Continuing Education Activity
Chronic inflammation is also referred to as slow, long-term inflammation lasting several months to years. Generally, the extent and effects of chronic inflammation vary with the cause of the injury and the ability of the body to repair and overcome the damage. This activity reviews the pathophysiology of chronic inflammation and highlights the role of the interprofessional team in taking steps to control the pathology.
Objectives:
- Identify the etiology of chronic inflammation.
- Summarize the pathophysiology of chronic inflammation.
- Outline the treatment and management options available for chronic inflammation.
- Explain interprofessional team strategies for improving care coordination and communication to advance the control of chronic inflammation and improve outcomes.
Introduction
Inflammation is part of the body's defense mechanism. It is the process by which the immune system recognizes and removes harmful and foreign stimuli and begins the healing process. Inflammation can be either acute or chronic.[1][2][3]
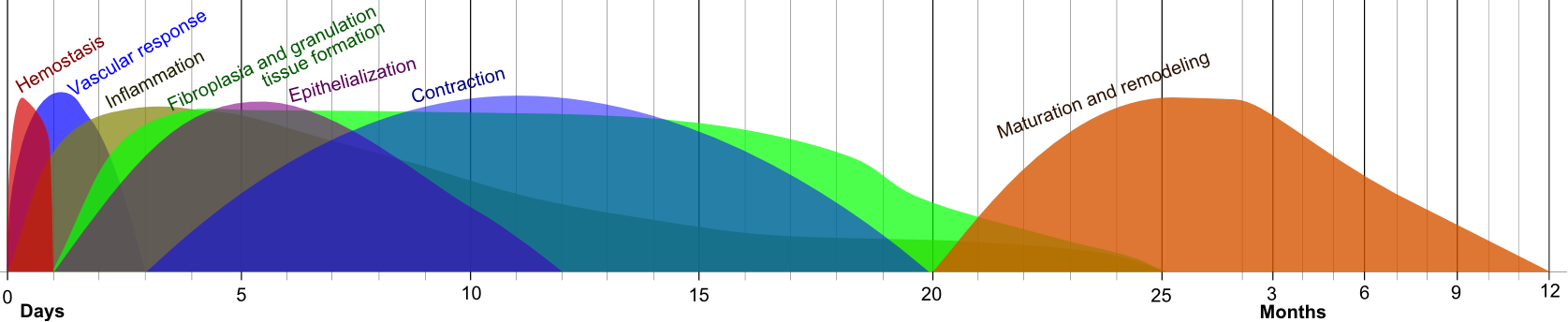
Acute Inflammation
Tissue damage due to trauma, microbial invasion, or noxious compounds can induce acute inflammation. It starts rapidly, becomes severe in a short time and symptoms may last for a few days for example cellulitis or acute pneumonia. Subacute inflammation is the period between acute and chronic inflammation and may last 2 to 6 weeks.
Chronic Inflammation
Chronic inflammation is also referred to as slow, long-term inflammation lasting for prolonged periods of several months to years. Generally, the extent and effects of chronic inflammation vary with the cause of the injury and the ability of the body to repair and overcome the damage. This article reviews chronic inflammation.
Etiology
Chronic inflammation can result from the following:
- Failure of eliminating the agent causing an acute inflammation such as infectious organisms including Mycobacterium tuberculosis, protozoa, fungi, and other parasites that can resist host defenses and remain in the tissue for an extended period.
- Exposure to a low level of a particular irritant or foreign material that cannot be eliminated by enzymatic breakdown or phagocytosis in the body including substances or industrial chemicals that can be inhaled over a long period, for example, silica dust.
- An autoimmune disorder in which the immune system recognizes the normal component of the body as a foreign antigen, and attacks healthy tissue giving rise to diseases such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE).
- A defect in the cells responsible for mediating inflammation leading to persistent or recurrent inflammation, such as auto-inflammatory disorders (Familial Mediterranean Fever).
- Recurrent episodes of acute inflammation. However, in some cases, chronic inflammation is an independent response and not a sequel to acute inflammation for example diseases such as tuberculosis and rheumatoid arthritis.
- Inflammatory and biochemical inducers are causing oxidative stress and mitochondrial dysfunction such as increased production of free radical molecules, advanced glycation end products (AGEs), uric acid (urate) crystals, oxidized lipoproteins, homocysteine, and others.
Epidemiology
Chronic inflammatory diseases are the most significant cause of death in the world. The World Health Organization (WHO) ranks chronic diseases as the greatest threat to human health. The prevalence of diseases associated with chronic inflammation is anticipated to increase persistently for the next 30 years in the United States. in 2000, nearly 125 million Americans were living with chronic conditions and 61 million (21%) had more than one. In recent estimates by Rand Corporation, in 2014 nearly 60% of Americans had at least one chronic condition, 42% had more than one and 12% of adults had 5 or more chronic conditions. Worldwide, 3 of 5 people die due to chronic inflammatory diseases like stroke, chronic respiratory diseases, heart disorders, cancer, obesity, and diabetes. [4][5][6]The prevalence of some specific chronic inflammation-mediated diseases are as follows:
- Diabetes: According to the American Diabetes Association, 30.3 million people or 9.4% of the American population, had diabetes in 2015 and it was the 7th leading cause of death in the United States.
- Cardiovascular diseases: In line with 2017 updated report from the American Heart Association, cardiovascular diseases (CVDs) accounts for 1 out of every three deaths or approximately 800,000 deaths in the United States. Globally, CVD accounts for 31% of all deaths, and coronary heart disease (CHD) accounts for most deaths due to CVD, followed by stroke (1 of 20 deaths in the United States) and heart failure.
- Arthritis and Joint Diseases: These affect approximately 350 million people worldwide and nearly 43 million people in the United States or almost 20% of the population. This number is expected to exceed 60 million by 2020. Nearly, 2.1 million Americans suffer from rheumatoid arthritis.
- Allergies: These rank among the sixth leading cause of chronic human diseases in the United States and affect more than 50 million Americans each year. Asthma affects more than 24 million people in the United States including more than 6 million children. In 2015, 8.2% of adults and 8.4% of children were diagnosed with hay fever.
- Chronic Obstructive Pulmonary Disease (COPD): The third most common cause of death in the United States in 2014, and nearly 15.7 million Americans (6.4%) were reported to have been diagnosed with COPD.
Pathophysiology
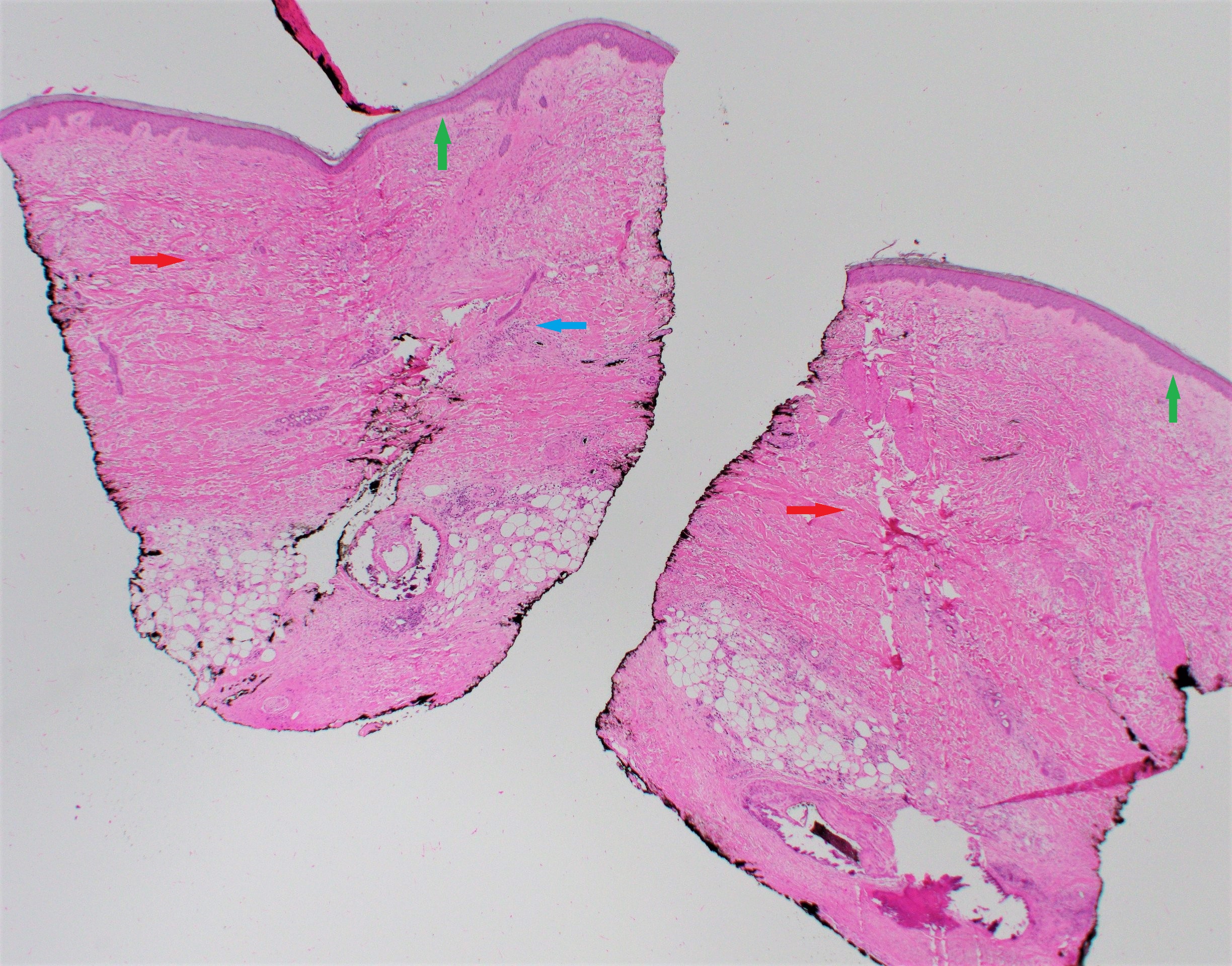
Most of the features of acute inflammation continue as the inflammation becomes chronic, including the expansion of blood vessels (vasodilation), increase in blood flow, capillary permeability and migration of neutrophils into the infected tissue through the capillary wall (diapedesis). However, the composition of the white blood cells changes soon and the macrophages and lymphocytes begin to replace short-lived neutrophils. Thus the hallmarks of chronic inflammation are the infiltration of the primary inflammatory cells such as macrophages, lymphocytes, and plasma cells in the tissue site, producing inflammatory cytokines, growth factors, enzymes and hence contributing to the progression of tissue damage and secondary repair including fibrosis and granuloma formation, etc.[7][8][9][10]
In response to foreign or self-antigens, the tissue immune cells such as macrophages and dendritic cells release cytokines such as IL-1 and TNF-α. These cytokines induce the injury-site-endothelial cells to release Selectins and Integrins which stimulate chemotaxis and diapedesis of the circulating leukocytes. In addition to the recruitment of leukocytes, the tissue macrophages, and dendritic cells also play a role in the clearing of the antigen by phagocytosis, the release of cytokines and serving as antigen-presenting-cells to lymphocytes. Once the circulating leukocytes enter the local injury site, they are activated by various cytokines and chemokines secreted by the macrophages and dendritic cells. On activation, the leukocytes further release cytokines and mediators of inflammation. Neutrophils are the initial cells and most predominant in the acute phase of inflammation. Neutrophils contain granules rich with lysozyme, matrix metalloproteinases, myeloperoxidase which are released on the foreign or self-antigen leading to its destruction. Neutrophils also destroy the antigen by phagocytosis, the release of reactive oxygen species and cytokines such as IL-1, IL-6, and TNF-α. Lymphocytes including T-lymphocytes and B-lymphocytes are the next line of defense, and they play a crucial role in mediating inflammation by several complex mechanisms including secreting of cytokines, costimulation of lymphocytes, and production of antibodies and immune complexes. Circulating platelets can also play a role in inflammation by platelet aggregation, thrombus formation and degranulation releasing chemokines and inflammatory mediators.
Types of Chronic Inflammation
- Nonspecific proliferative: Characterized by the presence of non-specific granulation tissue formed by infiltration of mononuclear cells (lymphocytes, macrophages, plasma cells) and proliferation of fibroblasts, connective tissue, vessels, and epithelial cells, for example, an inflammatory polyp-like nasal or cervical polyp and lung abscess.
- Granulomatous inflammation: A specific type of chronic inflammation characterized by the presence of distinct nodular lesions or granulomas formed with an aggregation of activated macrophages or its derived cell called epithelioid cells usually surrounded by lymphocytes. The macrophages or epithelioid cells inside the granulomas often coalesce to form Langhans or giant cells such as foreign body, Aschoff, Reed-Sternberg, and Tumor giant cells. There are two types:
- Granuloma formed due to foreign body or T-cell mediated immune response is termed as foreign body granuloma, for example, silicosis.
- Granuloma formed due to chronic infection is termed as infectious granuloma, for example, tuberculosis and leprosy.
History and Physical
Risk Factors Associated with Chronic Inflammation
Several risk factors promote a low-level inflammatory response. These include:
- Age: Increasing age is positively correlated with elevated levels of several inflammatory molecules. The age-associated increase in inflammatory molecules may be due to mitochondrial dysfunction or free radical accumulation over time and other age-related factors like an increase in visceral body fat.
- Obesity: Many studies have reported that fat tissue is an endocrine organ, secreting multiple adipokines and other inflammatory mediators. Some reports show that the body mass index of an individual is proportional to the amount of pro-inflammatory cytokines secreted. Metabolic syndrome typifies this well.
- Diet: Diet rich in saturated fat, trans-fats, or refined sugar is associated with higher production of pro-inflammatory molecules, especially in individuals with diabetes or overweight individuals.
- Smoking: Cigarette smoking is associated with lowering the production of anti-inflammatory molecules and inducing inflammation.
- Low Sex Hormones: Studies show that sex hormones like testosterone and estrogen can suppress the production and secretion of several pro-inflammatory markers and it has been observed that maintaining sex hormone levels reduces the risk of several inflammatory diseases.
- Stress and Sleep Disorders: Both physical and emotional stress is associated with inflammatory cytokine release. Stress can also cause sleep disorders. Since individuals with irregular sleep schedules are more likely to have chronic inflammation than consistent sleepers, sleep disorders are also considered as one of the independent risk factors for chronic inflammation.
Symptoms of Chronic Inflammation
Some of the common signs and symptoms that develop during chronic inflammation are listed below.
- Body pain, arthralgia, myalgia
- Chronic fatigue and insomnia
- Depression, anxiety and mood disorders
- Gastrointestinal complications like constipation, diarrhea, and acid reflux
- Weight gain or weight loss
- Frequent infections
Evaluation
Tests for Chronic Inflammation
Unfortunately, there are no highly effective laboratory measures to assess patients for chronic inflammation and diagnoses are only undertaken when the inflammation occurs in association with another medical condition.
- Serum protein electrophoresis (SPE) can show concomitant hypoalbuminemia and polyclonal increase in all gamma globulins (polyclonal gammopathy).
- The two blood tests that are inexpensive and good markers of systemic inflammation include high-sensitivity C-reactive protein (hsCRP) and fibrinogen. High levels of hs-CRP indicate inflammation, but it is not a specific marker for chronic inflammation since it is also elevated in acute inflammation resulting from a recent injury or sickness. The normal serum levels for hsCRP is less than 0.55 mg/L in men and less than 1.0 mg/L in women. The normal levels of fibrinogen are 200 to 300 mg/dl. SAA (Serum Amyloid A) can also mark inflammation but is not a standardized test.
- Detecting pro-inflammatory cytokines like tumor necrosis factor-alpha (TNF-alpha), interleukin-1 beta (IL-1beta), interleukin-6 (IL-6), and interleukin-8 (IL-8) is an expensive method but may identify specific factors causing chronic inflammation. Again, the assays are not standardized like hs-CRP, fibrinogen, and SPE.
Treatment / Management
Many dietary and lifestyle changes may be helpful in removing inflammation triggers and reducing chronic inflammation as listed below. The most effective is weight loss. For example, in patients with psoriatic arthritis which is chronic inflammatory arthritis, weight loss alone has been shown to be independently associated with clinically significant improvement in disease activity and inflammation.
- Low-glycemic diet: Diet with a high glycemic index is related to high risk of stroke, coronary heart disease, and type 2 diabetes mellitus. It is beneficial to limit the consumption of inflammation-promoting foods like sodas, refined carbohydrates, fructose corn syrup in a diet.
- Reduce intake of total, saturated fat and trans fats: Some dietary saturated and synthetic trans-fats aggravate inflammation, while omega-3 polyunsaturated fats appear to be anti-inflammatory. Processed and packaged foods that contain trans fats such as processed seed and vegetable oils, baked goods (like soybean and corn oil) should be reduced from the diet.
- Fruits and vegetables: Blueberries, apples, Brussels sprouts, cabbage, broccoli, and cauliflower, that are high in natural antioxidants and polyphenols and other anti-inflammatory compounds, may protect against inflammation. Cherries and cherry juice consumption has been shown to be uricosuric and inhibitory for IL-1 in patients with gout.
- Fiber: High intake of dietary soluble and insoluble fiber is associated with lowering levels of IL-6 and TNF-alpha.
- Nuts: such as almonds are associated with lowering the risk of cardiovascular disease and diabetes.
- Green and black tea polyphenols: Tea polyphenols are associated with a reduction in CRP in human clinical studies.
- Curcumin: a constituent of turmeric has been shown to be associated with significant improvement in several inflammatory diseases in animal models.
- Fish Oil: The richest source of the omega-3 fatty acids. Higher intake of omega-3 fatty acids is associated with lowering levels of TNF-alpha, CRP, and IL-6.
- Mung bean: Rich in flavonoids (particularly vitexin and isovitexin). It is a traditional food and herbal medicine known for its anti-inflammatory effects.
- Micronutrients: Magnesium, vitamin D, vitamin E, zinc and selenium). Magnesium is listed as one of the most anti-inflammatory dietary factors, and its intake is associated with the lowering of hsCRP, IL-6, and TNF-alpha activity. Vitamin D exerts its anti-inflammatory activity by suppressing inflammatory mediators such as prostaglandins and nuclear factor kappa-light-chain-enhancer of activated B cells. Vitamin E, zinc, and selenium act as antioxidants in the body.
- Sesame Lignans: Sesame oil consumption reduces the synthesis of prostaglandin, leukotrienes, and thromboxanes and is known for its potential hypotensive activity.
Physical Exercise
In human clinical trials, it is shown that energy expenditure through exercise lowers multiple pro-inflammatory molecules and cytokines independently of weight loss.
Conventional Drugs that Combat Chronic Inflammation
Metformin is commonly used in the treatment of type II diabetic patients with dyslipidemia and low-grade inflammation. The anti-inflammatory activity of metformin is evident by reductions in circulating TNF-alpha, IL-1beta, CRP, and fibrinogen in these patients.
Statins are anti-inflammatory as they reduce multiple circulating and cellular biomediators of inflammation. This pleiotropic effect appears to contribute in part to the reduction in cardiovascular events.
Non-steroidal anti-inflammatory drugs (NSAIDs) like naproxen, ibuprofen, and aspirin acts by inhibiting an enzyme cyclooxygenase (COX) that contributes to inflammation and are mostly used to alleviate the pain caused by inflammation in patients with arthritis.
Corticosteroids also prevent several mechanisms involved in inflammation. Glucocorticoids are prescribed for several inflammatory conditions including inflammatory arthritis, systemic lupus, sarcoidosis, and asthma.
Herbal supplements like ginger, turmeric, cannabis, hyssop, and Harpagophytum procumbens are shown to have anti-inflammatory properties however one should always consult with a doctor before their use and caution should be taken for using some herbs like hyssop and cannabis.
Differential Diagnosis
It is important to realize that chronic inflammation is not a specific disease but a mechanistic process. The diseases associated with chronic inflammation are multiple and include CVD, diabetes, malignancy, auto-immune disease, chronic hepatic and renal disease, etc. A good history, physical examination, and routine laboratory tests (glucose, creatinine, liver function, serum protein electrophoresis, rheumatoid factor, complete blood count, antinuclear antibodies) can confirm or rule out most of the differential diagnoses. Pertinent diagnostic and imaging studies can be helpful in certain circumstances, e.g., colonoscopy in suspected inflammatory bowel disease.
Prognosis
Untreated chronic inflammation generally carries a poor prognosis. Disease-specific morbidity and mortality are dependent on the causative mechanistic process leading to chronic inflammation.
Complications
Although chronic inflammation progresses silently, it is the cause of most chronic diseases and presents a major threat to the health and longevity of individuals. Inflammation is considered a major contributor to several diseases.
- Cardiovascular diseases: Many clinical studies have shown strong and consistent relationships between markers of inflammation such as hsCRP and cardiovascular disease prediction. Furthermore, Atherosclerosis is a pro-inflammatory state with all the features of chronic low-grade inflammation and leads to increase cardiovascular events such as myocardial infarction, stroke, among others.
- Cancer: Chronic low-level inflammation also appears to participate in many types of cancer such as kidney, prostate, ovarian, hepatocellular, pancreatic, colorectal, lung, and mesothelioma.
- Diabetes: Immune cells like macrophages infiltrate pancreatic tissues releasing pro-inflammatory molecules in diabetic individuals. Both circulating and cellular biomarkers underscore that diabetes is a chronic inflammatory disease. Chronic complications linked to diabetes include both microvascular and macrovascular complications. Diabetes not only increases the risk of macrovascular complications like strokes and heart attacks but also microvascular complications like diabetic retinopathy, neuropathy, and nephropathy.
- Rheumatoid arthritis: In a genetically susceptible host, chronic inflammation induced by several environmental factors such as smoking and infections lead to a systemic autoimmune response that causes a local inflammatory response in joints, infiltration of immune cells and release of cytokines. Persistence of chronic inflammation in the synovium in inadequately treated RA has been associated with worse prognosis and radiographic progression of the disease.
- Allergic asthma: A complex, chronic inflammatory disorder associated with inappropriate immune response and inflammation in conducting airways involving a decline in airway function and tissue remodeling.
- Chronic obstructive pulmonary disease (COPD): An obstructive lung disease, develops as a chronic inflammatory response to inspired irritants and characterized by long-term breathing problems.
- Alzheimer's disease: In older adults, chronic low-level inflammation is linked to cognitive decline and dementia.
- Chronic kidney disease (CKD): Low-grade inflammation is a common feature of chronic kidney disease. It can lead to the retention of several pro-inflammatory molecules in the blood and contributes to the progression of CKD and mortality. Amyloidosis can be a result of underlying chronic inflammation that can lead to severe renal complications.
- Inflammatory Bowel Disease (IBD) is a group of chronic inflammatory disorders of the digestive tract. It can develop as ulcerative colitis causing long-lasting inflammation and ulcers in the lining of large intestine and rectum or Crohn's disease characterized by inflammation of the lining of digestive tract dispersing into affected tissues such as mouth, esophagus, stomach and the anus.
Deterrence and Patient Education
Chronic inflammation can have a deleterious effect on the body and is a key factor causing almost all chronic degenerative diseases. The following are some of the most effective ways to prevent chronic inflammation.
- Increase uptake of anti-inflammatory foods: It is important to avoid eating simple sugars, refined carbohydrates, high-glycemic foods, trans fats, and hydrogenated oils. Consuming whole grains, natural foods, plenty of vegetables and fruits such as avocados, cherries, kale, and fatty fish like salmon is helpful in defeating inflammation.
- Minimize intake of antibiotics and NSAIDs: Use of antibiotics, antacids, and NSAIDs should be avoided as it could harm the microbiome in the gut causing inflammation in intestinal walls known as leaky gut which in turn releases toxins and triggers chronic, body-wide inflammation.
- Exercise regularly to maintain an optimum weight: It is largely known that adipose tissue in obese or overweight individuals induces low-grade systemic inflammation. Regular exercise is helpful not only in controlling weight but also decreasing the risk of cardiovascular diseases and strengthening the heart, muscles, and bones.
- Sleep longer: Overnight sleep (ideally at least 7 to 8 hours) helps stimulating human growth hormones and testosterone in the body to rebuild itself.
- Stress Less: Chronic psychological stress is linked to greater risk for depression, heart disease and body losing its ability to regulate the inflammatory response and normal defense. Yoga and meditation are helpful in alleviating stress-induced inflammation and its harmful effects on the body.
Enhancing Healthcare Team Outcomes
There are several chronic inflammatory disorders with no cure. Most are managed with symptomatic therapy. An interprofessional team including primary care physicians, nurses, physical therapists, dieticians, and specialists should be involved in the management of the underlying etiology, as well as prevention of complications of chronic inflammation. Patient education is the key with emphasis on diet and lifestyle modification including weight loss, regular exercises, smoking cessation, healthy diet, and good sleep hygiene. Unfortunately in some cases, life long anti-inflammatory medications may be needed to control chronic inflammation.