Continuing Education Activity
Acquired digital fibrokeratoma (ADFK) is a rare, benign fibrous tumor that usually occurs in adults as a solitary lesion on fingers and toes. Since ADFK shares clinical and histologic features with other cutaneous conditions, careful examination is necessary for proper diagnosis and management. This activity reviews the evaluation and treatment of ADFK and highlights the role of the interprofessional team in the care of patients with this condition.
Objectives:
- Differentiate acquired digital fibrokeratoma from other cutaneous lesions that may mimic its appearance through thorough clinical assessment and histopathological examination.
- Implement evidence-based treatment strategies for acquired digital fibrokeratoma, including selecting surgical excision as the primary intervention, considering patient factors and lesion characteristics.
- Select and utilize appropriate imaging modalities, such as dermoscopy or imaging studies, to aid in diagnosing and assessing acquired digital fibrokeratoma, particularly in challenging cases.
- Collaborate with dermatologists, plastic surgeons, and other healthcare professionals to ensure multidisciplinary coordination and comprehensive care for patients with acquired digital fibrokeratoma
Introduction
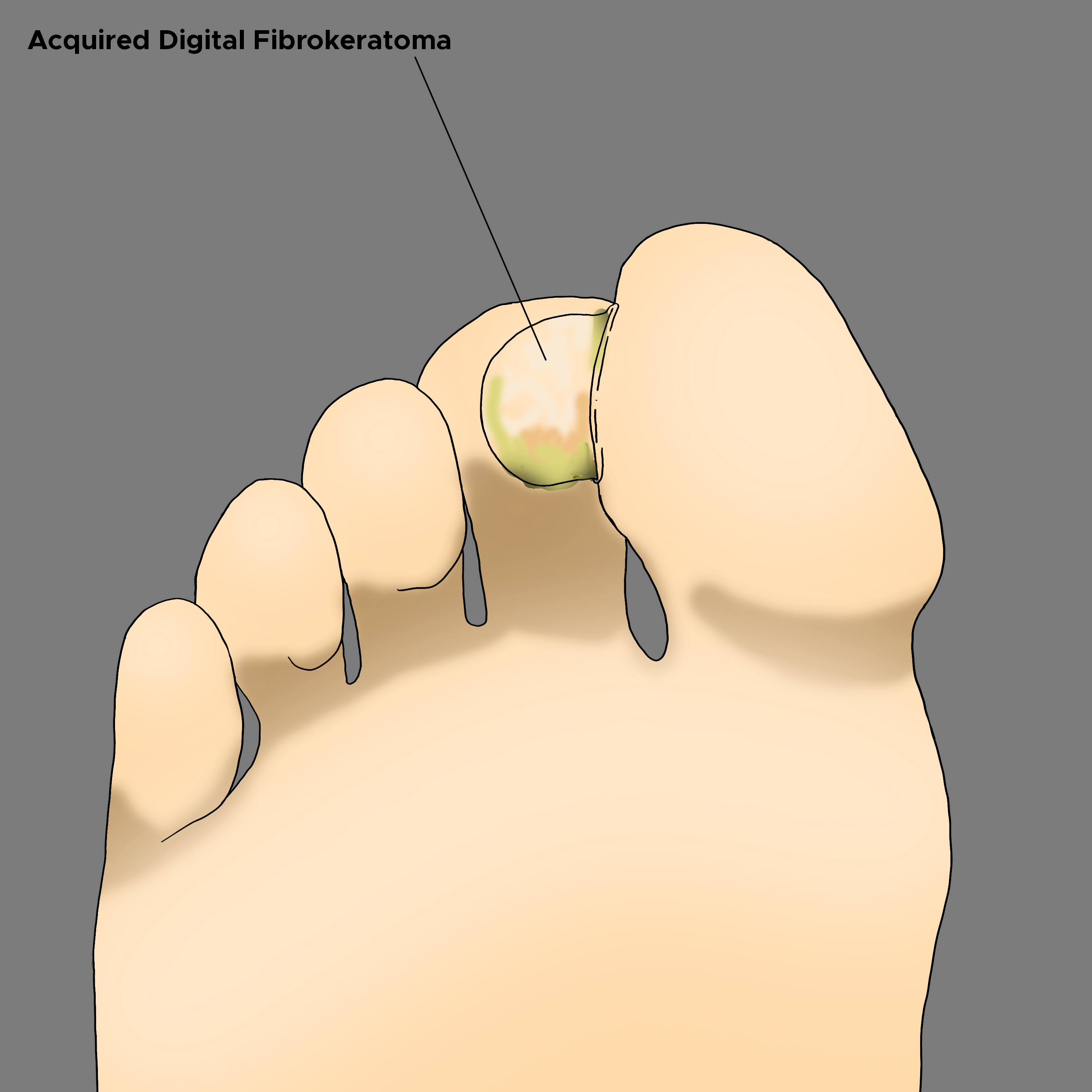
Acquired digital fibrokeratoma (ADFK) is a relatively rare and benign fibrous tumor.[1][2] The condition was first reported in 1968 by Bart et al, who noted multiple cases of this uncommon tumor on the fingers.[3] While ADFK typically occurs on the fingers, it can also occur on other acral surfaces, such as the heel, toes, palms, and soles. Therefore, it is often referred to as acral fibrokeratoma.[4][5][6]
Clinically, ADFK presents as a small solitary papule surrounded by a characteristic hyperkeratotic collarette. The differential diagnosis usually includes a rudimentary supernumerary digit and the common wart when diagnosing this condition.[7][8] The treatment of choice is surgical tumor excision, as ADFK does not show spontaneous regression.
Etiology
The etiology of acquired digital fibrokeratoma remains unclear though it has been proposed that trauma or chronic irritation may be associated with its development, especially in the acral areas.[9] Specifically, repetitive trauma to a single site is believed to contribute to ADFK. This explains why the acral regions, predisposed to significant trauma on a day-to-day basis, are more commonly affected areas.[10]
Histopathologic studies have revealed the presence of densely packed collagen fibers in affected areas, suggesting that collagen deposition by new fibroblasts may play a role in the etiology.[10]
However, most patients do not report a known history of trauma to the site of ADFK.[10] As a result, there are 2 other prevailing theories for the etiology of this condition.
The first theory proposes an infectious origin as a possible cause. There have been reports of 2 cases where ADFK developed after a staphylococcal infection, particularly caused by Staphylococcus aureus.[11][12] This may suggest that a proliferative fibroblast response triggered by an infection may lead to the same histopathologic findings associated with trauma in the development of ADFK.
Another theory suggests that the condition may result from a proliferative benign neoplasm. Evidence of factor XIIIa staining in the dermis, much like dermatofibroma, supports this theory.[10] Interestingly, there has been a documented case where ADFK occurred concurrently with gingival overgrowth following cyclosporin treatment.[13]
Epidemiology
Acquired digital fibrokeratoma is a rarely reported tumor, and its actual incidence is still unknown. Most publications on this condition consist of individual case reports, with authors often highlighting the lesions’ unusual size, location, or association with other conditions. However, a few case series have been published, with the most significant case including 50 patients.[1]
Documented cases of ADFK appear in patients of all racial backgrounds, and reports exist in German, Polish, Japanese, French, and Indian literature.[7] Males appear to be more affected than females, and the age range for ADFK is reported to be between 12 to 70 years, with a higher likelihood of occurrence in middle-aged adults.[7]
Pathophysiology
The pathophysiology of ADFK remains unclear. Histological examination of the tumor reveals denser fibers than normal skin and contains more fibroblasts and coarser elastic fibers. Therefore, the presumption is that ADFK results from the neoformation of collagen by fibroblasts.[5][7]
Nemeth and Penneys reported that factor Xllla, present in fibrovascular tumors, is also found in ADFK.[14] Furthermore, collagen synthesis may undergo regulation by factor Xllla-positive dermal dendrocytes, which are increased in ADFK. This suggests that factor Xllla may be predominant in the fibroblastic reaction associated with ADFK.[10]
In cases of post-staphylococcal ADFK, it has been demonstrated that Staphylococcus aureus enterotoxin B can enhance fibroblast migration.[15]
Histopathology
Excisional biopsy is considered the gold standard for diagnosing acquired digital fibrokeratoma. Histopathological examination of the biopsy specimen typically reveals a very hyperkeratotic and acanthotic epidermis, accompanied by thick collagen bundles oriented vertically in the dermis.
The dermal core of an ADFK presents 1 of 3 histological variants, as characterized by Kint et al.[1] Type I is the most common variant, which presents as a dome-shaped lesion and consists of a dermal core of thick, densely packed collagen bundles with fine elastic fibers.[1] Type II is a tall, hyperkeratotic tumor with more fibroblasts arranged in the cutis than in the first type. It also exhibits reduced elastic fibers.[1] Type III is the least common variant. Type III presents as a flat to dome-shaped lesion with a poorly cellular dermal core, edematous structures, and the absence of elastic fibers.[1]
History and Physical
In most cases, acquired digital fibrokeratoma presents as an asymptomatic protuberance that does not spontaneously regress.[5] Clinically, it appears as a solitary, skin-colored, well-defined papule with a characteristic hyperkeratotic collarette at its base.[16] It primarily occurs on the fingers and toes but can also be found in other areas such as the lower lip, nose, elbow, pre-patellar area, and periungual tissue.[1][7] The lesion size is generally smaller than 1 cm, but there have been reported cases of ADFKs larger than 1 cm, referred to as giant ADFKs.[4][7]
A variant of ADFK is known as multibranched acquired periungual fibrokeratoma (MAPFK), which has been documented in the literature. In MAPFK, multiple filiform papules along the cuticle resemble warts associated with human papillomavirus (HPV).[10]
Dermoscopy has been used to examine these lesions. Dermoscopy has shown filiform structures and significant variability in the dermoscopic findings due to possible vascular involvement and collagen fiber buildup within the lesions.[10]
Evaluation
The dermoscopic features of acquired digital fibrokeratoma have been rarely investigated and may differ among ADFK cases. Rubegni et al. described a central homogeneous pale-yellow core fringed by a hyperkeratotic white scaly collarette.[10][17] These features may reflect epidermal acanthosis, hyperkeratosis, and the presence of dense collagen fibers. A whitish-yellow area with dotted vessels was observed in the periphery, while globular vessels encircled the whole tumor externally.[17]
Hayashi et al reported the presence of red-clumped structures divided by white meshwork-like keratotic septa. These findings may correspond to the histological retraction of the epidermis.[10][18]
Treatment / Management
Various therapeutic options for ADFK, including cryotherapy, shave excision, curettage, and cauterization, are reported. However, surgical excision is considered the most effective and primary treatment modality. The tumor should be excised from its basal attachment to prevent the risk of recurrence.[19][20]
Lesions involving the nail plate may require the removal of the nail plate or other surgical intervention. In such instances, a dermatologist, Mohs micrographic surgeon, or other professional experienced in nail surgery may be necessary.[10]
Acquired digital fibrokeratoma has been associated with various conditions and factors. Infection caused by Staphylococcus aureus has been implicated in some cases, as well as an association with leprosy, particularly in individuals with reduced sensation.[10][21][22]
ADFK has been associated with other conditions, such as brain infarction, cyclosporine use in a renal transplant patient, pyogenic granulomas, pityriasis amiantacea, and psoriasis vulgaris.[10] However, many of these associations may result from trauma to the affected areas due to skin-picking behavior, and the associations are not fully understood.
Due to its histological resemblance to Koenen tumor, there have been discussions regarding a possible association between ADFK and tuberous sclerosis. While there are no clear guidelines regarding this association, it is suggested that patients with multiple lesions consistent with ADFK may warrant a cautious evaluation for other signs of tuberous sclerosis.[10]
Differential Diagnosis
Correctly identifying cutaneous lesions that mimic acquired digital fibrokeratoma is crucial to ensure appropriate and timely treatment. The differential diagnosis of ADFK includes the following:[7][8][23]
- Supernumerary digit, a common hereditary limb malformation, is found at the base of the fifth finger. Histologically, rudimentary polydactyly differs from ADFK by the presence of nerve bundles and neuroid elements.[6] ADFK can often be mistaken as a supernumerary digit, as demonstrated in a reported case by M. Ali et al., in which the histological report confirmed ADFK of the big toe.[7]
- Verruca vulgaris, commonly known as warts, is the most frequently occurring neoplasm of the hand and fingers. It is caused by human papillomavirus (HPV) types 1, 2, 4, and 29.[24] Clinically, common warts exhibit a pattern of tiny black dots known as thrombosed capillaries.[25] Yu and Morgan reported a case in which ADFK was misdiagnosed as common warts and recurred after cryotherapy.[8]
- A cutaneous horn is a clinical diagnosis referring to an exophytic and hyperkeratotic growth containing a column of keratin. Histological examination may reveal an underlying premalignant or malignant process. Cutaneous neurofibromas are benign tumors that may clinically resemble ADFK. They present as soft, polypoid, dome-shaped tumors on the skin.[26] Histological examination shows loosely spaced spindle cells, wavy collagenous strands, and a myxoid matrix.[5][27]
- Superficial acral fibromyxoma, also known as digital fibromyxoma, is another condition that can present as a well-circumscribed dome-shaped asymptomatic papule on the digits. Histologically, it shares similarities with ADFK.[10][28][29] However, digital fibromyxoma is likely to exhibit higher cellularity, and immunohistochemical staining for CD34 or CD99 is positive, while it is negative for ADFK.[28][29] Koenen tumor, also referred to as periungual fibroma, displays similar histological features to ADFK and may be a variant of ADFK or its own lesion. However, Koenen tumor has been associated with tuberous sclerosis.[23][30][31]
- Eccrine poroma may appear on the palms and soles as a tan-to-pink exophytic papule, though histologically, it will show cuboid cell proliferation (as it is an adnexal tumor) with intercellular bridges, unlike ADFK.[10][23]
- Pyogenic granuloma is a well-known vascular tumor that usually occurs in areas of minor trauma.[32] Clinically, it presents as a friable, dome-shaped, or pedunculated nodule with a scaly collarette. Other conditions such as dermatofibroma, papillary digital adenocarcinoma, or keratoacanthoma should also be considered when considering the differential diagnosis.[10]
Prognosis
Acquired digital fibrokeratoma is a benign tumor with no known risk of malignant transformation. Surgical excision is generally curative and carries a low risk of pain, bleeding, and infection.
After surgical treatment, patients can expect excellent functional recovery and a satisfying cosmetic outcome. With appropriate surgical management, the likelihood of the lesion reappearing is minimal.[20]
Complications
While ADFK generally does not lead to severe complications, there is a rare variant called periungual fibrokeratoma that may cause nail plate deformity and affect the function of the digit.[16]
Deterrence and Patient Education
The exact cause of ADFK is unknown. Therefore, no specific preventative measures can be taken to avoid its development. Patient education should include postoperative instructions to reduce the risk of complications such as infections.
Enhancing Healthcare Team Outcomes
Most patients with concerns about skin lesions first present to primary healthcare professionals. However, due to the vast number of skin lesions, it is essential to collaborate with a dermatologist when faced with an unknown or concerning skin lesion.
Dermatologists have specialized training and expertise in diagnosing and treating skin conditions, including differentiating between benign and potentially malignant lesions. Consulting with a dermatologist can provide valuable insights and guidance in accurately diagnosing and managing skin lesions, especially in cases where there is uncertainty or suspicion of malignancy.
Acquired digital fibrokeratoma is commonly diagnosed based on history and physical examination. Clinicians must be familiar with the various presentations of ADFK and be able to differentiate it from other skin conditions. Microscopic assessment and histological examination are necessary to confirm the diagnosis and identify histological variants.
Management of ADFK often involves surgical intervention with complete excision of the lesion performed by a dermatologist or a plastic surgeon. During the postoperative period, nurses are critical in providing incision care and monitoring for any signs of complications. Additionally, pharmacists collaborate effectively, as appropriate pain management significantly affects the patient's quality of life.
Pharmacists and nurses should remain aware during the treatment and follow-up process. If they detect any treatment failures or issues that may affect patient outcomes, they should report their concerns to the treating clinician.
Despite ADFK being a benign lesion, the principles of interprofessional team dynamics are essential. The involvement of clinicians, dermatologists, plastic surgeons, nurses, and pharmacists, among others, ensures comprehensive care and promotes better patient outcomes.