Introduction
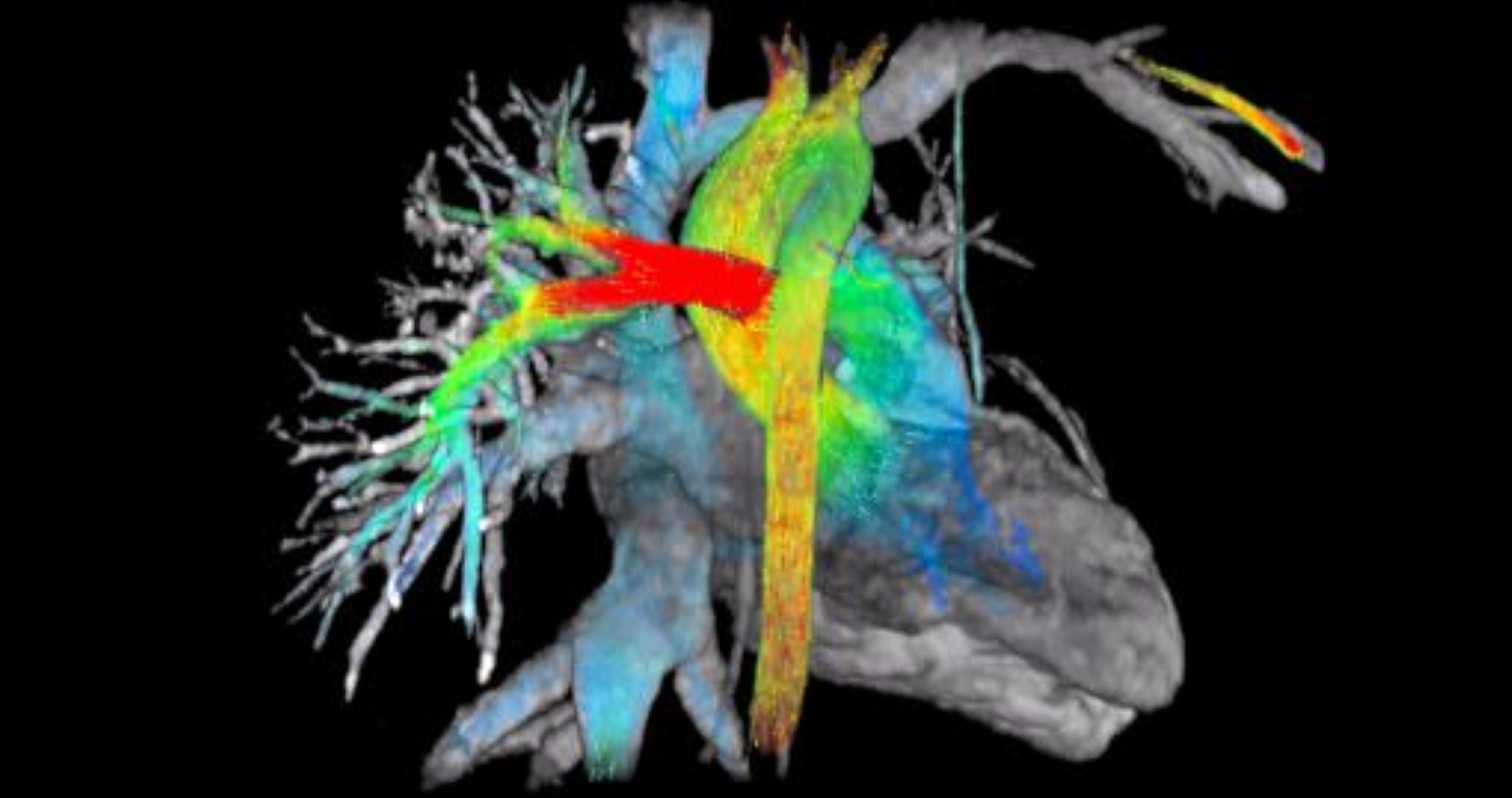
Blood flow through the body delivers oxygen, nutrients, hormones, cells, products of defense mechanisms for wound healing, and platelets. The heart pumps these products to the organs, while the vessels transport them to and from the organs. Arteries perfuse the organs and veins drain the organs of waste products. The lymphatic system helps in draining excess tissue fluid to the bloodstream. Two circulatory loops are most important to survival: the pulmonary circulation and the systemic circulation. The pulmonary circulation pumps blood from the right ventricle to the pulmonary artery. Blood exchanges carbon dioxide for oxygen while passing through the lung and the newly oxygenated blood drains into the left atrium from the pulmonary veins. The other circulatory loop is the systemic circulation, which pumps blood from the left ventricle to the aorta to the rest of the body. It transports nutrients to the intestines and hormones to endocrine glands. Waste excretion then occurs via the kidneys, intestines, lungs, and skin. Blood returns to the right atrium from the superior and inferior vena cava.[1]
Structure and Function
There are four main types of vessels in the body and have a specific role in blood flow. Arteries are thick-walled vessels that perfuse organs. Capillaries connect arteries to veins and are the main sites of nutrient/waste exchange. Capillaries have the largest total cross-sectional and surface area. Veins are thin-walled blood vessels that return deoxygenated blood to the heart. Sinusoids are substitutes for capillaries in some organs such as the spleen, liver, red bone marrow, etc. and their primary function is to elicit an immune response to foreign antigens. Each vessel plays a specific role in blood flow and is regulated by several different factors that alter flow physiology.
Arterioles are branches of arteries that are innervated by autonomic nerve fibers. There are alpha-1-adrenergic receptors on arterioles of the skin, splanchnic and renal circulations, and beta-2-adrenergic receptors on skeletal muscle. Alpha1-adrenergic receptor activation results in vasoconstriction, and beta2-adrenergic receptor activation results in vasodilation.[2] Therefore, organs with predominant sympathetic innervation, velocity, and blood flow are subject to alteration by autonomic activation. Velocity (cm/sec) is blood flow (Q) over cross-sectional area. For example, blood flow is slow at the capillaries because of the high total cross-sectional area, which allows for proper nutrient exchange. Blood flow is pressure gradient over resistance or the difference between mean arterial pressure and right atrial pressure over peripheral vascular resistance. Therefore, if alpha-1 receptors become stimulated (causing vasoconstriction), the peripheral vascular resistance increases, and blood flow decreases as well as velocity. In contrast, if beta-2 receptors become stimulated (causing vasodilation), vascular resistance decreases, and blood flow and velocity increase. Resistance is inversely proportional to the radius of the vessel, so decreased radius increases resistance, which decreases blood flow and velocity.
Embryology
When the embryo is no longer able to meet its respiratory, nutritional, and excretory needs, by simply spreading the nutrient fluids, it develops a system of vessels capable of distributing oxygen and nutrients to its tissues and transporting waste products.
Blood vessel formation begins with the development of blood islands or Wolff islets in the mesenchyme of the splanchnic mesoderm, before the yolk sac and later on the allantoid.
The blood vessels that develop in the wall of the yolk sac and the allantoid-chorion flow into an extra-embryonic network, which belongs to a pair of arteries and vitelline veins and a pair of allantoid arteries and veins which, through the umbilical cord, they penetrate the embryonic area.
Blood fluids are vital in the formation of the future child, as they generate valuable mechanotransductive information.
Blood Supply and Lymphatics
Blood flow can either be laminar or turbulent. Laminar flow is linear flow, mainly found in the middle of the vessel. Turbulent flow is any disruption in the laminar flow. Reynold’s number predicts the chances of flow being turbulent. The higher the number, the increased likelihood of being turbulent and vice versa. Reynold’s number is proportional to density, velocity, and diameter and inversely proportional to viscosity.[3] For example, high blood pressure causes increased velocity, which increases Reynold’s Number and increases the chances of turbulent flow. Anemia indicates low blood viscosity, which will also increase Reynold’s Number. Therefore, turbulence (which is identifiable on the physical exam via auscultation) could represent an underlying pathology. Shear forces can be a consequence of turbulent flow because velocity on the wall should be near zero. Disruption at the wall can damage the vessels and lead to atherosclerosis, thrombosis, and emboli.
Many organs, such as the heart, brain, and kidney, rely on autoregulatory mechanisms, or local control of blood flow, that affect perfusion. Other organs rely mostly on sympathetic stimulation or extrinsic control of blood flow. The coronary arteries are locally regulated by hypoxia and adenosine, which vasodilates the vessels to maintain oxygenation to the heart. When the heart increases in contractility, the oxygen demand of the coronary arteries increases. Therefore, vasodilation occurs to increase blood flow and oxygen to the arteries. The afferent arteries in the kidney are the main pressure-induced auto-regulators of renal blood flow and glomerular filtration rate via stretch and tubuloglomerular feedback. Carbon dioxide is the main autoregulator in the brain that stimulates cerebral vasodilation to maintain blood flow during ischemia.[4] Astrocytes also play an important role in cerebral blood flow by mediating functional hyperemia, which states that blood flow is dependent on the amount of metabolic activity. Astrocytes release vasoactive substances depending on the oxygen state of the brain. For example, during normoxic conditions, astrocytes mediate vasodilation, and during hyperoxic states, they mediate vasoconstriction. These findings have shown that astrocyte disruption causes a lack of efficient cerebral blood flow in conditions such as Alzheimer disease and diabetic retinopathy.[5] Autonomic receptors regulate blood flow to skeletal muscles at rest and metabolites during exercise. Lactate, potassium, and adenosine vasodilate the vessels during exercise.[6] This vasodilation during exercise is essential for the proper delivery of oxygen skeletal muscle and the removal of waste products and heat.[7] The skin has the highest amount of sympathetic innervation, mainly for temperature regulation. Vasoconstriction to maintain core body temperature during cold climates and vasodilation to dissipate the heat in hot climates.[8]
Nerves
Baroreceptors located on the carotid sinus response to the decreased pressure (low blood pressure), which signals to activate the sympathetic nerves and vasoconstricts arteries and veins.[9] The chemoreceptors in the carotid and aortic bodies are sensitive to oxygen pressures and respond with vasoconstriction if the partial pressure of oxygen is too low.[10] Vasopressin or anti-diuretic hormone (ADH) is a vasoconstrictor released from the posterior pituitary in response to low blood volume. In contrast, atrial natriuretic peptide (ANP) is a vasodilator released from the atrium in response to fluid overload in the heart.
Clinical Significance
A multitude of factors regulates blood flow throughout the human body. Each organ has its way of altering the flow, depending on certain conditions. Understanding the mechanisms behind perfusion is essential for the treatment of diseases associated with blood flow pathophysiologies such as myocardial infarction, hypertension treatment, and stroke.
Other Issues
The blood flow can vary its intensity, direction, type of flow (laminar, turbulent, etc.), entity. These processes involve different mechanical signals to the tissues, with mechanotransductive responses specific to the type of flow.[11]