Continuing Education Activity
Wrist arthrodesis, also known as wrist fusion, is a procedure in which the wrist joint is immobilized by fusing the radius to the carpal bones. It may involve the entire wrist joint or partial wrist joint in techniques such as scapholunate fusion, four-corner fusion with scaphoid excision, scapho-trapezoid fusion, scaphocapitate fusion, and radiolunate fusion. This activity highlights the role of the interdisciplinary team in this procedure.
Objectives:
- Outline the indications for wrist arthrodesis.
- Describe the complications of wrist arthrodesis.
- Summarize the surgical steps of wrist arthrodesis.
- Explain the importance of the interprofessional approach to a patient who is due to undergo a wrist arthrodesis.
Introduction
Wrist arthrodesis, also known as wrist fusion, is a procedure in which the wrist joint is immobilized by fusing the radius to the carpal bones. It is a procedure used for pain relief purposes in conditions such as advanced wrist arthritis, following wrist fractures, or severe ligament injuries. This procedure is performed when all other treatment options have failed to control the patient's symptoms.[1][2]
Wrist arthrodesis may involve the entire wrist joint or partial wrist joint in techniques such as scapholunate fusion, four-corner fusion with scaphoid excision, scapho-trapezoid fusion, scaphocapitate fusion, and radio-lunate fusion. Whether arthrodesis is total or partial, the goal is to provide pain relief and to preserve as much function as possible in the wrist joint. This article refers to total wrist fusion as a surgical procedure.
Anatomy and Physiology
The wrist joint is represented by the distal radioulnar joint, the radiocarpal joint, and the intercarpal joint.
The distal radioulnar joint is a pivot joint that articulates the head of the ulna with the ulnar notch of the distal radius. It works together with the proximal radio-ulnar joint to produce pronation and supination of the forearm. Lister's tubercle is a bony prominence located on the distal radius and can be palpated on the dorsal aspect of the wrist. It serves as a pulley for the extensor pollicis longus tendon and also as a surgical landmark.
The radiocarpal joint is an ellipsoid joint formed by the distal end of the radius and the proximal row of carpal bones. The carpal bones on the ulnar side only make intermittent contact with the ulna in ulnar deviation of the wrist. The capsule of the radiocarpal joint is lax and thin on the dorsal surface and is continuous with the midcarpal joints. It is straightened by numerous ligaments, which include the palmar and dorsal radio-carpal ligaments, as well as the radial and ulnar collateral ligaments.
There are 8 carpal bones organized in 2 carpal rows. The proximal row is represented from lateral to medial by the scaphoid, lunate, triquetrum, and pisiform. The pisiform bone does not articulate with the radius. The distal carpal row is made from lateral to medial by the trapezium, trapezoid, capitate, and hamate. The distal row of carpal bones articulates with the metacarpal bones.
The space of Poirier is a central weak area of the wrist, which is located on the floor of the carpal tunnel at the level of the proximate aspect of the capitate bone. It is delimited by the radioscaphocapitate ligament and the volar long radio-lunate ligament. It disappears in wrist flexion, and it is accentuated in wrist extension, and this space is where the lunate bone can dislocate in lunate dislocations.
The bony anatomy is completed further by a large number of ligaments, flexor tendons which pass through the carpal tunnel and ulnar tunnel on the volar aspect of the wrist, extensor tendons which pass through 6 extensor compartments on the dorsal aspect of the wrist, the radial, ulnar and median nerves with their branches as well as the radial and ulnar arteries with their anastomotic arches.[3][4]
There are three axes of motion within the wrist joint:
1. Flexion-extension: flexion is produced 40% by the radiocarpal joint and 60% by the mid carpal joint while extension is produced 66% by the radiocarpal joint and 33% by the mid-carpal joint.
2. Radial-ulnar deviation: the radial deviation is produced 90% by the mid carpal joint while the ulnar deviation is produced 50% by the radio-carpal joint and 50% by the midcarpal joint.
3. Pronation-supination which is produced at the proximal and distal radio-ulnar joints.
The distal radius bears 80% of the load of the wrist while the distal ulna bears 20% of the load of the wrist.[5]
Indications
Pain and instability resulting from wrist arthritis is the most common indication for wrist arthrodesis, and it can be caused by a multitude of factors. Depending on its location, the most common form of wrist arthritis is the scapholunate advanced collapse or SLAC. The second most common form of arthritis is the scaphotrapezial-trapezoidal arthrosis, which can be identified in approximately 40% of wrist radiographs. Other forms of arthritis, depending on the location of the injury, are the scaphoid nonunion advanced collapse or SNAC, the distal radio-ulnar joint arthrosis, and the pisotriquetral arthrosis.[6][3]
Looking at the pathophysiology, arthritis can be degenerative, or it can be post-traumatic following SLAC, SNAC, fractures of the wrist, or brachial plexus injuries.[7] Wrist arthritis can also be due to inflammatory processes such as in rheumatoid arthritis or other autoimmune conditions, congenital (for example secondary to Madelung's deformity), idiopathic, following previous wrist conditions such as Kienbock disease (lunate avascular necrosis) or Preiser disease (avascular necrosis of the scaphoid).[6][8]
Contraindications
There are no specific contraindications for this procedure. Patient refusal to have the procedure as well as an allergic reaction to the implant material can be considered contraindications. In certain circumstances, some patients might benefit from alternative procedures such as full joint replacement rather than wrist fusion. The decision regarding surgical procedure needs to be discussed between the patient and the surgical consultant depending on their age, functional requirements, and the condition affecting the wrist.
Equipment
Wrist arthrodesis instrument set can be provided by a number of medical device companies, and they contain all the necessary instruments and implants for the procedure. The implants are usually made of stainless steel or titanium and come in a variety of shapes and sizes to offer the best surgical outcome to each patient.
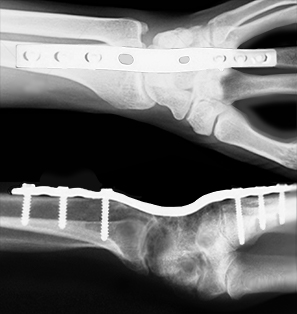
Precontoured plates usually come with a dorsal bend or angulation of 15 degrees to match the contour of the dorsal aspect of the wrist and also to provide maximum functional results. The plates can be bent more during the procedure to accommodate the anatomy of the patient; however, it is advisable to avoid bending the plate at the level of the holes as well as avoid bending the plate multiple times in opposite directions as this will weaken the plate.
The screws used in this procedure can be of various sizes, most commonly of 2.3 mm, 2.7 mm, and 3.5 mm, and they can be used in either locking or non-locking mode depending on which slots of the plate they are inserted in (threaded or nonthreaded).
Bone grafts are sometimes used during the procedure, depending on the surgeon's preference, experience, and patient requirements. The bone graft can either be harvested directly from the patient during the procedure or can be used from a tissue donation bank.
Image intensifiers are commonly used in theatre during the procedure. Because of this, the patient, the operating room staff, as well as the operating team, should wear adequate protective equipment during this procedure.
Tourniquets can be used as well, depending on patient factors as well as surgeon preference. Tourniquets should be applied and inflated at the beginning of the procedure and deflated prior to the closure of the wound to identify any bleeding areas.[9][2]
Other equipment that can be used during this procedure includes a suction device as well as diathermy.
Personnel
The operating team is made of the orthopedic surgeon, the surgical assistant, scrub nurse, and circulating staff. The anesthetic team and operating theatre practitioner are an essential part of the team as well. Most certainly, in all cases, image intensifiers have to be used, so the presence of radiographers is very important. Depending on the available equipment in certain cases, some mini image intensifiers can be manipulated directly by the operating surgeon. Surgical equipment company representatives can sometimes be asked to be present in theatre to help with the use of the equipment.[10][1]
Preparation
Full radiographic assessment should be done before the procedure to assess the extent of arthritis and the residual bone stock. Additional testing may be necessary to identify the underlying pathology such as inflammatory arthritis or degenerative arthritis and also to identify other comorbidities. This procedure is usually done under general anesthesia. The anesthetic team can deliver nerve block prior to the procedure to help with analgesia in the postoperative period, and local anesthetic can be injected at the end of the procedure depending on the complexity and length of the surgery to help with postoperative pain relief. Patients are positioned supine on a standard operating table with the affected arm on a radiolucent arm table attached to the operating table. The patient's shoulder is positioned at the edge of the operating table, and tourniquets are applied at this stage if required. Depending on local hospital guidelines, prophylactic antibiotics are also indicated before the procedure, and the adequate choice of antibiotics should be verified with the local trust or hospital.[2][4]
Technique or Treatment
The following technique is a guide only. This procedure is surgeon dependant, and certain techniques or operating steps may vary depending on surgeon preference or experience.
Once the patient has been anesthetized and positioned on the operating table, the tourniquet is applied (where applicable) and inflated to the desired pressure.
Skin is prepared using antiseptic surgical scrub solution, and sterile drapes are applied in the desired fashion by the operating surgeon.
An approximately 8 cm incision is made longitudinally on the dorsal aspect of the wrist between the third and fourth extensor compartments. Lister's tubercle can be used as a landmark to identify the location of the incision.
Blunt dissection of the soft tissues is performed with care, avoiding damage to the dorsal cutaneous nerve branches of the radial nerve. The extensor policis longus tendon is identified and retracted radially (laterally).
The dorsal radiocarpal and dorsal intercarpal ligaments are split longitudinally, and this will detach the dorsal capsule from the radius at the level of the styloid process.
Denude the articular cartilage from the radiocarpal and intercarpal joint surfaces. Decorticate the dorsal fourth of scaphoid, lunate, capitate, and 3rd carpometacarpal joint. During this stage, bone graft can be harvested from the distal radius or iliac crest and placed into the gaps at the fusion zone. Cancellous allograft can be used instead of autograft. The distal radioulnar joint is usually left undisturbed.
A Kirschner wire (K wire) is then placed through the articular surface of the distal radius, and another wire is placed through the lunate. The wrist is placed in 10 to 15 degrees of dorsiflexion and slight ulnar deviation to optimize handgrip strength. The K wire is then advanced through the radiolunate joint from dorsal to volar. The image intensifier is used to check the position of the lunate and the K wire.
The surgical plate is then applied. A pre-contoured dynamic compression plate or a standard 3.5mm dynamic compression plate can be contoured to be placed on the dorsal aspect of the radius and the third metacarpal bone.
The screws are inserted from the most distal hole situated on the third metacarpus, working towards the most proximal hole located on the distal radius. This step can vary depending on surgeon preference and technique, and some surgeons may choose to insert the first screws into the carpal bones rather than into the metacarpal bones.
Once all screws have been inserted, the wound is washed thoroughly, and the tourniquet is deflated. Sources of bleeding are then coagulated using diathermy.
The wound is then closed, starting with the capsule using absorbable sutures. The extensor retinaculum is repaired, and the extensor pollicis longus tendon is transposed subcutaneously.
The subcutaneous layer is closed with absorbable sutures, and a dressing of preference is applied.
Depending on surgeon preference, a volar brace or a short arm cast can be applied at the end of the surgery, and this is usually removed once the wound has healed.
Postoperatively early finger mobilization is advised, and patients are usually not allowed to weight bear through the affected arm for 8 to 12 weeks following the surgery.[2][3][6][8]
Complications
The risk of complications from this procedure can be as high as 20%. Most complications, however, are minor and include the following:
1. Hematoma formation
1. Nerve injury or dysfunction has been reported in up to 35% of cases with median nerve dysfunction reported in 10% to 25% of cases in the form of carpal tunnel syndrome (positive Phalen test). During this procedure, the highest risk of injury appears to be to the dorsal sensory branch of the ulnar nerve and the sensory branch of the radial nerve.
2. Vascular injury: This should be addressed during the procedure by involving the vascular surgical team.
3. Infection: Certain factors can increase the risk of postoperative infection such as the age of the patient (the elderly population is at higher risk), immunocompromised patients, patients suffering from kidney disease or diabetes, and smoking patients. The rate of infection can be lowered by the use of prophylactic antibiotics preoperatively.[4]
4. Nonunion can be suspected if the patient continues to have wrist pain post-operatively. Radiographs can be taken to investigate this further if suspicions are high. The risk of non-union is low as fusion rates are more than 90%.
5. Tendon injury, most commonly injury to the extensor policis longus tendon, is due to its superficial anatomical location; however, in rare cases, the flexor tendons can also be injured.[8][11]
6.Tendon irritation from the plate or fracture of the metalwork[3][9]
7. Reflex sympathetic dystrophy
8. Neuroma formation
9. Distal radioulnar joint arthritis
10. Iliac crest donor site complications (if used for harvesting bone graft): hematoma, infection, lateral cutaneous femoral nerve injury, prolonged discomfort
11. Hardware complications, such as screw fracture, plate loosening or plate fracture
Clinical Significance
From a functional point of view, following total wrist arthrodesis, patients usually have limited function of their affected wrist. They are unable to produce active flexion or extension of the wrist, and their grip can be reduced. Patients need to be informed of this, particularly if the affected wrist is their dominant one. The limited functionality can have a strong impact on the daily activities performed using the affected hand as well as on the patient's employment, particularly if it involves active use of the hands or wrist, for example, typing or computer work. Hence wrist arthrodesis should be reserved for patients not responding to any other treatment options. In the right patient, the overall satisfaction rate is more than 75% and the grip strength is 75% to 90% of the contralateral side.
Enhancing Healthcare Team Outcomes
Wrist arthrodesis is a complex procedure that can have a significant impact on the affected patient. An informed decision with the operating surgeon is advised before surgery to establish if this is the right procedure for the patient and to discuss any other alternative treatments. Once the patient and the surgical consultant have decided to proceed, a preassessment is advisable. During preassessment, the patient's general health can be assessed by the team, and necessary preoperative tests can be performed, such as blood tests, electrocardiograms, and radiography. Where indicated an anesthetic review could also be done if the patient has a complex past medical history. The surgical ward nurse's role is very important in preparing the patient for theatre on the day of admission as well as monitoring the patient following the procedure. A clear plan should be made for the ward staff to follow once the patient has had their procedure. The anesthetic team plays an essential role in providing both a general anesthetic as well as pain relief (in the form of nerve block), and the theatre staff is a very important part of the surgical team. Once the procedure has finished, the recovery team usually recover the patient until they are awake and ready to be returned to the ward. A physiotherapy assessment postoperatively is an important step in the recovery process of the patient. Clinical follow up with the operating surgeon is advised as the patient will require close monitoring of wound healing, complications, and overall rehabilitation.[1][12]