Continuing Education Activity
Epithelial neoplasms of the ovary account for 60 percent of all ovarian tumors and 40 percent of benign tumors. They are classified as benign, borderline, or malignant tumors. Ovarian cystadenomas are common benign epithelial neoplasms that carry an excellent prognosis. This activity reviews the cause and pathophysiology of ovarian cystadenoma and the role of the interprofessional team in management.
Objectives:
Review the types of ovarian cystadenomas.
Describe the presentation of ovarian cystadenoma.
Summarize the treatment options for ovarian cystadenoma.
Explain modalities to improve care coordination among interprofessional team members in order to improve outcomes for patients affected by ovarian cystadenomas.
Introduction
Epithelial neoplasms of the ovary account for 60% of all ovarian tumors and 40% of benign tumors.[1] They classify as benign, borderline, or malignant tumors. Ovarian cystadenomas are common benign epithelial neoplasms which carry an excellent prognosis. The two most frequent types of cystadenomas are serous and mucinous cystadenomas whereas endometrioid and clear cell cystadenomas are rare. Despite advances in imaging studies, the establishment of a definitive diagnosis of cystadenomas is primarily by histopathological examination of the surgical specimen. This review will focus on ovarian cystadenomas and their histopathological features.
Etiology
Serous Cystadenoma
Serous cystadenomas do not have mutations in either KRAS or BRAF in contrast to serous borderline tumors and low-grade serous carcinoma. Most serous cystadenomas are polyclonal, but monoclonal cystadenomas occur. They develop as a hyperplastic expansion from epithelial inclusions.[2] Serous cystadenomas show DNA copy number changes in the epithelial cells in some cases.[2]
Mucinous Cystadenoma
The association of mucinous cystadenomas with dermoid cysts indicates that some are of germ cell origin and an association with Brenner tumors implies a surface epithelial origin for another subset.[3] KRAS mutations are present in up to 58% of cases.[4]
Endometrioid Cystadenoma
Morphological and molecular genetic studies have implicated endometriotic cysts and endometriosis in the development of endometrioid, clear cell, and seromucinous tumors.
Seromucinous Cystadenoma
According to some authors, seromucinous cystadenomas likely derive from endometriosis.[5]
Epidemiology
Serous Cystadenoma
Benign serous tumors of the ovary represent 16% of all ovarian epithelial neoplasms and account for two-thirds of benign ovarian epithelial tumors and the majority of serous ovarian tumors. They occur in adults of all ages, with reported mean ages differing from 40 to 60 years.[6] They are bilateral in 10 to 20% of the cases.
Mucinous Cystadenoma
Benign mucinous cystadenomas account for 80% of ovarian mucinous tumors. Mucinous cystadenomas of the ovary occur mainly in during the third to sixth decades, but they may also occur in younger women.[7] They are unilateral in 95% of the cases.
Endometrioid Cystadenoma
Endometrioid epithelial tumors account for 2 to 4% of all ovarian tumors. They usually occur in the fourth and fifth decades.[8] Endometrioid tumors often correlate with endometriosis.
Clear Cell Cystadenoma
Clear cell cystadenoma is very rare with very few cases reported in the literature.[9]
Seromucinous Cystadenoma
Seromucinous cystadenoma occurs in adults with a peak in the late reproductive age group.[10]
Histopathology
Serous Cystadenoma
Macroscopic findings:
Serous cystadenoma ranges in size from 1 to more than 30 cm in greatest dimension (mean = 10 cm). They have a smooth outer surface and contain one or more thin-walled cysts filled with clear, watery fluid.[6] Serous cystadenomas are usually unilocular but may be multilocular.
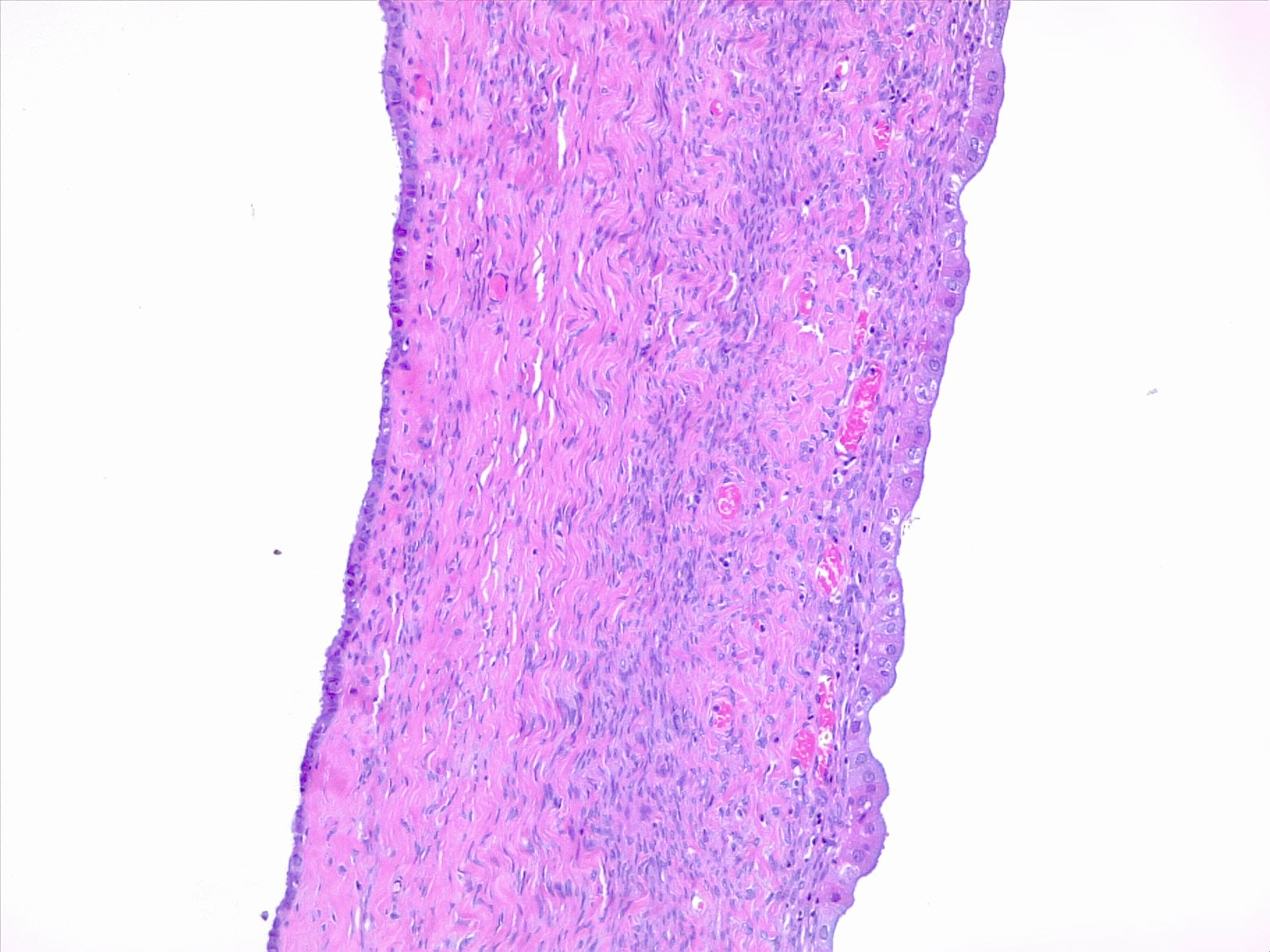
Histopathology:
Serous cystadenomas are composed of cysts and papillae lined by non-stratified or stratified cuboidal to columnar cells resembling fallopian tube epithelium.[6] Usually, there is no or minimal atypia.
Immunohistochemistry:
The immunohistochemical profile of serous cystadenoma is similar to that of normal ovarian surface epithelium and tubal epithelium. In addition to positivity with most commonly used epithelial markers, p63 is positive in most cases.[11]
Mucinous Cystadenoma
Macroscopic findings:
Mucinous cystadenomas have a smooth surface and are usually multilocular and sometimes unilocular. They range in size from a few centimeters to greater than 30 cm; with a mean of 10 cm.
Histopathology:
Mucinous cystadenoma is composed of multiple cysts and glands lined by simple non-stratified mucinous epithelium resembling gastric foveolar-type or intestinal epithelium containing goblet cells and sometimes neuroendocrine cells or Paneth cells. The ovarian stroma may be cellular with areas of stromal luteinization. There are no cytologic atypia and no mitotic figures.
Endometrioid Cystadenoma
Macroscopic findings: the cysts range in size up to 15 cm. The cyst lining is irregular with areas of hemorrhage. The cyst contents are typically dark brown due to old hemorrhage (chocolate cyst).
Histopathology: the rare endometrioid cystadenomas are similar to endometriotic cysts but lack endometrial stroma, hemosiderin-laden macrophages, and a myofibroblastic wall. There are no cytologic atypia and no mitotic figures.
Clear Cell Cystadenoma
Macroscopic findings:
Clear cell cystadenoma ranges in size from 3 to 16 cm. It has a smooth, lobulated external surface.
Histopathology:
Clear cell cystadenoma is composed of glands or cysts lined by cuboidal to flattened cells with clear or eosinophilic cytoplasm embedded in a fibromatous stroma. There are no cytologic atypia and no mitotic figures.
Seromucinous Cystadenoma
Macroscopic findings:
Grossly, seromucinous cystadenomas present as a unilocular cyst with a smooth surface and inner lining. They may contain serous or mucinous fluid.
Histopathology:
Histologically, the cysts are lined by a variable admixture of serous and mucinous cells (endocervical-type) but endometrial and less often transitional or squamous cells may be in evidence. If present, the stroma is bland and fibromatous.
History and Physical
Ovarian cystadenomas ranging in size from 1 to 3 cm are usually incidental findings and reveal themselves during an ultrasound investigation of another gynecologic disorder.[12]
The symptoms and signs associated with large tumors are nonspecific and most commonly include[6]:
- Pelvic pain
- Bloating
- Discomfort
Evaluation
Serum CA-125 Assay
Serum CA-125 assay is a useful tool that helps to distinguish between benign and malignant ovarian masses. The combination of normal findings at serum CA-125 assay, imaging, and clinical findings exclude the possibility of ovarian cancer.[12]
Imaging Studies
Several imaging techniques are useful for the diagnosis of ovarian cystadenomas. They include[13][12]:
- Pelvic ultrasonography (US)
- Computed tomography
- Magnetic resonance imaging
The features that are more suggestive of a benign cystic neoplasm include[12]:
- Unilocularity of cysts
- Minimal septations
- Thin walls
- and absence of papillary projections
The cell type of cystadenomas cannot be determined based on imaging findings.
Ultrasonography:
The initial imaging study recommended in the evaluation of adnexal masses is the pelvic US. The transabdominal US or the endo-vaginal US should is the study of choice to evaluate ovarian masses.[12]
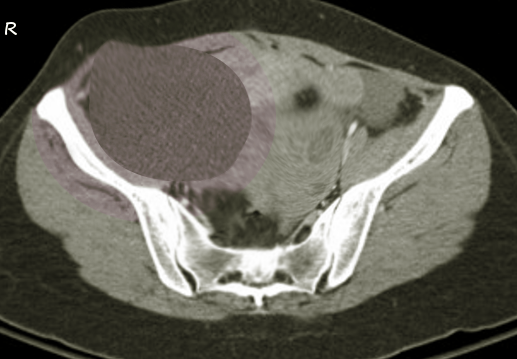
Computed tomography:
Although CT is a useful imaging technique in diagnosing adnexal masses, it is sometimes of limited value.[12]
Magnetic resonance imaging:
Benign epithelial ovarian neoplasms are predominantly cystic, in contrast to malignant epithelial neoplasms which comprise both cystic and solid components. Cystic lesions containing simple fluid have prolonged T1 and T2 relaxation times and very high signal intensity on T2- weighted images.[12]
Histopathology
The definitive diagnosis of ovarian cystadenomas is based on histopathological examination of the surgical specimen.
Treatment / Management
The management of ovarian cystadenomas depends on the following factors[14]
- Symptoms
- Size of the cyst
- Age of the patient
- Medical history
- Menopausal state of the patient
Unilateral salpingo-oophorectomy or ovarian cystectomy is the adequate treatment of ovarian cystadenomas.
Clinical recurrence is uncommon and reflects either incomplete resection or a new primary tumor.
Differential Diagnosis
Histological Differential Diagnosis
Serous Cystadenoma
- Broad ligament cysts
- Hydatid cyst of Morgani
- Mesonephric cysts
- Mesothelial cysts
- Extensive cortical inclusion cysts
- Cystically dilated follicles
- Paratubal cysts
- Hydrosalpinx
- Cystic struma ovarii
- Rete cystadenomas
- Polycystic ovarian disease
Mucinous Cystadenoma
Endometrioid Cystadenoma
Seromucinous Cystadenoma
- Serous cystadenoma
- Mucinous cystadenoma
- Cystic mature teratoma
Prognosis
Serous Cystadenoma
Serous cystadenomas are benign lesions, but they may occasionally recur after cystectomy.[13]
Mucinous Cystadenoma
Mucnous cystadenomas are benign. However, recurrences may be seen in cases treated with cystectomy.[7]
Endometrioid Cystadenoma
Endometrioid cystadenomas are benign lesions which carry an excellent prognosis. Although these tumors do, rarely recur.
Clear Cell Cystadenoma
Clear cell cystadenoma is a benign cyst with an excellent prognosis.
Complications
Cystadenomas of the ovary are benign lesions that rarely recur after incomplete resection.
Rare complications of ovarian cystadenomas include:
- Ovarian torsion
- Cyst rupture
There is a risk of development of pseudomyxoma peritonei if a mucinous cystadenoma ruptures.
Enhancing Healthcare Team Outcomes
Ovarian cystadenomas are benign tumors which carry an excellent prognosis. They are ideally managed by an interprofessional team that consists of gynecologists, radiologists, and pathologists.