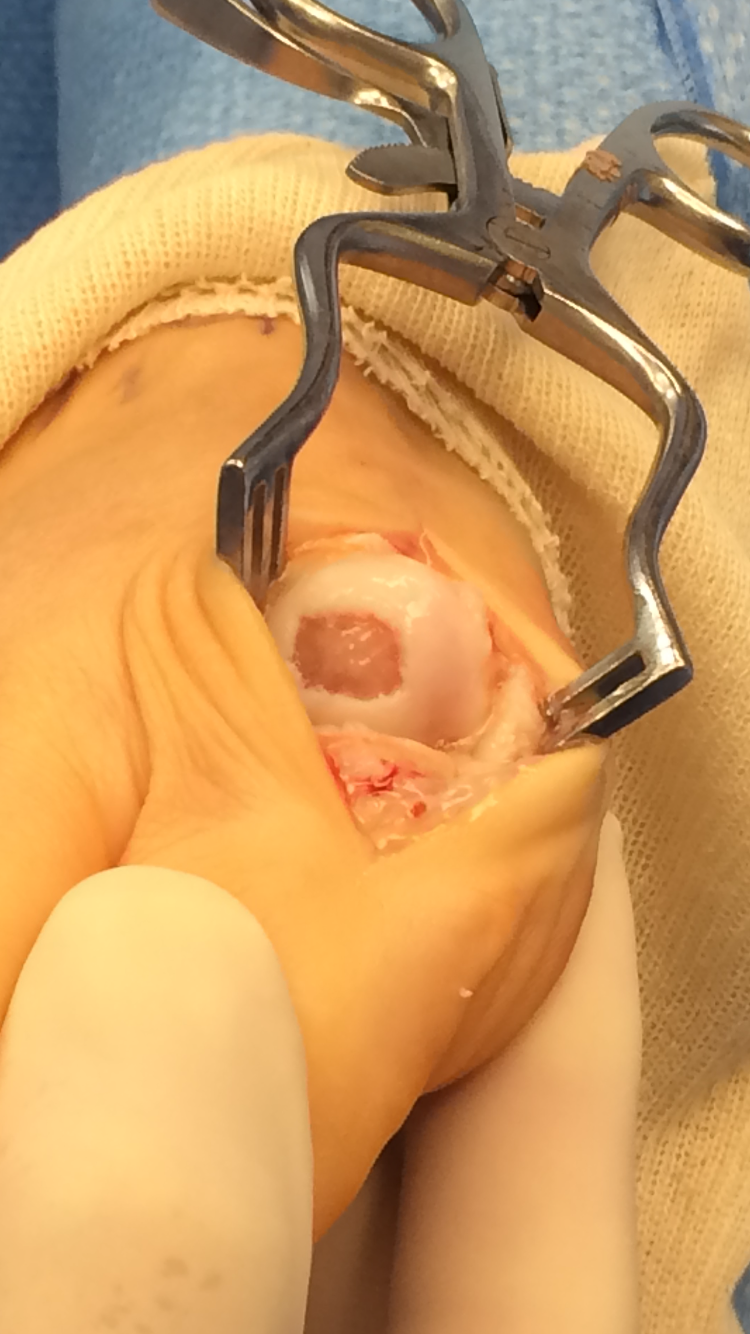
Arthroscopy is the gold standard for assessing lesion stability and determining appropriate management. The International Cartilage Repair Society has developed an intraoperative classification that defines the fragment's integrity and stability, as described in the Staging section later in this topic.[20]
Treatment / Management
Treating osteochondritis dissecans of the knee includes conservative and surgical approaches, with the choice depending on the patient's age as well as the severity and location of the disease.
Nonoperative Treatment
Clinicians consider nonoperative treatment for all juvenile patients without a displaced fragment or stage I to III disease, which includes:
- Cessation of participation in sports.
- Immobilization of the knee with a cast, splint, or hinged brace for 4 to 6 weeks.
- Initiation of physical therapy by the patient after immobilization and when healing is evident radiographically. The patient persists with physical therapy until becoming pain-free, achieving full range of motion, and attaining equal strength, power, and mobility compared to the other knee. Bracing is maintained throughout the recovery period. The patient may gradually resume sports activities once asymptomatic, having completed physical therapy, and experiencing no pain during running, sprinting, or cutting. This entire process typically takes approximately 6 months.[21]
- Utilization of nonsteroidal anti-inflammatory medications by the patient as necessary to manage pain and edema.
Studies estimate that 50% to 75% of affected patients will heal without fragmentation. Nonoperative therapy is also a viable option for adults with stage I or II disease, but the healing rate with nonoperative measures is 50% or less. Treatment is not necessary if osteochondritis dissecans of the knee is incidentally diagnosed in an asymptomatic patient. However, the patient should continue with regularly scheduled appointments until documented radiographic healing occurs.[13]
Operative Treatment
Experts recommend surgery for treating osteochondritis dissecans of the knee if conservative measures are not suitable or prove ineffective after 3 to 6 months. In adults, surgical intervention is the primary treatment for any symptoms related to osteochondritis dissecans, stage II disease, or expanding lesions observed on plain radiographs. Juveniles with stage IV disease or the presence of loose bodies, unstable lesions, or in the presence impending physeal closure warrant surgical intervention.[21][22]
Subchondral drilling: If the osteochondritis dissecans lesion appears stable during arthroscopy, the patient may undergo subchondral drilling using either a transchondral or retrograde approach with k-wire placement, which leads to the formation of fibrocartilage tissue. This approach is a good choice for skeletally immature patients.
Fixation of unstable lesions: If arthroscopy shows an unstable osteochondritis dissecans lesion or MRI shows a lesion larger than 2 cm, the lesion should be repaired by fixation.[23]
Chondral resurfacing is a consideration for lesions larger than 4 cm², which can be accomplished using various techniques. Microfracture surgery stimulates healing to increase fibrocartilage, leading to good short-term results; however, it has decreased durability and increased failure rates.[22] Clinicians perform microfracture using a microfracture awl advanced to a depth of 1 to 1.5 cm below the articular surface. After surgery, patients must avoid bearing weight on the affected limb for a period of 4 to 6 weeks. During recovery, patients should continue with passive range of motion exercises.
Osteochondral allografts: Although osteochondral allografts are a viable option, they are expensive. Clinicians perform allografts via arthrotomy or arthroscopic procedures. Arthrotomy is preferable for lesions larger than 3 cm. Autologous graft procedures lead to native bone-to-bone healing, potentially resulting in a faster recovery. Periosteal patches are implants that have shown promise in regenerating cartilage and are used clinically to aid in the regeneration process.[24] Furthermore, for patients older than 60, arthroplasty is typically the recommended surgical approach.[22]
Differential Diagnosis
The conditions that outline the differential diagnoses for juvenile osteochondritis dissecans include patellofemoral syndrome, patellar tendonitis, Osgood-Schlatter disease, Sinding-Larsen-Johansson syndrome, fat pad impingement, symptomatic discoid meniscus, and symptomatic synovial plica.
In an adult experiencing typical weight-bearing knee pain, potential differential diagnoses include patellofemoral pain, knee osteoarthritis, chondromalacia, patellar tendonitis, meniscal tear, fat pad impingement, and symptomatic synovial plica.
In adults presenting with more severe symptoms such as atraumatic edema and mechanical symptoms, potential differential diagnoses include meniscal tear, osteochondral loose body, and neoplasm.
Staging
Clanton and DeLee Classification of Osteochondritis Dissecans
Clanton and DeLee's classification system for osteochondritis dissecans is based on radiographic findings and includes 4 types, as mentioned below.
Type I: Depressed osteochondral fracture
Type II: Attached fragment with an osseous bridge
Type III: Detached fragment but no displacement
Type IV: Detached and displaced fragment
Hefti Classification of Osteochondritis Dissecans
Hefti's classification system for osteochondritis dissecans is based on MRI findings and includes 5 types, as mentioned below.
Type I: A small change of signal in the subchondral bone without clear margins
Type II: Osteochondral lesion with clear margins, with no underlying fluid between the fragment and bone
Type III: Fluid partially visible between the fragment and underlying bone
Type IV: Fluid surrounds the fragment, but the fragment remains in situ
Type V: Loose body
The International Cartilage Repair Society Classification of Osteochondritis Dissecans
The classification system of the International Cartilage Repair Society (ICRS) is based on the findings obtained through arthroscopy and includes 4 types, as mentioned below.
Type I: Softening of an intact cartilage
Type II: Cartilage breached, but stable fragment when probed
Type III: Fragment discontinuity, unstable when probed, but the fragment is in place
Type IV: Osteochondral crater and loose body
Prognosis
The prognosis of osteochondritis dissecans of the knee is influenced by the patient's age and the location and appearance of the lesion on imaging. Generally, the prognosis for juvenile patients is more favorable than for adults. In particular, pediatric patients with open distal femoral physes have the best prognosis for complete recovery with conservative measures.
If left untreated, adults with the disease often progress to arthritis.[21] Certain factors are associated with a higher incidence of poor outcomes in the case of osteochondritis dissecans. These factors include:
- Lesions located on the lateral femoral condyle or patella
- Higher stages of the disease, as revealed by imaging techniques
- Lesions that show sclerosis on radiography or synovial fluid behind the lesion on MRI [25]
Patient prognosis is significantly influenced by how individuals allow their bodies to heal completely. Those with less severe disease who permit complete recovery can generally regain full knee function. Juvenile patients with Stage I or II disease have a 95% chance of regaining full knee function. Patients with more severe stage III or IV lesions who do not have full recovery often progress to chronic pain, mechanical symptoms, and arthritic disease.[26] Skeletally mature patients with advanced disease have a 50% chance of developing chronic symptoms.
Complications
Potential complications of osteochondritis dissecans are as follows:
- Degenerative articular changes over time
- A nonunion and dissociation of the bony fragment
- Chronic pain and mechanical symptoms
- Surgical complications, including postoperative infection, pneumonia, hemorrhage, and reactions to anesthesia
- Venous thrombosis due to immobility [26]
Consultations
Clinicians should refer to an orthopedic or sports medicine specialist based on the likelihood of lesion healing with nonoperative therapy. Referral is recommended for the following patients:
- Skeletally immature patients with partially or wholly detached knee lesions as seen on plain radiographs or MRI
- Skeletally immature patients with stage 1 lesions larger than 2 cm in length or more than 6% scaled surface area on MRI
- Skeletally immature patients with clinically identifiable mechanical findings like locking or catching
- Skeletally mature patients
- Patients who do not respond to nonoperative treatment
Primary care clinicians can manage osteochondritis dissecans in skeletally immature patients with small, stable lesions when they are familiar and comfortable with the protocol for immobilization, rehabilitation, and proper clinical and imaging criteria to determine healing.
Deterrence and Patient Education
In patients with osteochondritis dissecans, a segment of subchondral bone and articular cartilage separates from the underlying bone, and the fragments of bone may be stable or unstable. Currently, established guidelines do not exist to prevent this condition. Patients, coaches, athletic trainers, and caregivers must understand that ongoing knee pain in a young athlete is not just "growing pains" or something to be "pushed through."
Active juveniles, caregivers, and coaches must understand that patients have a 95% chance of regaining full knee function with conservative management when treated appropriately. In addition, they need to understand that the process involves immobilization, physical therapy, repeat imaging, and restricted activities until fully healed. Juveniles with a loose body or who do not respond to nonoperative treatment require operative intervention. Adults with osteochondritis dissecans of the knee should be aware that although they may be able to treat the lesion with nonoperative therapy, they have a much higher likelihood of needing operative intervention. Osteochondritis dissecans can lead to lifelong pain and mechanical symptoms for both juvenile and adult patients.
Enhancing Healthcare Team Outcomes
Knee osteochondritis can pose a diagnostic challenge, as the lesion may either be asymptomatic or mimic other causes of knee pain. The management of osteochondritis dissecans of the knee in patients necessitates an interprofessional team of healthcare professionals, including primary care, sports medicine, orthopedics, physical therapy, radiology, and pharmacy. All clinicians caring for patients with osteochondritis dissecans must possess the essential knowledge to recognize and differentiate osteochondritis dissecans from other causes of knee pain, including ordering the appropriate diagnostic imaging to diagnose and stage the lesions. Healthcare professionals must collaborate as a cohesive team, providing the proper specialty referrals when necessary.
Each specialist should understand their specific contribution to the team and provide seamless interprofessional communication to foster patient-centered collaborative decision-making. A strategic approach to implementing evidence-based treatments is imperative to provide the best possible care, optimize patient outcomes, and reduce morbidity. Clinicians must ensure that patients and caregivers are fully educated and obtain informed consent before all treatments. By adopting a team-based approach centered on skill, communication, strategy, and ethics, healthcare professionals can reduce morbidity and improve overall patient care and quality of life for patients with osteochondritis dissecans of the knee.