[1]
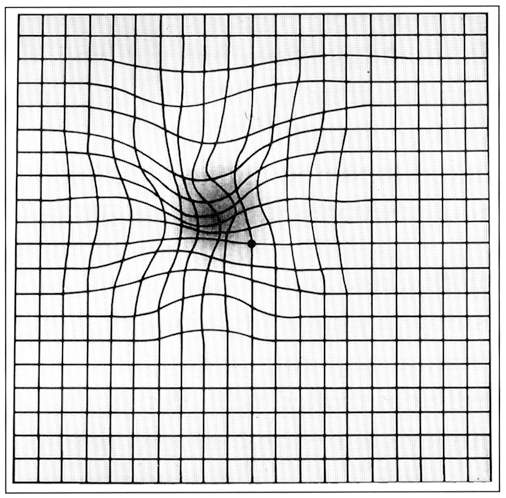
Marmor MF. A brief history of macular grids: from Thomas Reid to Edvard Munch and Marc Amsler. Survey of ophthalmology. 2000 Jan-Feb:44(4):343-53
[PubMed PMID: 10667441]
Level 3 (low-level) evidence
[2]
Abadi RV, Jeffery G, Murphy JS. Awareness and filling-in of the human blind spot: linking psychophysics with retinal topography. Investigative ophthalmology & visual science. 2011 Jan 25:52(1):541-8. doi: 10.1167/iovs.10-5910. Epub 2011 Jan 25
[PubMed PMID: 20847110]
[3]
Jonas JB, Schneider U, Naumann GO. Count and density of human retinal photoreceptors. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 1992:230(6):505-10
[PubMed PMID: 1427131]
[4]
Watanabe A, Arimoto S, Nishi O. Correlation between metamorphopsia and epiretinal membrane optical coherence tomography findings. Ophthalmology. 2009 Sep:116(9):1788-93. doi: 10.1016/j.ophtha.2009.04.046. Epub 2009 Jul 30
[PubMed PMID: 19643494]
[5]
Okamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T. Associations between metamorphopsia and foveal microstructure in patients with epiretinal membrane. Investigative ophthalmology & visual science. 2012 Oct 3:53(11):6770-5. doi: 10.1167/iovs.12-9683. Epub 2012 Oct 3
[PubMed PMID: 22969078]
[6]
Wiecek E, Lashkari K, Dakin SC, Bex P. Novel quantitative assessment of metamorphopsia in maculopathy. Investigative ophthalmology & visual science. 2014 Nov 18:56(1):494-504. doi: 10.1167/iovs.14-15394. Epub 2014 Nov 18
[PubMed PMID: 25406293]
[7]
Marmor MF, Kellner U, Lai TY, Melles RB, Mieler WF, American Academy of Ophthalmology. Recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy (2016 Revision). Ophthalmology. 2016 Jun:123(6):1386-94. doi: 10.1016/j.ophtha.2016.01.058. Epub 2016 Mar 16
[PubMed PMID: 26992838]
[8]
Matsumoto C, Arimura E, Okuyama S, Takada S, Hashimoto S, Shimomura Y. Quantification of metamorphopsia in patients with epiretinal membranes. Investigative ophthalmology & visual science. 2003 Sep:44(9):4012-6
[PubMed PMID: 12939323]
[9]
Midena E, Vujosevic S. Metamorphopsia: An Overlooked Visual Symptom. Ophthalmic research. 2015:55(1):26-36. doi: 10.1159/000441033. Epub 2015 Nov 11
[PubMed PMID: 26554918]
[10]
Alster Y, Bressler NM, Bressler SB, Brimacombe JA, Crompton RM, Duh YJ, Gabel VP, Heier JS, Ip MS, Loewenstein A, Packo KH, Stur M, Toaff T, Preferential Hyperacuity Perimetry Research Group. Preferential Hyperacuity Perimeter (PreView PHP) for detecting choroidal neovascularization study. Ophthalmology. 2005 Oct:112(10):1758-65
[PubMed PMID: 16154198]
[11]
Loewenstein A, Malach R, Goldstein M, Leibovitch I, Barak A, Baruch E, Alster Y, Rafaeli O, Avni I, Yassur Y. Replacing the Amsler grid: a new method for monitoring patients with age-related macular degeneration. Ophthalmology. 2003 May:110(5):966-70
[PubMed PMID: 12750099]
[12]
Wilkinson F, Wilson HR, Habak C. Detection and recognition of radial frequency patterns. Vision research. 1998 Nov:38(22):3555-68
[PubMed PMID: 9893789]
[13]
Pitrelli Vazquez N, Harding SP, Heimann H, Czanner G, Knox PC. Radial shape discrimination testing for new-onset neovascular age-related macular degeneration in at-risk eyes. PloS one. 2018:13(11):e0207342. doi: 10.1371/journal.pone.0207342. Epub 2018 Nov 8
[PubMed PMID: 30408127]
[14]
Wang YZ, He YG, Mitzel G, Zhang S, Bartlett M. Handheld shape discrimination hyperacuity test on a mobile device for remote monitoring of visual function in maculopathy. Investigative ophthalmology & visual science. 2013 Aug 13:54(8):5497-505. doi: 10.1167/iovs.13-12037. Epub 2013 Aug 13
[PubMed PMID: 23860761]
[15]
Jensen OM, Larsen M. Objective assessment of photoreceptor displacement and metamorphopsia: a study of macular holes. Archives of ophthalmology (Chicago, Ill. : 1960). 1998 Oct:116(10):1303-6
[PubMed PMID: 9790627]
[16]
Fink W, Sadun AA. Three-dimensional computer-automated threshold Amsler grid test. Journal of biomedical optics. 2004 Jan-Feb:9(1):149-53
[PubMed PMID: 14715067]
[17]
Cassels NK, Wild JM, Margrain TH, Chong V, Acton JH. The use of microperimetry in assessing visual function in age-related macular degeneration. Survey of ophthalmology. 2018 Jan-Feb:63(1):40-55. doi: 10.1016/j.survophthal.2017.05.007. Epub 2017 Jun 1
[PubMed PMID: 28579549]
Level 3 (low-level) evidence
[18]
Achard OA, Safran AB, Duret FC, Ragama E. Role of the completion phenomenon in the evaluation of Amsler grid results. American journal of ophthalmology. 1995 Sep:120(3):322-9
[PubMed PMID: 7661204]
[19]
Ramachandran VS, Gregory RL. Perceptual filling in of artificially induced scotomas in human vision. Nature. 1991 Apr 25:350(6320):699-702
[PubMed PMID: 2023631]
[20]
Schuchard RA. Validity and interpretation of Amsler grid reports. Archives of ophthalmology (Chicago, Ill. : 1960). 1993 Jun:111(6):776-80
[PubMed PMID: 8512478]
[21]
Wall M, Sadun AA. Threshold Amsler grid testing. Cross-polarizing lenses enhance yield. Archives of ophthalmology (Chicago, Ill. : 1960). 1986 Apr:104(4):520-3
[PubMed PMID: 3954654]
[22]
Slavin ML. The use of the red Amsler grid and red-green lenses in detecting spurious paracentral visual field defects. American journal of ophthalmology. 1987 Mar 15:103(3 Pt 1):338-9
[PubMed PMID: 3826248]
[23]
Shinoda K, Ishida S, Kawashima S, Matsuzaki T, Yamada K, Katsura H. A new method for quantification of metamorphopsia in patients with epiretinal membrane. Japanese journal of ophthalmology. 2000 Jul-Aug:44(4):424-7
[PubMed PMID: 10974300]
[24]
Bouwens MD, Van Meurs JC. Sine Amsler Charts: a new method for the follow-up of metamorphopsia in patients undergoing macular pucker surgery. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2003 Feb:241(2):89-93
[PubMed PMID: 12605261]
[25]
Ugarte M, Shunmugam M, Laidlaw DA, Williamson TH. Morphision: a method for subjective evaluation of metamorphopsia in patients with unilateral macular pathology (i.e., full thickness macular hole and epiretinal membrane). Indian journal of ophthalmology. 2013 Nov:61(11):653-8. doi: 10.4103/0301-4738.117804. Epub
[PubMed PMID: 24008785]