Introduction
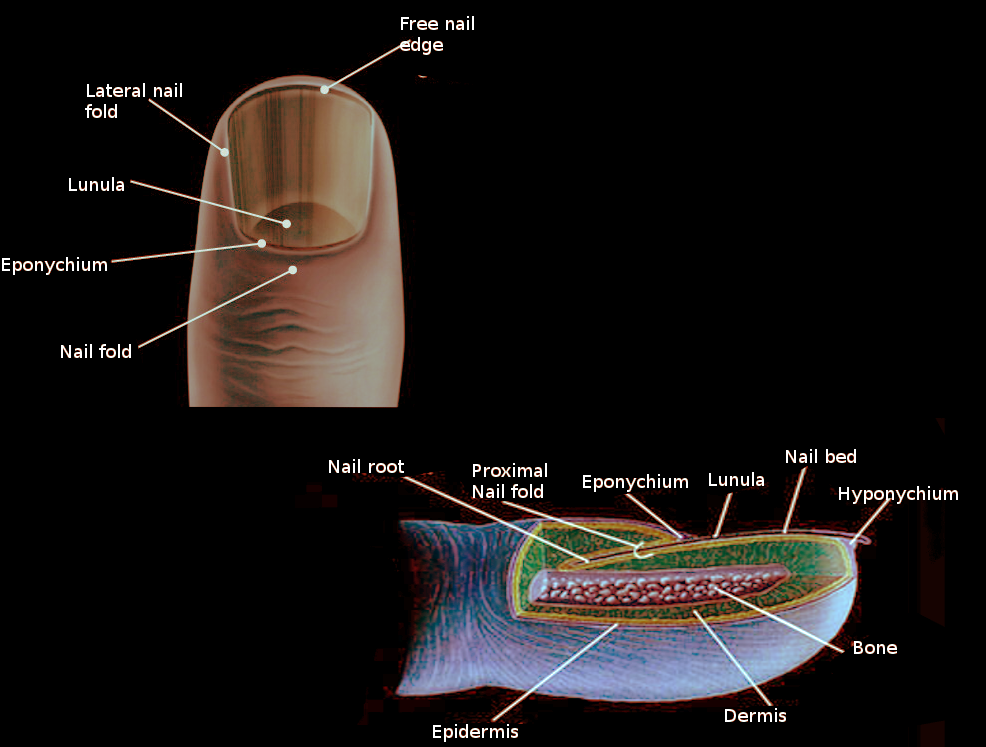
Our nails are an essential sensory organ. The tips of the digits are composed of almost all tissues components found elsewhere in the human body: skin, joint, bone, synovial membrane, ligaments, tendons, arteries, veins, lymphatic vessels, tendon sheaths, nerves, and specialized nervous end organs.[1] The nail plate is made up of laminated keratinized structure on the nail matrix, nail bed with the distal onychodermal band and the hyponychium at the first edge. Some toenails can have a lunula at the distal part of the matrix, characterized by the half-moon shape. The nail plate is embedded in the proximal and lateral folds. The cuticle adheres to the proximal nail fold. The nails possess both complex vascular and nerve networks to ensure adequate blood supply and sensory innervation. All these structures listed function together to provide healthy, growing nails.[2]
Structure and Function
The nail unit consists of the nail plate and periungual tissues. Each unit is listed below.
Nail Matrix
The nail matrix is the structure that produces the nail plate, the visible part of the nail that is hard and translucent. The nail matrix is about halfway between the proximal nail fold and the distal interphalangeal joint. It is divided up into the proximal and distal nail matrix. The distal nail matrix is visible and is called the lunula. The lunula looks like a white half-circular flat structure at the proximal portion of the nail plate. There are three portions of the nail matrix that correspond to the three-layer structure of the nail plate. The dorsal aspect of the nail matrix corresponds to the proximal nail fold and the upper nail plate. The intermediate aspect of the nail matrix, the classical nail matrix, corresponds to the intermediate nail plate. The ventral aspect of the nail matrix corresponds to the nail bed and the lower nail plate. The proximal nail matrix produces most of the nail plate, and for that reason, it is important not to disrupt its structure when performing nail surgery.[2][3][4]
Nail Bed
The nail bed is epithelium that provides firm attachment to the dermis. The nail plate makes up only one-third of the length of the nail unit, and only the distal portion is visible, as most remains hidden underneath the proximal nail fold. It extends from the distal margins of the lunula to the hyponychium.[2]
Nail Plate
The nail plate is a modified stratum corneum that serves as a laminated keratinized structure that protects the nail bed and matrix. It is considered a bilaminar structure that provides its thickness and density as it grows distally. There are both longitudinal and transverse axes in the nail plate. These axes provide strong attachments. In the great toe, the lateral margins of the matrix and nail extend almost halfway around the terminal phalanx, which provides additional strength.[5]
Grossly, the upper surface of the nail can be smooth with some rigidity depending on the age of the patient. In childhood, there are partial oblique ridges called herringbone or chevron pattern. With age, longitudinal ridges become more common.[2]
The nail plate has several layers produced by different parts of the nail matrix. The apical matrix produces the most superficial layers of the nail plate. The middle matrix produces the middle nail plate, and the distal matrix is for the deep layers.[6]
The nail plate is firmly attached to an area known as the nail bed. When they are firmly attached, the nail should be a pink color. The nail bed has a thin epithelium. The distal aspect of the nail plate is called the nail isthmus and is where the granular layer of the nail plate appears and marks the transition to the hyponychium.[6]
The hyponychium is where the nail plate and nail bed separate. It is the epithelium equivalent of the skin contains granular and thickens cornified layers. It serves as a barrier from outside material from entering between the nail bed and plate, which is why it exhibits strong keratinization.[6]
Nail Folds
There are three total nail folds, two laterally, and one proximally. These function to direct the nail growth in the correct direction and shape.[1] The lateral nail folds provide the lateral cutaneous margins of the nails. These folds are prominent in the toenails. If these folds become weakened or compromised, the risk of infectious disease and onycholysis increases. There can be pathologic ingrowing, commonly seen in the big toe, can result from trauma to the area. The proximal nail fold adheres to the dorsal aspect of the nail plate and combines with the nail plate to provide protection. The keratin layer of the proximal nail fold forms the cuticle. This structure serves as a seal against chemicals that might disrupt the nail matrix function. Compromise of this function can result in a transverse groove due to inflammation in the nail matrix. These are known as Beau lines.[2]
Growth Rate
Growth measurement is in the longitudinal axis from a defined reference point to the free edges. Nails do grow continuously. However, both age and poor circulation can decrease growth rate. Toenails do grow slower than fingernails. The time for a toenail to undergo full replacement is about 12 to 18 months. The toenails grow about 1mm in a month. Several systemic diseases, for example, scarlet fever, can cause a reduction in the rate of matrix-cell division, causing thinning of the nail plate. Typically, toenails in women are about 1.4 mm thick and 1.65 mm thick in men.[7]
Normal Nail Histology
The dorsum of the proximal nail fold is similar to the skin of the digits. The ventral aspect is thin and flat epidermis. Between them, there is thick stratum corneum making the nail cuticle. The nail matrix has multilayered epithelium as it serves as the production of the nail plate. It is the sole site of hard keratin synthesis. The nail bed epithelium is thin and lacking a stratum granulosum layer. The stratum granulosum layer reappears in the hyponychium, the distal thickened part of the nail bed. The distal matrix is composed of loose and edematous tissue. The dermis contains multiple glomus bodies, which represent arteriovenous anastomosis. The nail plate itself is composed of multiple paralleled layers of keratinized, flat well-differentiated cells called onychocytes. These cells are firmly adherent and do not desquamate.[3]
Embryology
The beginning stages of nail growth becomes evident around eight weeks of gestational age. The nail primordium begins as a transverse ridge on the distal dorsal surface of the digit. As the week progress, the ridge extends proximally and becomes invaginated beneath the developing proximal nail fold. The outline is evident by 16 weeks gestational age. The matrix is a band of the highly proliferative epithelium in which production of the proximal nail plate occurs. There is less proliferation activity distally to create a convex curve of the plate. By month 5, the nail plate has completely covered the nail bed.[1][8]
Blood Supply and Lymphatics
The nail unit is relatively vascular. It receives vascular supply from both the volar and dorsal proper digital arteries. The merge together around the distal interphalangeal joint. They give small branching vessels called the arcades that provide the proximal nail fold, matrix, and nail bed. Between the arcades are small arteries running parallel along the nail bed longitudinally. Because of the orientation of these vessels, it is essential if possible, to biopsy longitudinally.[6]
The digit gets its supply by two dorsolateral and two ventrolateral arteries that lack an internal elastic lamina. They have a tortuous route and morphology that helps withstand the various movements and flexions without damage. Between these branches, numerous communications provide the digit with a blood supply in multiple directions, which ensures continued blood flow in the events of trauma and any hand positioning that decreases delivery from ventral vessels.[9]
The proximal nail folds have dermal capillaries that form hairpin loops. Dermoscopy examination of the proximal nail bed can help asses for the microvascular status of the proximal nail bed. Patients with autoimmune diseases such as lupus erythematous can demonstrate dilated, tortuous capillaries with a typical density of the proximal nail fold. Patients with scleroderma or dermatomyositis can present with decreased capillary density with avascular areas alternating with dilated capillaries in the proximal nail fold.[9]
A unique feature of the nail unit is a vascular unit called the glomus bodies. These function as organs for thermoregulation. They are afferent and efferent vessels with vascular lumina and innervated glomus cells with contractile function. These units are through to be the origin of a type of hamartoma that can present on the nails called glomus tumors. Glomus tumors typically show as painful lesions on the nails.[6]
Nerves
The nail unit of the lower extremity, the nails are innervated by the plantar digital nerves. These digital nerves are branches from the medial and lateral plantar nerve. The medial plantar nerve has three branches which provide the sensation for the great toe, second, third, and fourth toe. The lateral plantar nerve communicates with a distal branch of the medial plantar nerve to provide sensation for the fourth and fifth toes. Similar to the vascular supply of the digit, there are two dorsal and two ventral branches with overlapping sensory areas. There are several nerve fibers in the fingers due to their essential role of sensory perception. There are numerous type 1 fibers that transmit pain, Meissner, and Pacinian bodies that carry touch and temperature sensing fibers.[1]
Surgical Considerations
A nail biopsy can provide additional concrete information when it comes to diagnoses of disease. But it is far more complicated compared to skin biopsies. A punch biopsy should be performed to get a full biopsy of the nail bed, the matrix, and the folds. However, longitudinal nail biopsies provide the most accurate information. A straight incision is possible through the proximal nail fold to the hyponychium and a second incision parallel to that providing a long rectangular shaped piece of tissue contain all nail components.[6]
Clinical Significance
The nail can be the first clue to different types of cutaneous or systemic diseases. The nail examination is underutilized and should be a part of every annual full body skin check. Several different types of conditions can involve the nail. Below are the names and findings of several nail diseases:
- Subungual Melanoma
- Melanoma arises from the nail apparatus consisted of about 0.18 to 7% of all cutaneous melanomas. Its incidence is higher in dark-skinned and Asian population. Most commonly it presents in the thumb or great toenail, possibly due to the increased density of nail matric in these digits. It typically arises from the nail matrix and less commonly in the nail bed or folds. It presents with a longitudinal melanonychia or nail dystrophy. Longitudinal melanonychia can also present from benign hyperplasia of melanocytes. It is essential to follow the ABCDE (asymmetry, border, color, diameter, evolution) rules when considering subungual melanoma; however, a biopsy is necessary for diagnosis confirmation. Hutchinson sign is when the nail melanoma extends laterally onto the periungual tissue.[10]
-
Onychomycosis
-
Onychomycosis, typically caused by a dermatophyte, is a fungal infection in the nail unit. Less commonly, it can result from yeasts. Onychomycosis of the toenail is more prevalent than the fingernails. Asymptomatic, dry hyperkeratotic tinea pedis is a frequent precursor. Organisms can be present in hotels, public showers, pool decks, etc. Over time, the dermatophytes causing the tinea pedis can penetrate the nail bed and cause tinea unguium, another name for onychomycosis. It causes damage to the nail matrix leading to the hyperkeratotic and thickened nail bed. It can be differentiated from dystrophy toenails by longitudinal striae whereas transverse onycholysis is consistent with nail dystrophy. Systemic antifungals are the most effective treatment.
-
Periungual Warts
- Periungal warts commonly seen in children and young adults. Typically located around the nail, leaving the nail plate unaffected. It can present as firm, keratotic papules with ranging sizes. Clinical presentation is a paronychia0lik inflammatory reaction with distal wart emerging under the cuticle.
-
Trachyonychia
-
Trachyonychia is a term used for rough nails covered with scale and extensive superficial longitudinal ridges. Nails become brittle and can split at the free edge. It can be associated with one nail or all finger and toenails (twenty-nail dystrophy syndrome) It has been seen commonly with lichen planus, psoriasis and alopecia areata.
-
Onycholysis
- Onychosis is the painless separation of the nail from the nail bed. It is fairly common. Separation typically begins at the distal groove and progresses proximally in an irregular pattern. The nonadherent portion of the nail is white. Causes include psoriasis, trauma, infections such as Pseudomonas or Candida, internal medication, photochemotherapy, contact with irritants, or prolonged allergic contact dermatitis. It can also be associated with thyroid disease. It can be treated by removing the separated nail and keeping the area dry to decrease the risk of infection. Any form of manipulation to the area should be discouraged.[11]
-
Ingrown Toenails
-
Ingrown toenails are most common in the large toe. The nail begins to grow laterally and pierce the lateral nail folds, acting as a foreign body. It typically presents as swelling and pain and can progress to purulent or edematous granulation tissue. It can occur from continuous lateral pressure of ill-fitting shoes, improper or excess trimming of lateral nail plates or trauma. Treatment is determined by if the area exhibit inflammation or not. Typically the area can be cut under local anesthesia if inflamed but otherwise absorbent cotton can provide immediate relief of pain once placed to separate the distal top and lateral edges of the toenail from the soft tissue.