Introduction
The cervical plexus is a complex neurologic structure located within the head and neck. The large portion of the cervical plexus is the communication between the anterior divisions of C1 through C4 nerves. While the plexus itself can be complex, it is essential for practitioners to understand the significant motor and sensory functions of the cervical plexus as this information can provide valuable information when treating a patient with a possible insult to this area.
Structure and Function
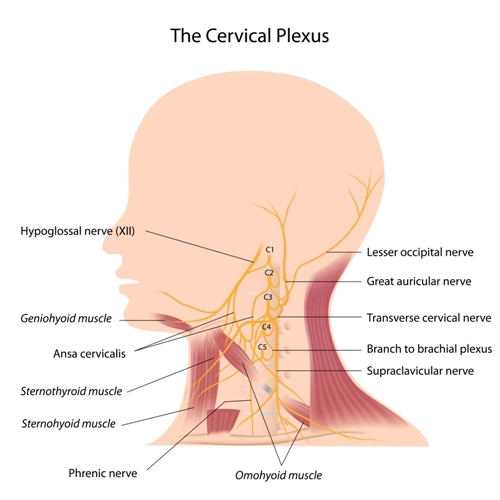
The function of the cervical plexus is to provide a network of branches that give sensory and muscular innervation to structures within the head, neck, and trunk. Some branches also receive contributions from cranial nerves as they innervate their corresponding tissues. The cervical plexus is more specifically two separate plexuses, one superficial, and the other deep. The superficial plexus is made up of the lateral terminal branches which turn into loops that give the sensory branches of the cervical plexus and become the great auricular nerve, the external acoustic meatus, the transverse cervical nerve, the lesser occipital and supraclavicular nerves. The deep plexus then becomes the muscular branches which include the ansa cervicalis, the phrenic nerve, and various segmental branches.[1]
Embryology
The ventral roots of the spinal nerves are derived originally from the mantle layer of the neural tube. The processes from the neuroblasts in this mantle layer assemble into rootlets that exit in a continuous longitudinal series on the ventrolateral border of the neural tube. The direction taken by the ventral root fibers as they emerge from the tube varies according to the size and position of the ganglion crest. The superficial cervical plexus originally forms by the anterior branch fusion of C2 andC3 which forms the descendens cervicalis; this then unites in a loop with the hypoglossal nerve and together with the first cervical nerve, is incorporated into the plexus. The deep plexus is made up of the lateral terminal branches.[2] While the development of the cervical plexus is a complex process, there has been one major branch of the deep cervical plexus accurately detailed during development, this being the phrenic nerve. During development, the diaphragm develops near the newly developing nerves. Some literature describes the phrenic nerve developing directly ventral to the diaphragm during development. As the fetus continues to grow, the points of origin and insertion of the phrenic nerve draw gradually apart due to the descent of the diaphragm and the elevation of the cervical nerves as it accompanies the development of other structures in the neck.[3]
Blood Supply and Lymphatics
While the nerves receive their blood supply through various tributaries throughout their course, the vessels that course near the cervical spinal cord are the vertebral arteries. Additionally, there is one anterior spinal artery, two posterior spinal arteries, an anterior and posterior radicular artery, and an arterial vasocorona. This arterial vasocorona is an anastomosis between the spinal arteries. It consists of the anterior and two posterior spinal arteries, which are direct branches of the two vertebral arteries which form the basilar artery. The anterior spinal artery runs along the anterior median fissure while the two posterior spinal arteries run along the posterolateral sulcus bilaterally. These posterior spinal arteries run along the line of attachment of the dorsal nerve roots. The anterior spinal artery does give off branches that enter the spinal cord through the anterior median fissure.[4]
Nerves
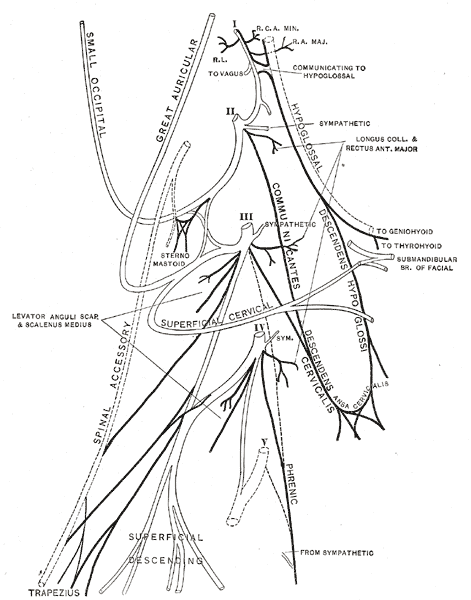
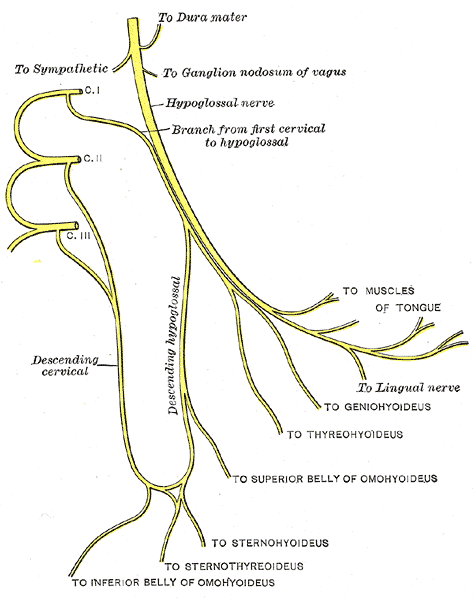
The cervical plexus lies deep to the internal jugular vein and the sternocleidomastoid muscle and on the surface of the scalenus medius and levator scapulae muscle. The nerves are also located laterally to the transverse processes between prevertebral muscles on the medial side and other vertebral muscles from the lateral side. The primary rami, besides C1, divides into two. C1 joins the upper branch of C2, and the adjacent upper and lower branches of C2 and C3, as well as C3 and C4, fuse. The lower branch of C4 joins C5 and contributes to the brachial plexus. The branches emerge from the posterior border of the sternocleidomastoid muscle.[5]
The cutaneous branches of the cervical plexus all emerge near the midpoint of the posterior border of the sternocleidomastoid muscle. One of those nerves, the lesser occipital nerve, originates from C2 and ascends the posterior border of the sternocleidomastoid muscle to supply the skin of the upper neck and the scalp behind the auricle. The great auricular nerve gains innervation from both C2 and C3 ascends across the sternocleidomastoid to reach the skin of the parotid gland on the lateral part of the face just anterior to the auricle. The transverse cervical nerve also has roots from C2 and C3, but it crosses the sternocleidomastoid horizontally, deep to the platysma to supply the skin along the anterior triangle of the neck. Lastly, the supraclavicular nerves, which come from C3 and C4 descend initially as one trunk behind the sternocleidomastoid and then divide near the clavicle to supply the skin over the shoulder and the upper pectoral region.[6][7]
The muscular branches pass deeply from the plexus to supply the rhomboids, the serratus anterior, the sternocleidomastoid, the trapezius, levator scapulae, and the scalenus medius. There are also branches that supply the muscles of the suboccipital triangle.
The communicating branches contributing to the plexus from the sympathetic nervous system are from the gray ramus communicantes from the superior cervical sympathetic ganglion. The plexus also gives a communicating branch from C1 to the hypoglossal nerve which then almost immediately leaves to supply the geniohyoid and thyrohyoid muscles.
The phrenic nerve deserves careful consideration due to its motor, sensory, and sympathetic nerve fibers to the diaphragm. It originates at the lateral border of the scalenus anterior at the level of the upper border of the thoracic cavity and passes anterior to the subclavian artery.[8]
Surgical Considerations
Cervical plexus blocks are commonly used in this region to promote anesthesia and regional pain block for surgical procedures in the neck region. Such procedures include cervical fat pad biopsy, lymph node biopsy, or other superficial surgical procedures in the neck. If done correctly, this type of block produces anesthesia over the neck, occipital region, the shoulder region, and the upper pectoral region. Firstly, to achieve this nerve block correctly, it is necessary to inject an analgesic solution subcutaneously around the midpoint of the posterior border of the sternocleidomastoid. It is through this anesthetized skin that the areas lateral to the transverse processes of the second, third, and fourth cervical vertebrae should be infiltrated. Avoiding intrathecal and intravascular injection during this approach is essential. One case study also reported injections into the phrenic and vagus nerves while another showed a Horner syndrome following this procedure.[9]
If more radical surgical interventions are required, such as dissections of the neck, excision of masses, thyroglossal cysts, operations on the trachea and larynx and even carotid endarterectomy, then local anesthetic must be administered under the carotid sheath. This injection must be under the adventitia of the carotid bifurcation and into the superior angle of the incision. Unfortunately, thyroidectomies are usually not performed using this method as the bilateral blockade gives a choking sensation to the patient and the potential for a bilateral phrenic blockade.[10]
Clinical Significance
The triangles of the neck are commonly an interest to various surgical subspecialties. Of the triangles of the neck, the posterior triangle is the location of the posterior cervical plexus. It is vital for professional medical staff to be familiar with these structures and their respective functions. Ultrasound is used to identify the cervical plexus during such nerve blocks. As noted above, the most common indications for these blocks is a carotid endarterectomy and also superficial neck surgery.