Continuing Education Activity
Bezold's abscess is a rare deep neck abscess and is an intratemporal complication of a coalescent mastoiditis via direct extension into the peri-mastoid tissues. It was first described by a German otologist Dr. Friedrich Bezold in 1881. Since the introduction of antibiotics, the number of reported cases of Bezold's abscesses has significantly decreased. According to some authors, since 1967 there have been fewer than 100 reported cases in the English literature, of which only four cases occurred in children under the age of five. This activity reviews the cause, pathophysiology, and presentation of Bezold abscess and highlights the role of the interprofessional team in its management.
Objectives:
- Describe the pathophysiology of Bezold abscess.
- Review the presentation of a patient with bezold abscess.
- Outline the treatment and management options available for bezold abscess.
- Summarize interprofessional team strategies for improving care coordination and communication to advance the treatment of bezold abscess.
Introduction
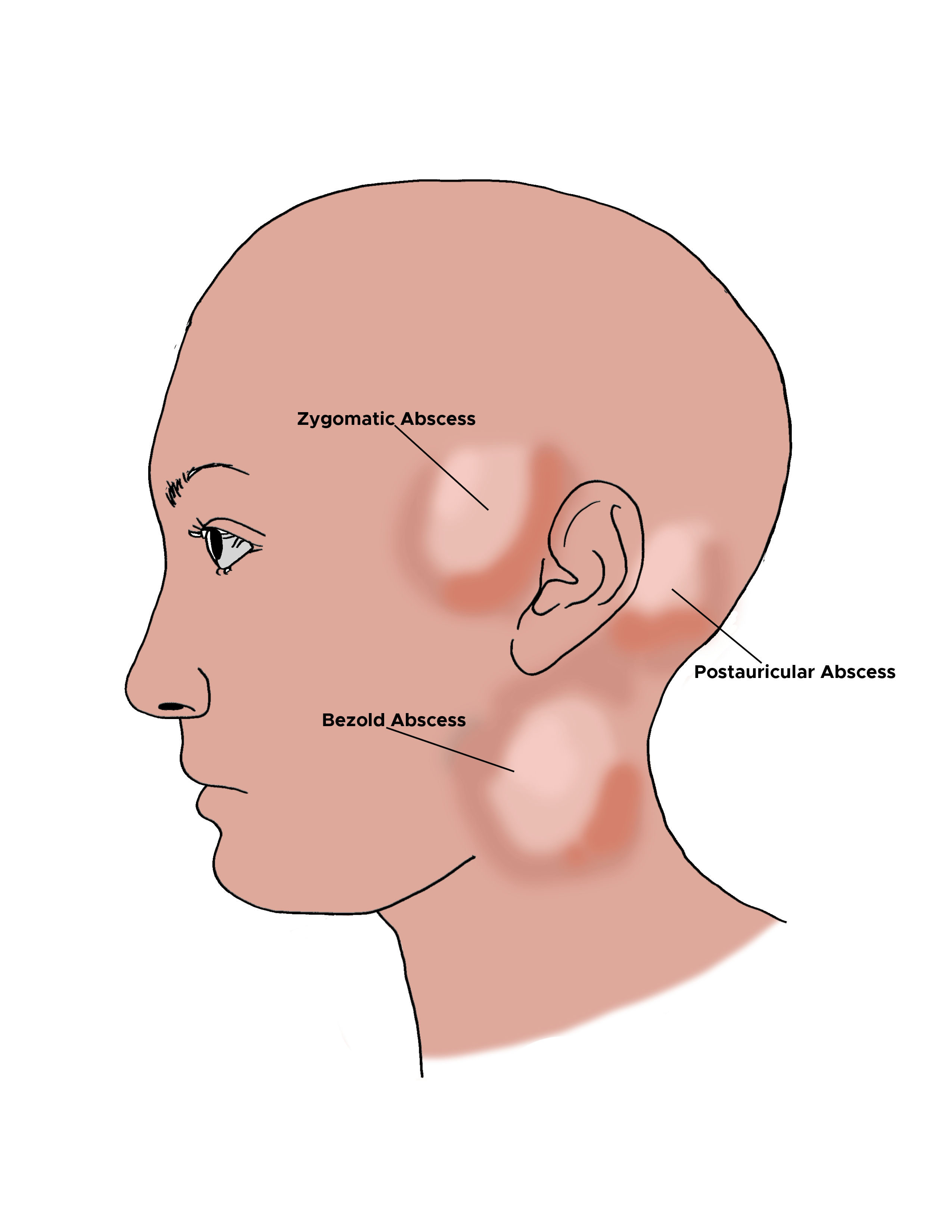
Bezold's abscess is a rare deep neck abscess and is an intratemporal complication of a coalescent mastoiditis, wherein the infection erodes through the lateral mastoid cortex medial to the attachment of the sternocleidomastoid (SCM) muscle. Once the infection has reached this space, it can progress into the infratemporal fossa and travel deep to the investing layer of the deep cervical fascia. The spread of infection in this layer can lead to a progressive cellulitis/abscess, but can also proceed toward the carotid sheath, and thrombosis of the internal judular vein can occur. It was first described by a German otologist Dr. Friedrich Bezold in 1881. Since the introduction of antibiotics, the number of reported cases of Bezold's abscesses have significantly decreased. According to some authors, since 1967 there have been fewer than 100 reported cases in the English literature, of which only four cases occurred in children under the age of five. [1][2][3]
Etiology
The organisms commonly cultured from Bezold's abscesses include gram-positive aerobes: Streptococcus, Staphylococcus, and Enterococcus species; gram-negative aerobes: Klebsiella, Pseudomonas, and Proteus species and anaerobes, particularly Peptostreptococcus and Fusobacterium species. These are the same organisms implicated in coalescent mastoiditis, from which this condition develops. While this infection is exceedingly rare in modern times, immunosuppressed patients and patients in areas without access to antibiotic treatments remain at higher risk. [1]
Epidemiology
Many factors have been shown to play a role in the development of acute, chronic, and suppurative otitis media in children. Bezold's abscess is perhaps the penultimate complication of suppurative otitis media (SOM). If SOM is left untreated or unrecognized, it can progress to a Bezol's abscess. Risk factors include the following:
- Socioeconomic conditions: there is an increase in the number of cases in children living in poorer socioeconomic conditions.
- Daycare: there appears to be an increase in children attending daycare.
- Underlying medical conditions that affect the Eustachian tube function: children with cleft palate, craniofacial anomalies, congenital or acquired immune dysfunction, conditions affecting the ciliary function of the Eustachian tube and middle ear mucosa.
In adults, medical considerations that must be considered include the patient's HIV status, history of uncontrolled diabetes, renal failure, and patients who are immunosuppressed for other reasons. Additionally, patients with chronic, untreated ear disease who are without access to regular medical care and antibiotics may present with such late, severe, manifestations of SOM.[4]
Pathophysiology
The most important contributing factor to the development of a Bezold's abscess is the presence of a well-aerated and pneumatized mastoid bone. At birth, the mastoid bone consists mainly of an antral cell. From this antral cell, air cells begin to develop until there is complete pneumatization of the mastoid bone around the age of five. As the process of pneumatization of the mastoid bone occurs, the surrounding walls of the mastoid bone thin, particularly at the tip of the mastoid bone on its medial surface along the incisura digastrica (digastric groove), where the digastric muscle attaches. If the infection is left unchecked, the outer walls of the mastoid tip become involved with the spread of the infection along the sternocleidomastoid muscle, the trapezius, and splenius capitis muscles. Secretions and bacteria can enter the middle ear through the eustachian tube and from the middle ear can pass directly into the mastoid bone through a small opening the aditus ad antrum. During an inflammatory process (suppurative otitis media), obstruction of the aditus ad antrum occurs. Purulent secretions cannot escape and will accumulate in the mastoid bone. The pressure created by this purulent material with its enzymatic activity within the mastoid bone causes osteitis and osteonecrosis of the fragile pneumatized air cells further thinning the walls of the mastoid bone. This stage is called coalescent mastoiditis. The inflammatory process can spread in many directions. If it spreads inferiorly towards the mastoid tip, the purulent material will eventually erode the very thin bone along the digastric ridge at the insertion of the digastric muscle. Consequently, a purulent material will spread into the neck between the digastric and sternocleidomastoid muscles.[5][4][5]
History and Physical
Bezold's abscess may occur in both children and adults with well-developed mastoid bones. Both may have had a history of recurrent otitis media or chronic otitis media with tympanic membrane perforation and a draining ear. Prior mastoid surgery for cholesteatoma normally causes further thinning of the mastoid walls making it easier for infection to spread in this way. An important early clinical sign of a coalescent mastoiditis on physical examination is sagging of the posterior superior external auditory canal. Other common clinical signs include the following:
- neck pain
- swelling in the lateral neck
- postauricular tenderness over the affected mastoid bone
- otalgia
- otorrhea
- hearing loss
If any of the above is documented, and the patient presents with fever with an associated neck mass one should have a high index of suspicion that the infection has spread to adjacent regions within the head and neck. Thus a thorough head and neck evaluation should always be conducted. In the differential diagnosis, one must always consider an abscess of post-auricular lymph nodes, other deep neck space abscesses from oropharyngeal or odontogenic sources, and malignancy. If CT scanning is not available, then a simple lateral x-ray of the temporal bone may be helpful in ascertaining the status of the mastoid air cell system. A thorough cranial nerve examination is essential, as the progression of the infection into the infratemporal fossa can cause cranial neuropathies.[6]
Evaluation
Laboratory evaluations are often not helpful since the leukocyte count and erythrocyte sedimentation rate may be normal or elevated; the initial diagnosis is a clinical one. Contrast-enhanced computed tomography (CT) of the neck should be obtained if there is any indication or suspicion of a deep neck abscess, regardless of a lack of evidence of an infection in the mastoid bone since prior antibiotics may have truncated the infection in the mastoid bone while the abscess was still developing in the neck. Recently, in the emergency room setting, a bedside soft-tissue ultrasound with the use of a high-frequency linear array probe to the mastoid was used to detect a complex hypoechoic-anechoic fluid collection in the neck. An intravenous contrast CT scan was used to confirm the ultrasound findings, and both an abscess in the neck and ear pathology were identified. If there is a palpable fluctuance, needle aspiration at the bedside can be attampted, but great care should be taken.[7][8]
Treatment / Management
If a Bezold's abscess is present or suspected, practitioners should use intravenous broad-spectrum antibiotics. Once antibiotic therapy is initiated, a contrast-enhanced CT scan should be obtained. Naturally, cultures are important, particularly with a diabetic or immunocompromised patient since the bacteriology in these cases may be different. If a fluid collection is identified on CT, surgical drainage is indicated via a trans-cervical approach. If this fluid collection exists concurrently with a coalescent mastoiditis, a post-auricular incision is made, and a simple, complete mastoidectomy should be performed in addition to the drainage of the deep neck portion of the abscess. This may require separate incisions to avoid damage to the greater auricular nerve, the facial nerve, and the accessory nerve, though a single incision can also be used if meticulous technique is employed in the dissection. The objective is to remove as much osteitic bone and granulation tissue present in the mastoid bone as possible. If there is concurrent suppurative OM, a tympanostomy tube (grommet) should be placed concurrently. In rare cases, a Bezold's abscess may appear in children before there is a complete development of the mastoid air cell system. In these patients, the practitioner must pay particular attention to the position of the facial nerve. Therefore, they should not make a standard post-auricular incision since the facial nerve may be more superficial than anticipated. In this case, a post-auricular superior linear incision is made to drain the purulent material and carefully debride as much granulation tissue as possible and a tympanostomy tube placed. At the same time, the neck abscess should be thoroughly drained. Broad-spectrum antibiotics with good cerebrospinal fluid penetration should be continued until culture results are obtained to prevent further extension of the inflammatory process to adjacent vascular structures.[1][9]
Differential Diagnosis
- Other deep neck abscess (parapharyngeal, retropharyngeal, odontogenic, etc.)
- Cutaneous abscess
- Suppurative lymphadenoapthy
- Malignancy
- Parotid lymphoepithelial cyst
- Parotid malignancy
- Suppurative parotitis
- Tuberculosis
- Coalescent mastoiditis
Prognosis
The prognosis is good if the infection has not spread beyond the temporal bone and, if antibiotic intervention occurs early on.
Complications
If the infection is not contained and treated, the infection may spread to the following areas:
- sigmoid sinus
- transverse sinus
- meninges
This is as a result of spread intracranially. The infection more commonly spreads along the investing layer of deep cervical fascia, leading to:
- Jugular vein thrombosis
- Cranial neuropathies
- Trismus
- Superficial extension with cutaneous fistula formation
Long-term complications can include:
- Death
- Meningitis
- Cranial neuropathy
- Hearing loss
Consultations
- ENT
- Neurosurgeon
- Infectious disease
Pearls and Other Issues
Because of the advent of antibiotic therapy in the treatment of acute, chronic, and suppurative otitis media, Bezold's abscesses are rarely seen in areas with developed healthcare systems. Still, practitioners should have a high index of suspicion in cases where patients present with a neck mass and clinical signs of previous ear pathology or concurrent ear pathology, particularly in areas of developing healthcare infrastructure or other significant barriers to accessing routine healthcare, or in the immunosuppressed.
Enhancing Healthcare Team Outcomes
Bezold's abscess is a deep neck abscess resulting from a complication of coalescent otomastoiditis. Bezold's abscess is not a common condition and is unlikely to be seen by most surgeons in their practice. However, even though rare, it has to be considered in the differential diagnosis of neck abscesses and otologic pathologies. If the diagnosis is delayed, the abscess can extend both extracranially and intracranially, causing significant morbidity.
The diagnosis of a Bezold abscess can be missed if it is simply considered to be just another neck abscess. For this reason, an interprofessional team with a systemic approach to neck abscesses is recommended. Once a neck abscess around the ear is noted, the following should be consulted:
- Radiology to obtain imaging tests to determine the origin, location, and extent of the abscess
- ENT for debridement and drainage of the abscess and mastoidectomy/tympanostomy tube placement
- Laboratory technologists to determine the type of bacterial growth
- Pharmacists to recommend the most appropriate antibiotics and manage the emesis
- Nurses to monitor vital signs and presence of altered mental status
- Neurologist to monitor the patient for neurological deficits (e.g., facial paralysis)
- Neurosurgeon if there is an intracranial extension of the abscess.[10]
Outcomes
Outcomes reports of Bezold's abscess and its management are in the realm of case reports and series, owing to its rarity. There are no randomized clinical trials that have evaluated treatment or outcomes. The few isolated reports indicate that when the condition is diagnosed promptly and treated with drainage, the prognosis is good. The key is prompt drainage.[1] (Level III) However, delays in diagnosis and treatment can lead to poor outcomes and even death.