Introduction
The gracilis is a spiral unipennate muscle in the medial thigh compartment. It is innervated by the anterior branch of the obturator nerve. It receives its vascular supply from the medial circumflex, superficial femoral, deep femoral, descending genicular, and the anterior branch of the obturator artery.[1][2] The gracilis assists with hip adduction, knee flexion, and internal knee rotation. It is the most superficial muscle of the medial thigh. It may suffer strain injury when patients have an adductor strain, a common injury among soccer, hockey, football, and basketball athletes.[3][4] Surgeons commonly use the gracilis for breast, craniofacial, lower limb, perineal, anterior cruciate ligament (ACL) reconstruction, and other reconstructive surgeries.[5][6]
Structure and Function
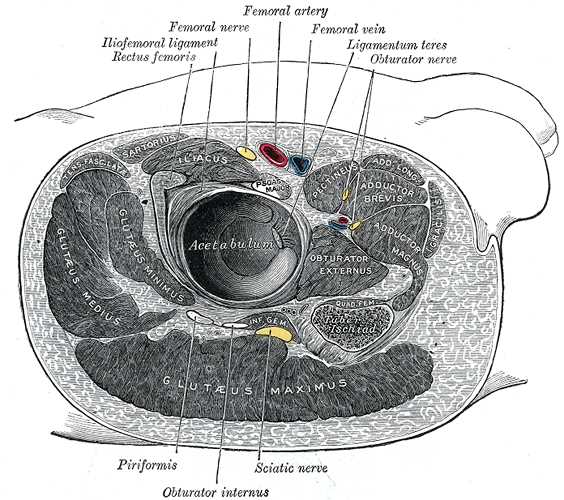
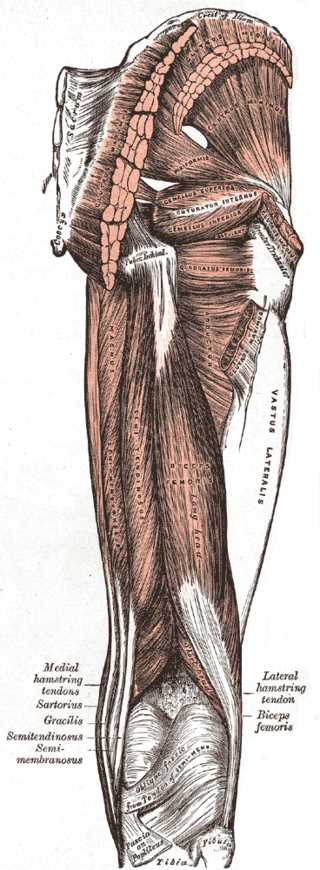
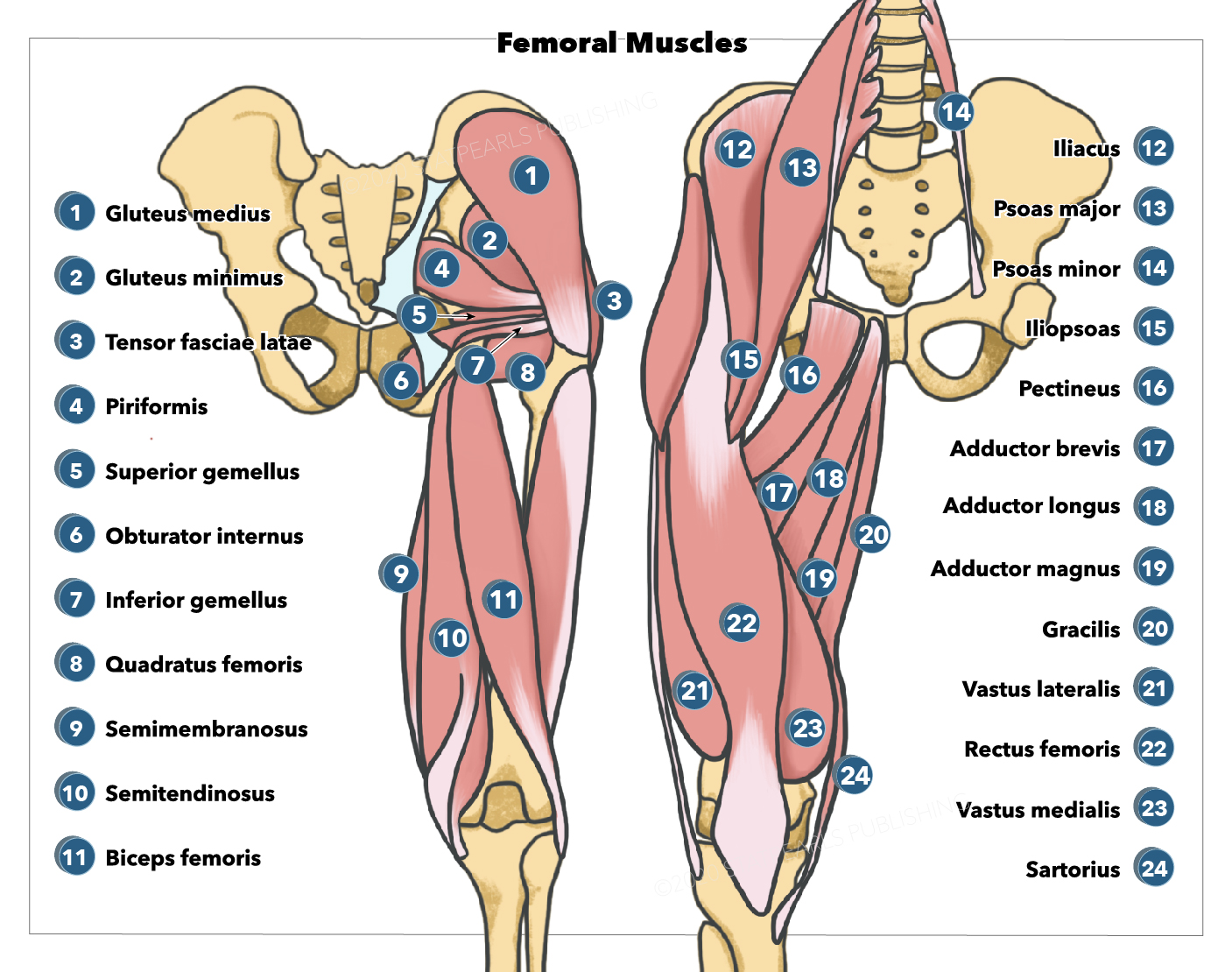
The gracilis is a long, thin muscle located in the medial compartment of the thigh. It originates from the medial aspect of the ischiopubic ramus. It is also related (along with the adductor brevis muscle) to the inferior pubic ligament, a band connecting the inferior parts of the pubic rami.[7] Distally, the gracilis joins with the sartorius and semitendinosus muscle tendons to form the pes anserinus, which inserts on the superior medial tibia, medial to the tibial tuberosity.
The muscle fiber bundles of the gracilis have a spiral arrangement, which inserts onto the anterior aspect of the gracilis tendon obliquely, making it a spiral unipennate muscle.[1][4] There are 5 to 7 muscle fiber bundle compartments in the gracilis muscle, with nerve branches coursing along each compartment, indicating that each compartment may have independent neuromuscular compartment function.
Crossing both the hip and knee joints, the gracilis muscle performs hip adduction, hip flexion, hip internal rotation, knee flexion, and internal knee rotation.[3][8][9]
Embryology
The gracilis muscle derives from the mesoderm and can be found in the fetus from the eighteenth week of gestation. In a 22.5 mm crown-rump length embryo, the femur, and associated adductor thigh muscles, are appreciable.[10] The gracilis is fully complete by the twenty-eighth week of gestation.
Blood Supply and Lymphatics
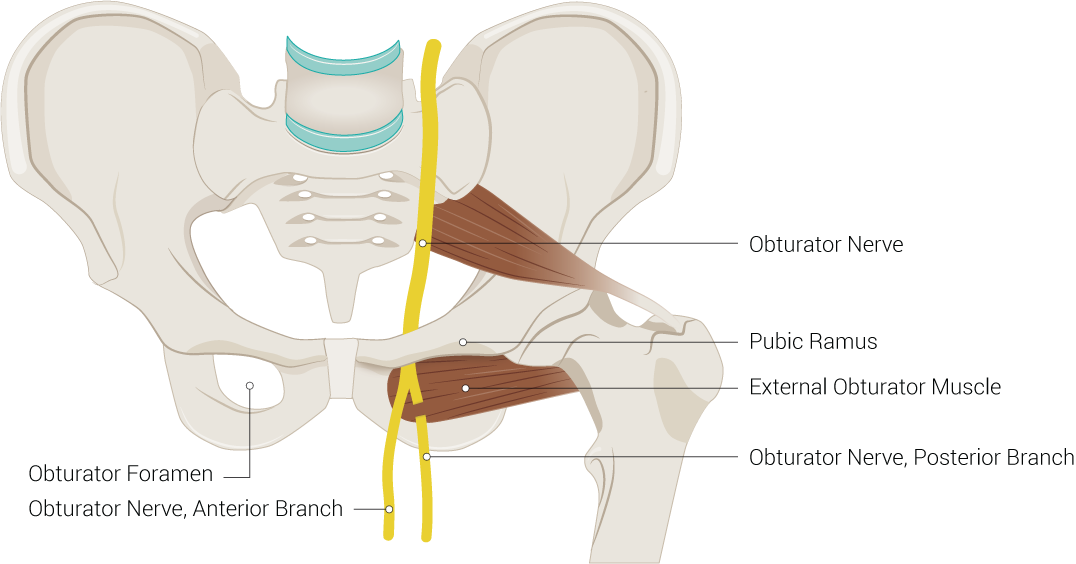
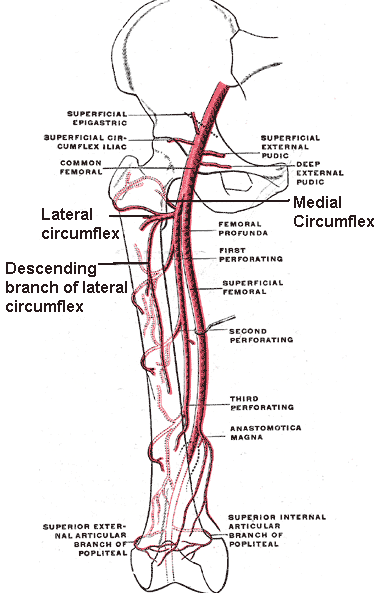
The gracilis obtains its vascular supply from the medial circumflex femoral artery, superficial femoral artery, deep femoral artery, descending genicular artery, and the anterior branch of the obturator artery. The anterior division of the internal iliac artery, the inferior epigastric artery, or the external iliac artery can give off the obturator artery, which traverses the ilioischial line, enters the obturator foramen, and splits into the anterior and posterior branch of the obturator nerve as it exits the obturator foramen.[3][5] The external iliac artery turns into the common femoral artery as it passes under the inguinal ligament at the mid-inguinal point. The common femoral artery splits into the superficial and deep femoral arteries. The deep femoral artery then gives rise to the medial and lateral circumflex femoral arteries. The superficial femoral artery gives rise to the descending genicular artery near its terminal end.[11][12]
The terms major and minor pedicles are utilized when describing the neurovascular supply of the gracilis muscle. Major pedicles are areas where one artery (the major artery), two veins (venae comitantes), and the anterior branch of the obturator nerve enter the muscle, while minor pedicles are where one artery and two vena comitantes enter the muscle. The medial circumflex femoral artery, deep femoral artery, and the anterior branch of the obturator artery are the arteries that may be present in major pedicles.[10] Patients usually have one major pedicle going into the proximal anterior aspect of the gracilis; some patients may have two major pedicles. Once the major pedicle artery enters the gracilis, it assumes one of three intramuscular distribution patterns, known as types.
- Type I (Dichotomous): The major artery splits into a proximal and distal branch. The proximal branch runs proximally from the pedicle insertion and branches to supply the proximal gracilis. The distal branch progresses distally in the muscle and branches into two branches, each of which branches again into two additional branches.
- Type II (Array): The major artery enters the gracilis and runs diagonally (slightly towards the distal end) in an anterior-to-posterior direction, from which arrays of ascending and descending branches arise to supply the gracilis.
- Type III (Dual Pedicle): In patients with two major pedicles, both pedicles are present on the proximal anterior aspect of the gracilis. However, they do not have any connections between the major arteries or their branches. The major artery of one pedicle and its branches supply the proximal gracilis, and the major artery of the other pedicle and its branches supply the distal gracilis.
The major artery typically supplies the posterior (deep) portion of the muscle, while the other branches supply the anterior (superficial) portions of the gracilis.
The minor pedicle artery can be the superior femoral artery, the deep femoral artery, or the descending genicular artery. Most of the minor pedicles are distal to the major pedicle. The artery of minor pedicles enters the gracilis anteriorly and divides into ascending and descending branches within the muscle. The ascending and descending branches form anastomoses with adjacent vessels, especially along the anterior aspect of the gracilis.
In the major and minor pedicles, each artery has two venae comitantes running alongside them, with one vein distal and anterior to the artery and one vein proximal and posterior to the artery. Each vein has a distinct draining region. Veins only anastomose with minor pedicle arteries outside the muscle, not within the muscle. When patients have two major pedicles, each major artery only has one vena comitans.[5][3]
Nerves
The obturator nerve originates from the L2 to L4 spinal nerve roots. It traverses along the iliopectineal line, enters the obturator canal, exits from the obturator forearm, and splits into the anterior and posterior branches. The gracilis muscle receives innervation from the anterior branch of the obturator nerve. The major pedicles contain the anterior branch of the obturator nerve. Typically, the anterior branch of the obturator nerve forms two divisions, one of which is superficial to the pedicle and one deep to the pedicle. From there, the nerve divides into two to six descending branches, which distally traverse the length of the muscle.
From the main branch of the obturator nerve that entered the muscle, one or two branches go proximally and supply the proximal gracilis. There are variations in the paths of the vasculature (arteries and vena comitantes) and the nerves; they usually follow each other intramuscularly, but not always.[2][3]
Physiologic Variants
Females are more prone to ACL injury due to different knee muscle morphology.[13] This proclivity was calculated from the muscular relationship between extensor muscles and knee flexors.
The muscular volume of the medial vastus is greater in females, while the volume of the gracilis muscle (and the sartorius muscle) is smaller when compared to males.[14]
Surgical Considerations
Surgeons may use the gracilis tendon in reconstructive surgery of the anterior cruciate ligament (ACL) of the knee. The gracilis muscle also has surgical use in patients who have lost the muscular function of their digits, patients with facial palsy, or brachial plexus injuries. Since the gracilis can be split into independent neuromuscular compartments, utilizing a muscle transfer technique that applies more than one functioning compartment can achieve good functional outcomes. Additionally, the gracilis muscle may be used as a free tissue flap because it has predictable neurovascular pedicles, which can be used to repair large pelvic and perineal wounds, temporoparietal defects, and anovaginal and rectovaginal fistulas.[4][3]
The gracilis muscle is part of the medial hamstring group, which provides rotational, valgus, and anterior translation stability to the knee. When the gracilis is harvested to use as a graft for surgeries such as ulnar collateral ligament reconstruction, external rotation of the knee is increased slightly, with no difference seen in anterior translation. When harvesting only the semitendinosus muscle, there is an increase in external rotation and anterior translation of the knee. When harvesting both the gracilis muscle and the semitendinosus for ACL reconstruction, a significant increase in external rotation and anterior translation occurs.
Additionally, when knees were ACL-deficient, and the semitendinosus and gracilis were both harvested, a significant increase in external rotation and anterior translation occurred, indicating the importance of the medial hamstring group in stabilizing the knee in patients who are ACL-deficient and further providing evidence for pre-ACL reconstruction hamstring strengthening. In patients who are high-performing athletes, altering knee dynamics may be detrimental to performance. Therefore, evaluating sport-specific demands in high-performing athletes when determining what ACL reconstruction graft to use is recommended. Similar consideration is advised when using a gracilis harvesting procedure to repair conditions such as ulnar collateral ligament rupture.[8]
Open or arthroscopic techniques can be utilized when harvesting the gracilis and semitendinosus tendons for a hamstring autograft ACL reconstruction. Awareness of structures associated with those tendons is important when utilizing those techniques. The gracilis and semitendinosus tendons connect via intertendinous bands. They are each surrounded by a dense fascia that connects them to surrounding soft tissue, and each tendon may have accessory bands that connect them to each other or structures such as the sartorius, gastrocnemius, or crural fascia. A smooth tendon harvest requires the dissection of any intertendinous or accessory bands and the dense fascia surrounding each tendon.[15][16][17][1]
When selecting what tendon to use for ligament reconstruction surgery, biomechanical properties such as elastic modulus (ability to resist elastic deformation) should be accounted for to see if the graft tissue can simulate the function of the original tissue it is replacing. The gracilis and semitendinosus tendons have a statistically significant higher elastic modulus when compared to the patellar tendon, quadriceps tendon, and iliotibial band (ITB). Additionally, there is a statistically significant lower strain in the gracilis and semitendinosus tendons compared to the patellar tendon and ITB. Therefore, the hamstring tendons demonstrate better strength as ACL reconstruction grafts when compared to the patellar tendon, quadriceps tendon, and ITB grafts.
However, graft success is a multifactorial issue. Pre-operative status and rehabilitation, surgical technique, and post-operative rehabilitation play a role in graft success or failure and should be accounted for before selecting a graft for ACL reconstruction. Additionally, patient goals merit consideration when determining which graft is most appropriate.[18]
Clinical Significance
Soccer, hockey, football, basketball, tennis, baseball, figure skating, baseball, and softball are all sports with a high incidence of hip adductor muscle strains. This is especially true in men’s collegiate soccer, where 46.5% of all hip and groin injuries are adductor muscle strains.[6] Since it is a common injury, and the gracilis muscle is part of the adductor group, it is vital for athletes to incorporate adductor muscle strengthening into their training and to correct conditions such as over-pronation, which may predispose athletes to adductor strains.[9]
When patients present with atrophy of the gracilis muscle and atrophy of the adductor longus and adductor brevis, the inclusion of possible injury to the anterior branch of the obturator nerve should be included in the differential diagnosis; etiologies may include nerve impingement caused by a ganglionic cyst that emerges from the transverse acetabular ligament, neoplasm, hematoma, or iatrogenic nerve injury caused by hip surgeries such as total hip replacement.[2]
When patients have pain along the distal portion of their gracilis tendon, where it becomes the pes anserinus, there should be a high suspicion of pes anserinus bursitis, especially if there is edema present. Pes anserinus bursitis is commonly seen in patients with obesity or osteoarthritis or who are female.[19] The typical presentation of pes anserinus bursitis as medial knee pain, which may be worse when ascending stairs, can mimic internal knee joint injuries, such as a meniscal tear. Dedicated imaging, such as MRI, can ensure the correct diagnosis and avoid unnecessary knee arthroscopy.[20] Pes anserinus bursitis is typically managed with conservative measures such as NSAIDs and physiotherapy; corticosteroid injections can also benefit.[21]