Continuing Education Activity
Field intubation is the placement of an advanced airway or endotracheal tube (ET) by emergency medical services (EMS) personnel outside the hospital setting. Endotracheal tube intubation (ETI) has long been the standard for airway control in the prehospital setting and is the focus of this activity. While ET placement has a long history of use in the prehospital setting, its use is not without controversy. When compared to in-hospital intubation, higher failure and complication rates have brought the practice of field intubation into question. Nevertheless, there are times when airway control is paramount, and the ability to intubate a patient who has no airway control is a critical skill for prehospital providers. This procedure requires sufficient knowledge of the proper technique and indications for its use. Local protocols and medical direction should guide prehospital providers regarding their use. This activity outlines field intubation procedures in the prehospital setting and highlights the role of the prehospital provider in performing field intubations on patients who require definitive airway control in the prehospital setting.
Objectives:
- Review the anatomy relevant for performing endotracheal tube intubation.
- Summarize how field intubations impact patient outcomes.
- Review the limitations of performing endotracheal tube intubations in the prehospital setting.
- Explain the importance of collaboration and communication amongst the interprofessional team to ensure appropriate training, enhance the delivery of care, and improve outcomes for patients undergoing endotracheal tube intubation in the prehospital setting.
Introduction
Field intubation is the placement of an advanced airway or endotracheal tube (ET) by emergency medical services (EMS) personnel outside the hospital setting. There are many techniques available to control a patient’s airway or provide rescue ventilation and oxygenation to a patient. ET intubation (ETI), nasotracheal intubation, supraglottic airway devices, continuous positive airway pressure (CPAP), and bilevel positive airway pressure (BPAP) machines are all viable options in the right clinical situations. ETI has long been the standard for airway control in the prehospital setting and is the focus of this article.[1] While ET placement has a long history of use in the prehospital setting, its use is not without controversy.[2] When compared to in-hospital intubation, higher failure and complication rates have brought the practice of field intubation into question.[3] Nevertheless, there are times when airway control will be paramount, and the ability to intubate a patient who has no airway control is a critical skill needed for prehospital providers in the field. This procedure requires a clear understanding of the proper technique and indications for its use. Local protocols and medical direction should guide prehospital providers regarding their use.
The decision to intubate a patient should carefully be planned. The procedure can be technically challenging and lead to additional problems even in the best of circumstances. Provider competency and comfort with the procedure may also dictate whether a patient should be intubated. If a provider is unfamiliar or uncomfortable with performing field intubation, alternatives should be used if possible. Supraglottic airways and alternatives to intubation, such as continuing to provide ventilatory support via a bag-valve-mask (BVM) with airway adjuncts or CPAP and BPAP machines, might be better and safer alternatives in certain situations. The use of supraglottic airways, airway adjuncts, and CPAP/BPAP are discussed in separate articles and are not addressed here. There will be minor variances in technique and equipment used in-field intubation depending on provider competency and local protocols, but the main concepts should apply across all EMS jurisdictions. Field intubation should be used in patients that have lost control or have an impending loss of their airway, or patients that require increased ventilatory support that cannot be maintained through BVM ventilation and the use of airway adjuncts. Training and practice, appropriate patient evaluation and selection, and preparation in advance of difficult airway situations are all critical to the success of field intubation.
Despite a long history of prehospital airway management, there is conflicting evidence to show morbidity or mortality benefit when using prehospital intubation.[3] Much of the published research has focused on the success rates and complication rates of the procedure. While it is crucial to continue to track prehospital personnel performing field intubation, future studies should also strive to identify emerging techniques, technology, and training methods to improve outcomes.
Anatomy and Physiology
The relevant anatomy for field intubation is the oropharynx, larynx, esophagus, and upper airway. Providers need to be able to identify key landmarks when attempting field intubation to ensure good outcomes. For direct laryngoscopy, the provider should be able to locate at the very minimum the structures of the oropharynx, epiglottis, arytenoids, and vocal cords to ensure direct visualization of the ET tube entering the trachea. Variances in patient anatomy such as the location of the epiglottis and vocal cords relative to an anterior and posterior position in the oropharynx, or the size of the airway for patients of different body types and ages, can lead to difficulties when intubating a patient. Several mnemonics, acronyms, and scoring systems are available to help identify potentially difficult airway characteristics. A commonly used acronym to help predict a difficult airway is LEMON. LEMON stands for:
- L: Look externally
- E: Evaluate the 3-3-2 rule
- M: Mallampati score
- O: Obstruction
- N: Neck Mobility
When looking externally, a provider should look for any signs that this may be a difficult airway. Physical characteristics including short or thick necks, obesity, dental conditions such as underbites and overbites, missing teeth, or facial trauma that may make the airway unstable, can all increase the difficulty of the procedure. Three anatomical measurements make up the 3-3-2 rule. Ideally, a patient should be able to open their mouth three finger widths, there should be three finger widths from the chin to the hyoid bone along the mandible, and there should be two finger widths from the hyoid bone to the thyroid notch. Variation in these measurements can indicate a patient with difficult anatomy for intubation. The Mallampati score is an assessment of the oropharyngeal structures that can also identify difficult airways. A patient is scored I to IV on the Mallampati scale based on the oropharyngeal structures seen with the patient's mouth open. A score of I indicates the ideal airway with the entire posterior pharynx fully exposed. A score of II indicates only partial visualization of the posterior pharynx. A score of III indicates that the posterior pharynx cannot be seen, but the base of the uvula is still visible. A score of IV indicates the most difficult airway when no posterior structures are visible. Airway obstruction may be anything that could interfere with the direct visualization of the ET tube into the trachea, such as trauma, edema, or masses in the mouth or neck. Neck mobility may be limited by cervical collars, trauma, or preexisting comorbidities and will decrease the provider’s ability to align the airway for maximum success.
In a study by Gaither et al., difficult airway predictors were identified in a retrospective of patients that required intubation in the ED after failed prehospital attempts or non-attempts before arrival in the ED.[4] The study found that airway edema is associated with the highest likelihood of failure or non-attempts in the field. Airway edema was followed by blood, facial trauma, large tongue, short neck, c-spine immobility, vomit, obesity, and a short mandible in decreasing order of difficulty. It was also found that there is an additive effect to these difficult airway predictors and the likelihood of intubation failure increased significantly when more than one predictor was present. As above, the authors advocated an acronym to help identify potentially difficult airway features. The authors used BE FAST (Blood, Emesis, Facial trauma, Airway edema, Spinal immobilization or short neck, and large Tongue) to identify the most common difficult airway predictors, all of which can also be identified with the use of LEMON above. Which acronym, mnemonic, or scoring system used is less important than ensuring that the method used can quickly and easily identify potential pitfalls before the procedure.
Indications
Patients require an advanced airway under two sets of circumstances: failure to maintain a patent airway and the inability to oxygenate and ventilate the patient adequately.[5] The etiologies of these circumstances can vary and include but are not limited to:
- A diminished level of consciousness with concern for the loss of airway control (Glasgow coma scale less than 8)
- Hypoxemic or hypercarbic respiratory failure
- Cardiac arrest
- Risk of aspiration with vomiting, secretions, or blood
- Airway obstruction
Each provider's local protocols will identify definitive indications for field intubation and can guide a provider to the appropriate action. The online medical command can also provide real-time guidance to providers in the field to help improve outcomes.
Contraindications
There are generally accepted contraindications to performing field intubation. Absolute contraindications are hard to define, but if the procedure cannot be completed in a manner that is reasonably safe for both the provider and the patient, field intubation should not be attempted.[2] The situations where absolute contraindications occur include but are not limited to an unstable or dangerous environment, or when there is no provider qualified to perform endotracheal intubation, or when the appropriate equipment is unavailable.[2] Relative contraindications are situation-specific. These include patient circumstances that may place the procedure outside the provider's technical skill, such as severe trauma or a pathological condition that prevents opening the mouth, epiglottitis, copious secretions, vomit, or blood, all of which may impair direct visualization of the airway.[2] Additionally, there may be contraindications for the use of specific rapid sequence intubation (RSI), or sedation assisted intubation (SAI), pharmacologic agents, based on patient comorbidities and condition.
Field intubation should also never be used in a punitive manner. Patients that are intoxicated or uncooperative and have no other medical need for urgent airway control should not be intubated.[2] At times, sedation or paralyzation of the patient is needed to ensure patients' or providers' safety, but these occurrences should be sporadic at best.[2] “Social intubations” should not be considered.
The time required for arrival to care can be another relative contraindication to field intubation.[2] Often, especially in an urban environment, the patient may be safely transported with a BVM supporting respirations or stabilized temporarily with adjuncts such as CPAP when arrival time to a receiving facility is short.[3] The time taken to prepare for and perform the procedure could be better used to deliver the patient to definitive care where there is more support available and a more controlled environment. Providers in rural areas or air medical personnel may elect to be more aggressive with airway control, as there may be a higher incidence of patient decompensation or increased difficulty performing the procedure en route.
Equipment
When performing field intubation, a provider should use the equipment with which he or she is most comfortable. This choice is often both provider and company-specific. At a minimum, the provider will require:
- An appropriate size laryngoscope blade MAC, Miller, or combination blade, with a functioning light source
- An appropriate size ET based on patient anatomy and age
- An appropriate size stylet for ET tube used.
- Ten-mL syringe to inflate the balloon after insertion
- Medications to provide sedation in SAI or sedation and paralytic medications used in RSI as allowed by local protocols.
- Intravenous (IV) access if SAI or RSI is to be utilized or to provide resuscitation medications.
- Age-appropriate BVM with a reservoir and needed attachments to ventilate the patient before and after the procedure
- Suction equipment to clear vomitus, secretions, among others
- Rescue equipment such as a gum elastic bougie, multiple sized tubes to account for stenosis or anatomical differences in patients, supraglottic airway devices, or video laryngoscopy equipment, if available.
- Equipment for surgical airway as allowed by local protocols in the event of a catastrophic airway failure
- Methods for tube placement confirmation such as end-tidal carbon dioxide (CO2) monitoring equipment, waveform capnography, or color change CO2 detectors
- Tape or commercially available "tube holders" to maintain an appropriate ET position.
- Gloves, mask, and goggles as personal protective equipment
Personnel
All personnel involved in field intubation must be adequately trained and be proficient with the procedure. Field intubation should not be undertaken alone if possible since it is nearly impossible to prepare for and safely perform the intubation and other ancillary resuscitative tasks simultaneously without help. Additional personnel can assist with BVM respirations, equipment set-up and control, patient positioning, and external laryngeal positioning. Having multiple staff available capable of performing the procedure can also increase the overall success rate by allowing another provider to attempt the procedure if the first provider fails.
Preparation
Providers should place and position the patient in as controlled an environment as possible.[2] In ideal circumstances, the patient should be supine, with the head in a sniffing position as long as it is not contraindicated by trauma or a patient's preexisting conditions. Pads may be placed under the back to align the patient and airway better. These maneuvers can help align the three planes of the airway, the oral plane, the pharyngeal plane, and the tracheal plane, allowing for direct visualization of the airway. The patient should be placed at a height that allows the provider with the best possible view of the patient's airway. These conditions are commonly not available in the field and adverse environments. There are anecdotal reports of patients being intubated in a seated or recombinant position in cases of entrapment, but there is little evidence to support these measures, and they may pose a risk to both provider and patient (NAEMSP). The best possible preparation is to anticipate a difficult airway every time and have the necessary equipment available, as outlined above. It is best to attempt all intubations in a stable environment without unnecessary hazards to patients and providers. All essential equipment should be available, including all rescue adjuncts, before beginning the procedure to avoid delays when needing rescue treatment for a failed airway.
Technique or Treatment
Intubation technique may vary slightly depending on the operator and equipment used, but the following overarching principles should apply to all situations. The “P’s” of airway control and intubation have long been taught to help providers effectively and safely perform the procedure.[2]
- Plan—providers should plan for the procedure and evaluate the environment to ensure the safety of patients and providers.
- Preparation – the patient should be positioned as described above; all drugs, personal protective equipment, and instruments must be available. All providers should understand and agree to the plan to intubate the patient and how to best care for the patient post-intubation. A Broselow Tape is beneficial when treating pediatric patients to ensure appropriately sized equipment and medication doses.
- Protect – the cervical spine should be protected in the setting of trauma with an additional provider holding in-line stabilization.
- Preoxygenation—patients are typically provided high flow oxygen via a non-rebreather mask or ventilatory support with a BVM and supplemental oxygenation to prevent potential decompensation during laryngoscopy. These measures replace nitrogen in the airways with oxygen to create a reservoir for oxygen exchange during the procedure (Dunford). Apneic oxygenation via high flow nasal cannula may also help maintain oxygen reserves during the peri-intubation period.
- Pretreatment—local protocols may call for the use of pretreatment medications to attenuate the physiologic response patients experience from intubation, such as lidocaine, to blunt the intracranial pressure response to laryngoscopy or atropine to offset bradycardia in pediatric patients. Studies have shown mostly equivocal findings in the OR for premedication but no definitive evidence that it is beneficial in the prehospital setting.[2]
- Local protocols set paralysis and Induction-indications and procedures to induce, sedate, or paralyze the patient and choice of medications available through the medical direction. In general, agents with rapid onset and short durations are best to mitigate problems arising from a failed airway.
- Placement with proof – Appropriate equipment and technique are utilized to place an endotracheal tube through the cords with direct visualization. ETCO2, chest rise, and auscultation should all be used to confirm placement.
- Postintubation management—Patients should be appropriately sedated after intubation to ensure comfort and safety per local protocols. Care must be made to avoid hypoxia, hypoventilation, and hyperventilation, all of which can be detrimental to long-term outcomes and mortality.[6][7][8] ETCO2 monitoring with waveform capnography is the gold standard to ensure appropriate ventilation and continued evaluation of tube placement.[6][7]
Following this approach can mitigate potential problems and ensure a provider can respond to challenging situations if necessary. Proper preparation can also increase the likelihood of first-pass success. First-pass success is critical to help prevent many of the complications described below. Multiple attempts have been associated with an increased risk of intubation failure and complications.[9] When using direct visualization technique or video laryngoscopy, there is no substitute for seeing the tube pass through the vocal cords to ensure proper placement. A provider must be well versed in the relevant anatomy of the larynx and posterior pharynx to obtain an adequate view of the patient’s airway. The exact technique varies with the laryngoscope blade choice, but a provider must control the tongue and epiglottis to visualize the vocal cords. The tongue is controlled by holding the laryngoscope in the provider’s left hand and sweeping it to the patient’s left. The epiglottis is controlled using the tip of the laryngoscope blade, directly when using a Miller blade, or by inserting the blade tip into the vallecula when using a MAC blade, to expose the vocal cords. Once the cords are visualized, the ET tube is inserted with the provider’s right hand until the balloon portion of the tube has just passed the vocal cords. The stylet is removed, the balloon inflated, and ventilation is provided using a resuscitation bag and reservoir. Placement is then confirmed with ETCO2 colorimetric capnometry or monitored capnography, observing equal chest rise, and auscultation of all lung fields. Special care is taken to never “rock” the laryngoscope blade in an attempt to obtain a better view. The oropharynx and epiglottis structures are to be lifted in an anterior and caudal direction to avoid damage to the teeth. Excessive force should be avoided, as this could cause damage to the soft tissues as well. There will be times that direct laryngoscopy, or the use of the video laryngoscopy, will fail on the first attempt at intubation. A provider may have difficulty identifying the necessary anatomical landmarks, need to change equipment, or misplace the ET. It is customary to allow repeated attempts, but it is generally considered a failed airway after three unsuccessful attempts (Wang HA).[10] Providers should follow the guidance of their local protocols to define a failed airway, the use of airway adjuncts, and the use of rescue devices. It is recommended that providers be skilled in BVM ventilation as well as with the use of rescue supraglottic devices and surgical airways in the case of a failed airway.[2] The most effective deterrents to a failed airway are proper training, experience, and practice.[11] Numerous recommendations have been made for the best way to acquire and maintain competency with airway procedures, but there is no substitute for experience. The National Association of EMS Physicians (NAEMSP) provides consensus recommendations on the “ideal preparation for prehospital RSI” through its position statement and resource documentation on Drug-Assisted Intubation in the Prehospital Setting.[2] Preparation to become efficient in field intubation should incorporate formal didactic training, acquisition of baseline SAI/RSI skills with clinical and operating room experience, and continuing maintenance of SAI/RSI skills. These recommendations do not set a specific number of procedures to gain and maintain competency but highlight the importance of continued education and practice. Multiple studies have tried to identify the minimum experience required to become proficient with intubation and the necessary rate of use with the procedure to maintain competency. Anesthesia literature has reported that healthcare providers require 50 endotracheal intubations to reach a success rate of 90%.[12] Wang et al. found that a prehospital provider requires 4 to 12 endotracheal intubations a year to maintain competency.[13] Such goals are difficult to reach for most prehospital providers because of a lack of quality operating room (OR) training time and exposure to field intubation in the clinical setting. Many providers only have the opportunity to perform a field intubation one time or less per year.[13] Despite the difficulty reaching the cited thresholds for training and procedure exposure, field intubation rates are improving to more satisfactory levels.[14]
Complications
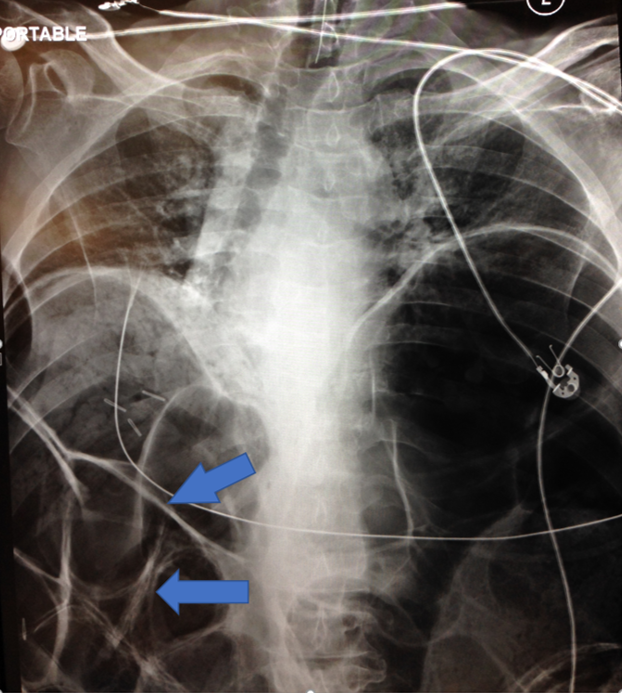
Although field intubation has been part of a prehospital provider’s scope of practice for some time, there persists a higher complication rate with prehospital intubation than in the in-hospital setting. The most catastrophic of these complications are the result of misplaced ET tubes, which can lead to hypoxia and a patient's death. Misplaced endotracheal tubes were found to occur 25% of the time in a study by Katz and Falk in a cohort of 108 field intubations.[15] This misplacement rate is markedly higher than other studies examining the frequency of tube misplacement cited by the authors (0.4% to 12%), but the actual rate may be higher than previously anticipated.[15] Most of the published studies are retrospective and rely on reported and recorded complications. Studies such as these are limited by a self-reporting bias that can lead to fewer incidents secondary to a decreased likelihood to report errors by the providers. Additionally, small sample sizes may skew the results in these studies. Katz and Falk found that the majority of misplaced tubes located in the esophagus, 67%, with the rest in the hypopharynx, 33%. Wang et al. examined the prevalence of ET intubation errors over a much larger subset of patient encounters involving intubation attempts - 1,953 patients over 18 months.[10] This study utilized an anonymous data entry system and found an overall tube misplacement rate of 3.1%.[10] Total intubation errors (including tube misplacement, four or more attempts to intubate the patient, and failed intubation) occur at a rate of 22%.[10] Although this study attempted to limit the possible under-reporting of field intubation complications by using an anonymous reporting system, the authors recognize that this bias is likely still present and feel their findings likely represent only a “best-case scenario” of field intubation error rates (Wang HA).While a misplaced tube is the most feared and devastating complication, multiple other complications can occur. There are no large studies on the rate of many of these complications in the prehospital setting, but it is expected to see similar complications to those found in the hospital setting. These complications may include :
- Dental injury
- Vocal cord injury
- Laryngeal injury
- Tracheal injury
- False passage creation
- Vomiting
- Aspiration
- Pneumonia
- Barotrauma
- Autonomic instability
- Hypoxia
Special note should be made of complications that can arise in the peri- and post-intubation phases of the procedure. Dunford et al. examined a subset of patients from the San Diego Rapid Sequence Intubation Trial, which looked at the incidence of transient hypoxia and pulse rate reactivity during field intubations.[8] This study sought to identify the rate of two complications, hypoxia and bradycardia, which can be significant detriments to good outcomes in patients with traumatic brain injuries such as those studied in the trial. It was found that over 57% of patients experienced transient hypoxia with an SPO2 < 90% for a median duration of 180 seconds. These periods of hypoxia were accompanied by marked bradycardia, the second sign of decompensation, in 19% of intubations. The estimated rate of transient hypoxia varied in other studies, ranging from 10% to 27%, much lower than what was found by Dunford et al.[8] These complications occurred despite standardized training on preoxygenation and RSI for all paramedics in the trial, and paramedics reporting that 84% of the patients who desaturated as being “easy” to intubate. The subset of patients examined by Dunford et al. were all treated by the same EMS company. This higher than average rate of hypoxia episodes shows that possible systemic issues could propagate problems when performing procedures. Because of these findings, the authors stressed that additional examination of their prescribed protocols for preoxygenation needed to be performed to find the root causes of the above-average complication rate.[8] Reexamination of protocols in the face of concerning trends is a crucial step for quality improvement within an EMS system and should be completed continuously to identify areas for improvement.Many post-intubation complications have been attributed to improper ventilation. Field intubation is a high-stress procedure. Often providers will be highly energized with adrenalin and singularly focused on the task at hand, resuscitation. In these high-stress periods, providers may over-aggressively ventilate the patient with rapid rescue breathing via a resuscitator bag. Davis et al. performed several studies examining the rate of hyperventilation and hypocarbia post field intubations in patients with traumatic brain injury and their corresponding effect on mortality.[6][7] The authors found that severe hyperventilation, defined as ETCO2 of less than 25 mmHg, led to a significantly higher mortality rate in their patient population than that which would be explained by injury patterns. This inadvertent hyperventilation was found to occur in 13.4% of patients. This number decreased to 5.6% in a similar subset of patients when ETCO2 monitors were used to monitor the ventilations. It is believed that the hyperventilation of the patients in the study caused a reduction in cerebral perfusion, again a significant detriment to good outcomes in patients with traumatic brain injury.[6][7]Aggressive resuscitative ventilation can also lead to increased airway pressures and barotrauma. This is especially true in pediatric patients who will not require a full squeeze of the resuscitation bag to receive an adequate tidal volume. It is best to try to remain calm, count out the time between breaths to once every 6 seconds or more, monitor effective ventilation with waveform capnography, and only provide a tidal volume to see the chest of the patient rise.
Clinical Significance
Field intubation can be a life-saving procedure that should be part of all ALS and critical care prehospital providers' skill set. There are clinical situations where no other options for airway control and patient ventilation are possible. Despite this need, the decision to perform field intubation should not be taken lightly. The procedure is technically difficult and fraught with complications. Multiple studies and editorials even question its utility and show concern for a trend of worse outcomes from field intubation versus basic airway management by EMS.[3][16] Few studies show a significant benefit from performing field intubation when looking at long-term survival and neurologic outcomes.[17][9][18] Most authors cite the high failed airway and complication rates along with the potential for the procedure to detract from the ability to perform other lifesaving interventions as reasons to question the utility of prehospital intubation.[3] With chest compressions, medication administration, and electrical therapy may all need to occur concomitantly during field intubation to resuscitate a patient successfully; it is challenging to manage it all in the typical two-person EMS crew.[3] Overall, there is a measurable difference in outcomes that would favor intubation performed by in-hospital providers over prehospital providers. Despite a lack of proven improvement in outcomes, authors such as Fevang et al. note, even though there is an association between prehospital intubation and a higher mortality rate than in-hospital intubation, this does not contradict the importance of the intervention.[19] There are too many moving parts and confounders to completely discredit the utility of advanced airway control in the prehospital setting. Instead, study authors call for more evidence before definitive conclusions are made.When studies examining field intubation success rates are displayed over time, there is improvement seen. The rates of successful first pass and total intubations are improving, coming closer to the in-hospital success rates for physicians.[14][18] These improvements are likely due to the increased scrutiny field intubation receives and continued attempts to improve its safety and patient outcomes. Wang et al. found significant variation in intubation failure rates across different EMS companies in their report “Paramedic Intubation Errors: Isolated Events or Symptoms of Larger problems.”[10] When we find discrepancies in treatment outcomes in similar EMS systems (Pennsylvania has statewide EMS protocols), there is an opportunity to examine why certain EMS companies show much higher success rates.[10] Additionally, small steps, such as the use of waveform capnography and the emergence of video laryngoscopy in the prehospital setting, are starting to show improved outcomes.[7][20] It is reasonable to believe that with more in-depth study into the factors that limit the success rate of field intubation and investigation of ways to overcome these barriers, successful field intubation rates will improve closer to in-hospital levels.
Enhancing Healthcare Team Outcomes
When examining the efficacy of field intubation, it is important to recognize that these procedures are not performed in a controlled environment of the ED or OR. The use of prehospital airway control is reserved for the “sickest of the sick” patients, with no other intervention available to bridge the patient until definitive treatment is obtained at a hospital facility. Based on the environmental and resource limitations providers face in the field, it may be unreasonable to expect field intubation success rates to equal those of in-hospital care, but this should not deter further examination and quality improvement measures. The focus of future studies should not only examine overall trends for the success rate of field intubations but also explore how this procedure can be made safer and identify which patients would benefit from the intervention. There should be a conscious effort, like those proposed by Carlson et al., to identify the latest improvements in training methods, equipment, monitoring, and techniques that are proven to show benefit to patient outcomes.[21] These findings should be incorporated into local protocols and training regimes. While national organizations and government oversight can help provide some direction and recommendations, the fragmented nature of EMS oversight sets the onus on the medical directors, medical oversight personnel of EMS companies, and the prehospital providers themselves to implement the necessary changes.