Introduction
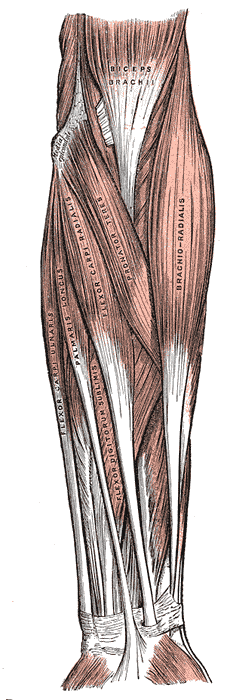
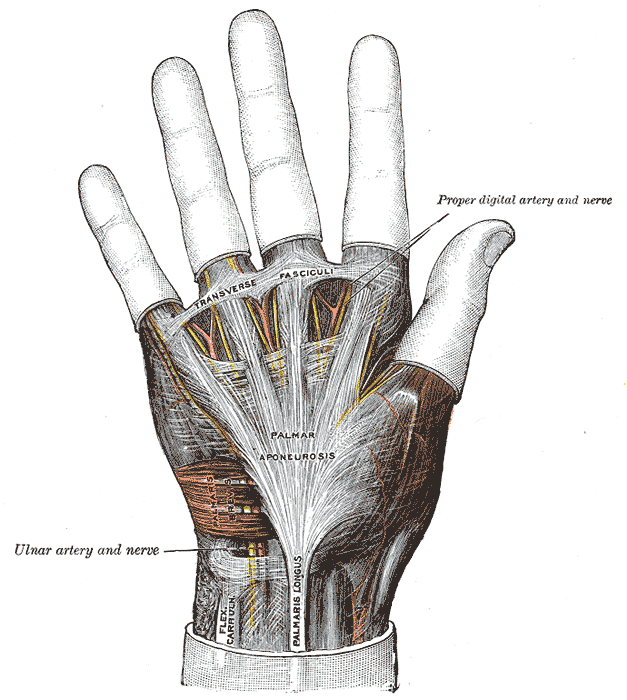
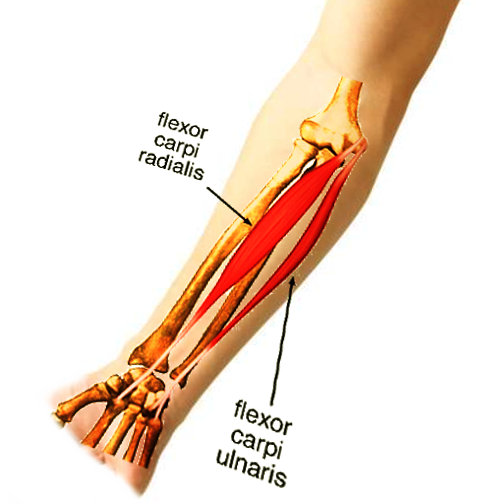
The flexor carpi ulnaris (FCU) is a superficial flexor muscle of the forearm that flexes and adducts the hand (see Image. Anterior Forearm Compartment Muscles). This muscle is the most powerful wrist flexor and the only anterior forearm compartment muscle completely innervated by the ulnar nerve. The FCU tendon is a landmark for locating the ulnar nerve and artery during surgery, as these structures lie immediately lateral to the muscle (see Image. Hand Ligaments and Fascia).
Chronic wear and tear and trauma are the most frequent causes of FCU injuries. In surgery, this muscle is vital to wrist procedures like wrist and hand tendon transfers and cubital tunnel release. Understanding the FCU's surgical importance is essential for healthcare professionals treating conditions affecting the forearm, wrist, and hand.
Structure and Function
The FCU originates from 2 separate heads connected by a tendinous arch. The humeral head arises from a common flexor tendon origin on the medial humeral epicondyle. In contrast, the ulnar head arises by an aponeurosis from the olecranon and proximal three-fourths of the ulna's subcutaneous margin.
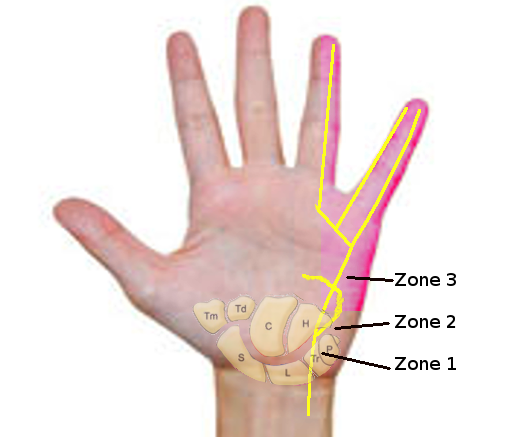
The FCU inserts on the 5th metacarpal, hook of the hamate, and pisiform. The muscle is attached to the hook of the hamate via the pisohamate ligament and the 5th metacarpal bone through the pisometacarpal ligament.[1] The Guyon canal is a depression between the pisiform and hook of the hamate (see Image. Guyon Canal Zones.). The borders of this canal include the volar carpal ligament anteriorly, transverse carpal ligament posteriorly, hook of the hamate laterally, and pisiform and pisohamate ligament medially.
The FCU is the most medial among the superficial anterior forearm compartment muscles. The ulnar nerve and artery are situated immediately lateral to the FCU tendon at the wrist level.
The FCU primarily flexes the wrist and is the most powerful wrist flexor. The muscle also assists in wrist adduction and elbow and forearm flexion.[2]
Embryology
The upper limb musculature arises from the dorsolateral somite cells that move into the limb bud around the 4th to 5th week to form muscles.[3] With limb bud growth, newly formed connective tissue from the lateral plate mesoderm divides the muscle masses into extensor and flexor components.
Fibroblast growth factor synchronizes the developmental schema between the anteroposterior and proximodistal axes by promoting Sonic hedgehog expression in the zone of polarizing activity. In turn, Sonic hedgehog ensures that fibroblast growth factor is present in the apical ectodermal ridge, creating a positive feedback loop.[4] Once the limb buds form, the primary ventral rami pass through the mesenchyme. The ulnar nerve then arises to eventually supply the FCU.
Blood Supply and Lymphatics
The posterior ulnar recurrent collateral arteries and small ulnar artery branches supply the FCU. The ulnar artery is situated laterally to the FCU tendon and ulnar nerve. Pulsations of this artery can be palpated in this region.
The FCU lymphatic drainage is via the upper limb's superficial and deep lymphatic vessels. The superficial vessels around the basilic vein drain to the cubital lymph nodes, which are proximal to the medial humeral epicondyle. The lymph vessels around the cephalic vein empty into the axillary lymph nodes. The deep lymphatic vessels also drain lymph from the FCU and follow the major deep veins, eventually terminating in the humeral axillary lymph nodes.[5]
Nerves
The FCU is innervated by the ulnar nerve's muscular branch, which arises from the C7 and C8 nerve roots. The ulnar nerve enters the forearm between the 2 heads of the FCU. Distally, the ulnar nerve passes the wrist lateral to the FCU tendon, superficial to the flexor retinaculum, and within the Guyon canal.[6]
Muscles
The FCU is one of the superficial flexor muscles of the forearm, along with the pronator teres, flexor carpi radialis, palmaris longus, and flexor digitorum superficialis (FDS). These superficial forearm flexor muscles attach onto the medial epicondyle of the humerus through a common flexor tendon. The FCU is the most medial of these muscles.
Physiologic Variants
The accessory FCU is a physiologic variant that can arise in a plane anteromedial to the FDS or between the FCU and FDS, extending to the FCU's radial aspect. According to one case report, this variant originates from the medial epicondyle 1 cm posterolateral to the FCU origin and forms a separate tendon 5 cm above the flexor retinaculum's proximal border.[7] Distally, the tendon inserts into the flexor retinaculum and wrist bones, including the triquetral and hamate.
Various insertions and origins have been described for accessory FCU muscles. The brevis variant may insert into the pisiform, hook of the hamate, abductor digiti minimi, or 5th metacarpal. Others may insert on the flexor pollicis longus tendon, index finger tendon of the flexor digitorum profundus (FDP), or triquetral bone. Anomalous anatomical structures in the Guyon canal may compress the ulnar nerve.[8] Importantly, ulnar artery thrombosis has been reported in association with an abnormal FCU variant reaching the Guyon canal distally. Knowledge of these anatomic variants aids significantly in preoperative surgical planning.
Surgical Considerations
The FCU is a surgical landmark used for exposing the ulnar shaft in procedures like the following:
- Open reduction and internal fixation of ulnar fractures
- Ulnar osteotomy
- Ulnar lengthening or shortening
- Treatment of the ulnar fibrous anlage in ulnar clubhand
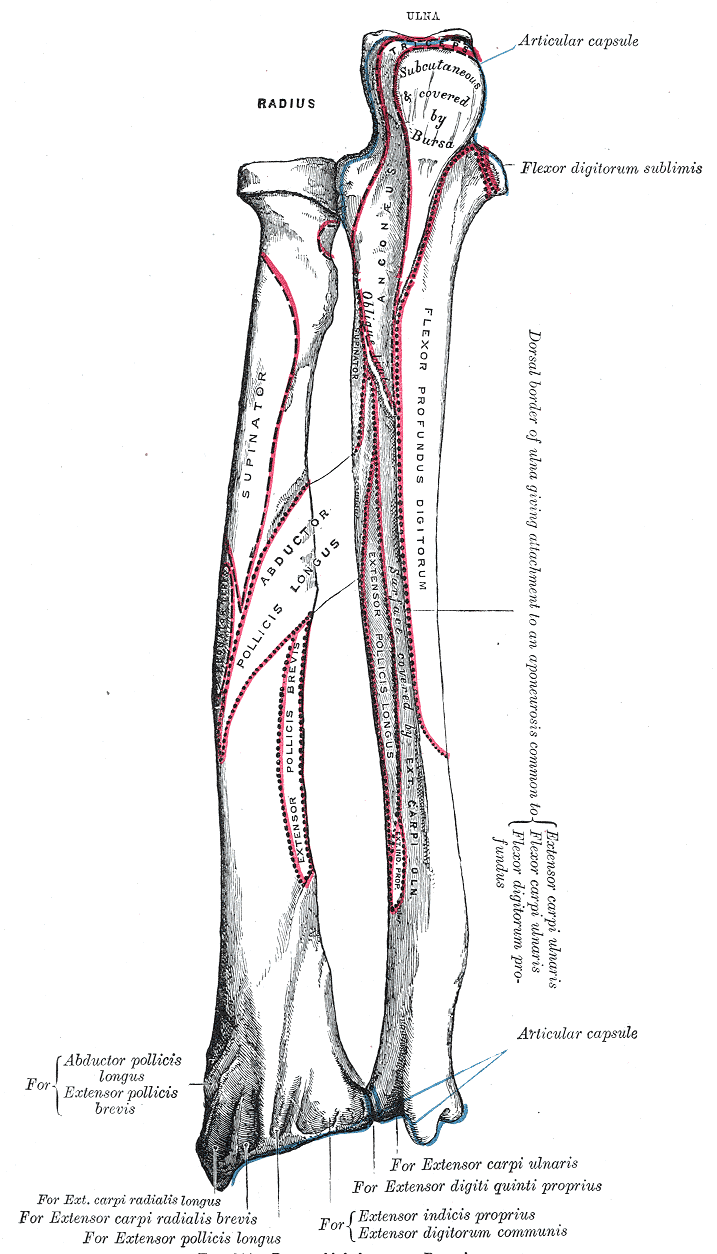
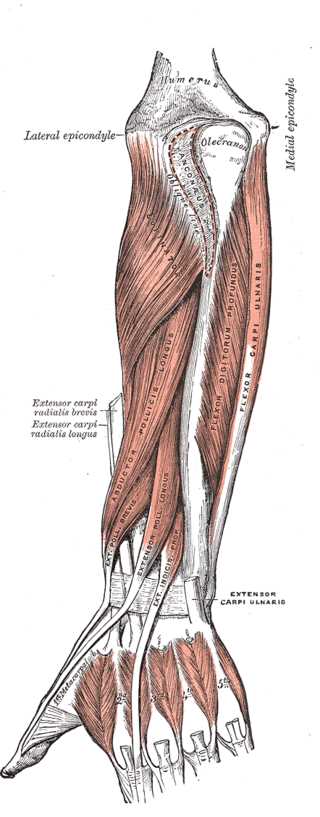
Ulnar shaft exposure allows access to the internervous plane between the extensor carpi ulnaris and FCU (see Image. Muscles of the Forearm, Wrist, and Hand). The ulnar nerve enters the forearm between the 2 heads of the FCU and runs deep to the FCU tendon at the wrist level. Care must be taken when stripping the FCU from the ulna epiperiosteally, which risks injuring the ulnar nerve (see Image. Bone Markings on the Radius and Ulna).[9]
The FCU is also important when taking a volar approach to Guyon canal decompression surgery. This procedure releases the ulnar nerve from entrapment. The volar carpal ligament is a continuation of the deep palmar fascia and FCU fibers. The FCU fascia is incised to allow muscle retraction and reveal the ulnar nerve and artery. The ulnar nerve and artery lie just deep to the FCU and volar carpal ligament. Care must be taken to avoid ulnar nerve and artery injury during superficial and deep surgical dissection of this area.[10]
Cubital tunnel syndrome arises from ulnar nerve compression in the proximal forearm region, where the nerve runs between the 2 heads of the FCU. Subcutaneous ulnar nerve transposition requires releasing the deep and superficial aponeuroses covering the 2 FCU heads. A transverse fascial arc distal to the FCU hiatus is also released to avoid iatrogenic compression. The ulnar motor branches are at risk of inadvertent ligation when incising the FCU and its associated soft-tissue structures.
Clinical Significance
The FCU, FDS, and FDP protect the forearm's neurovascular bundle, which consists of the ulnar artery and vein and the venae comitantes. The FCU is an important anatomical guide when flexing and ulnarly deviating the wrist (see Image. Forearm Muscles).
The cubital tunnel is the region between the 2 FCU heads. The Osborne ligament connects the 2 FCU heads and is a continuation of the fibroaponeurotic covering of the epicondylar groove. Cubital tunnel syndrome is a condition arising from compression of the ulnar nerve between the 2 FCU heads and their aponeurosis. This condition is the second most common upper extremity compression neuropathy.[11] Symptoms include paresthesias of the small finger, ulnar half of the ring finger, and ulnar dorsal hand. The condition is exacerbated at night by sleeping with the arm in flexion, as the cubital tunnel flattens when the ligament stretches during arm flexion, increasing pressure against the nerve.
Prolonged compression of the ulnar nerve by the FCU may reduce sensation in the ulnar 1-1/2 digits. Patients may also complain of a weak grasp and thumb pinch. Patients may also demonstrate Froment's paper sign, which is the inability to hold slim objects between the thumb and index finger due to weak metacarpophalangeal joint flexion and thumb adduction.[12] Muscle wasting and clawing of the ring and small fingers indicate chronic compressive syndrome.[13]
Other Issues
FCU tendinopathy is an overuse injury presenting with focal volar and ulnar-sided wrist pain. The pain may be reproduced by wrist flexion and ulnar deviation. The pisiform is a sesamoid within the FCU tendon contributing to tendonitis-related wrist pain.[14]