Etiology
Trichiasis[2]
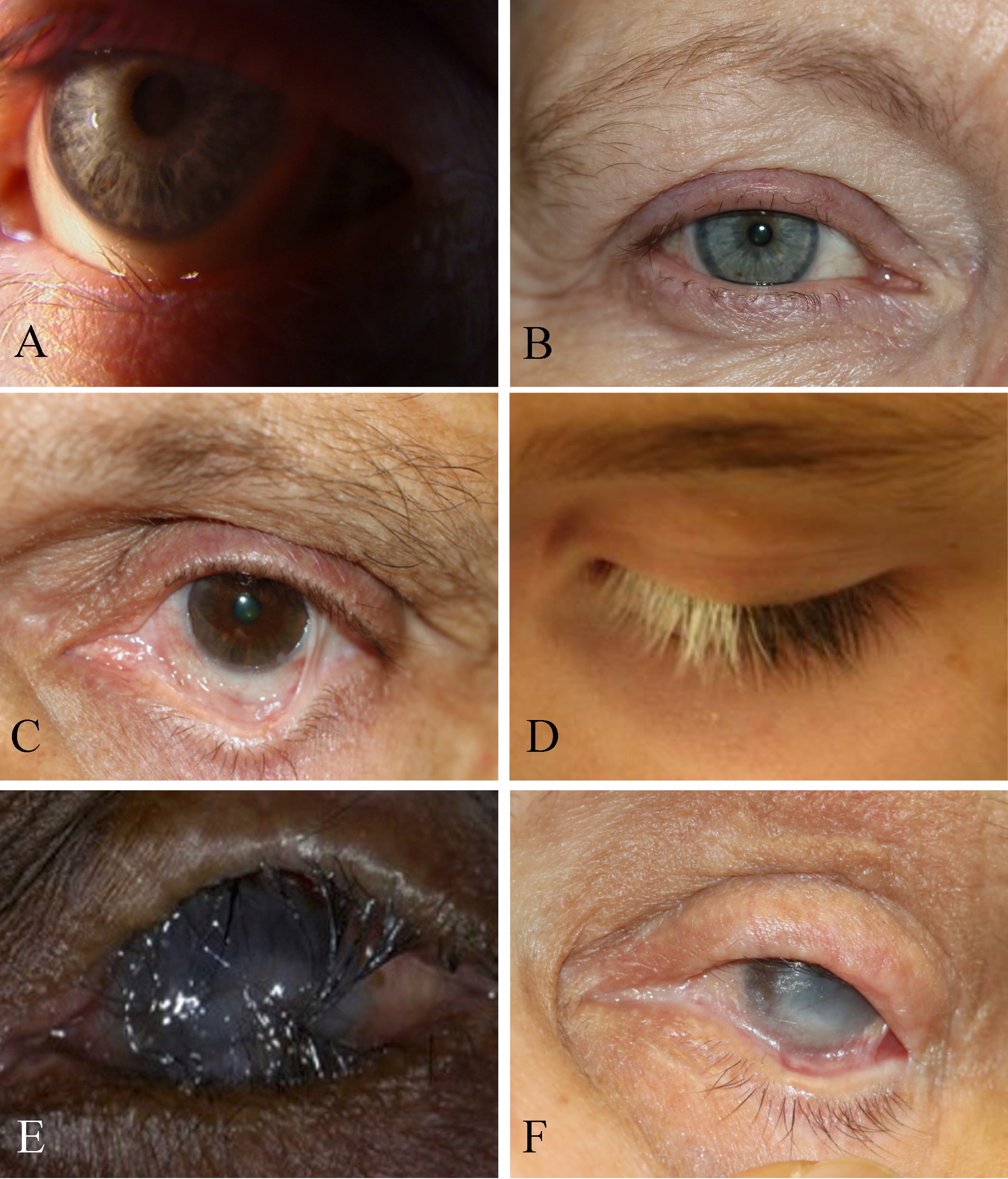
Trichiasis is defined as normal lashes growing inward. In trichiasis, the lash follicle is normal, but the direction of lash growth is abnormal. In the presence of inflammation, there may be a misdirection of the follicle with the lash growing inwards towards the cornea, but the cause is not entropion. Some authors have divided trichiasis into primary where the lash is misdirected by abnormal direction of the shaft of the hair and secondary trichiasis where there is a misdirection of the follicle. We have found this division less useful in clinical practice. Others have classified trichiasis as minor (less than five cilia) and major (more than five cilia). Mostly, trichiasis affects the lower eyelid.
Examination under the biomicroscope should assess the lid margin, the posterior lamella, and fornices (looking for symblepharon or scarring). An examination will reveal lashes pointing backward rubbing against the conjunctiva or the cornea. The lashes may be in their normal position may be growing from behind the normal eyelashes. Scarring of the eyelid margin secondary to inflammation should be looked for. Trichiasis is differentiated from involutional entropion, where the eyelid margin turns in and causes normal lashes to rub against the cornea. This is often termed secondary trichiasis or pseudo-trichiasis.
Causes
- Chronic blepharitis
- Vernal keratoconjunctivitis
- Chemical burns
- Thermal injury
- Eczema
- Herpes zoster
- Atopic diseases
- Ocular cicatricial pemphigoid disease
- Cicatrizing conjunctival disease
- Eyelid trauma
- Eyelid surgery
- Meibomitis
- Stevens-Johnson syndrome
- Leprosy
- Eyelid tumors
- Trachoma
- Chalazia: Sometimes one will see trichiasis at a site of a prior chalazion which may or may not have been surgically drained: the collapsed meibomian gland can cause a local change in the architecture with lashes turning in.
Mostly, trichiasis affects the lower eyelid, except in chemical burns (where both lids are affected) or trachoma, where the upper eyelid is more severely affected. Chlamydia trachomatis causes trachoma: the disease is endemic in sub-Saharan Africa. In trachoma, inflammation of the eyelid margin and conjunctiva will cause a combination of trichiasis as well as cicatricial entropion. Corneal scarring and eventual corneal opacification can occur.[3]
Management
Short-term relief may be obtained by epilating the lashes or inserting a bandage contact lens. Surgical treatment should only be undertaken after active inflammation is brought under control. Permanent destruction of the roots of the offending lashes is achieved using numerous techniques, including argon laser, electrolysis, radiofrequency epilation, trephination, eyelash bulb extirpation, resection of the lash follicle, cryotherapy, and surgical repositioning. We use the radiofrequency needle to the depth of the root of the lashes (2.4 mm deep in the upper lid and 1.4 mm in the lower lid) to kill the offending lash roots. Monopolar electrocautery is used less often now as it causes more collateral thermal injury to the eyelid margin.
Distichiasis[4]
Distichiasis is defined as a separate row of lashes that are present behind the normal row of lashes. These lashes are fine with little pigmentation but will cause corneal irritation. Various forms of distichiasis are seen, from a complete row of lashes to an irregular row. Distichiasis may be congenital, in which case the pilosebaceous units differentiate into lashes instead of meibomian glands. In the autosomal lymphedema-distichiasis syndrome,[4] distichiasis is associated with limb lymphedema, and there may be cleft palate and cardiac abnormalities. Other congenital causes of distichiasis include mandibulofacial dystonia and Setleis syndrome (focal facial dermal dysplasia with upper eyelid lashes present in multiple rows or eyelashes may be completely absent).
Secondary distichiasis is seen in conditions that cause inflammation which in turn leads to metaplasia of the Meibomian glands forming lashes within the Meibomian glands. These conditions are similar to those causing trichiasis, including blepharitis, caustic injuries, meibomian gland dysfunction, meibomitis, ocular cicatricial pemphigoid, and Stevens-Johnson syndrome,
Management
This includes epilation, use of cryotherapy, trephination, folliculectomy, lid split and treatment of the abnormal follicles and radiofrequency treatment of the follicles. In acquired distichiasis, there is eyelid inflammation (Meibomian gland dysfunction, cicatricial pemphigoid, Stevens-Johnson syndrome). Inflammation induces metaplasia of the Meibomian glands forming lashes within the Meibomian glands. There may be a need for application of a mucous membrane graft, particularly if there is mucocutaneous keratinization.
Tristichia/Tetrastichiasis
The presence of a third row of lashes. Tetrastichiasis is the presence of a fourth row of lashes. These are rare conditions.
Pseudocilium
Sometimes, an eyelash will be seen in a meibomian gland orifice or the punctum. We have termed this "pseudocilium" because the lash does not have root but is loose in the meibomian gland or the punctum. Such an isolated lash can find its way into a meibomian gland or punctum still and may have the tip of the lash on the outside or the root on the outside (upside down lash). Either way, the lash can still cause corneal and conjunctival irritation. Treatment is simply the removal of the lash from the orifice of the meibomian gland or the punctum.
Hypotrichosis
Hypotrichosis, which is defined as reduced hair density anywhere in the body may also affect eyelashes. The only effective treatment is the use of topical bimatoprost ophthalmic solution 0.03%. It is applied to the lash bases, resulting in lashes which are thicker, longer and darker. Bimatoprost is thought to prolong the anagen phase of the lash cycle. Results are seen in 16 weeks. A recent concern is that some patients may show atrophy of orbital fat after prolonged use of such topical bimatoprost solution. Side effects include increased iris pigmentation, skin pigmentation, and skin irritation, all of which will reverse with discontinuation of the medication.
Alopecia Adnata has been used to describe under-developed eyelashes. Alopecia areata, which is thought to be an autoimmune process, can also affect eyelashes.
Madarosis[5]
Madarosis is the loss of lashes (ciliary madarosis) or eyebrows (superciliary madarosis). Milphosis means eyelash loss. Madarosis and milphosis are often used interchangeably. Trichotillomania is the self-induced pulling of hair from anywhere in the body but is also applied to eyelash-pulling. In most cases, psychiatric evaluation and treatment are needed.
Causes
- Blepharitis
- Meibomian gland dysfunction
- Ocular rosacea
- Seborrheic blepharitis
- Staphylococcal infection
- Demodex infestation
- Trachoma
- Congenital syndromes like Oliver-McFarlane and Cornelia de Lange
- Alopecia Universalis is a type of alopecia which also results in loss of lashes. In this condition, corticosteroids and topical immunotherapy have been used successfully to achieve hair growth.
- T-cell lymphoma and associated follicular mucinosis
- Allergic contact dermatitis may be caused by many cosmetics and ophthalmic medications with preservatives and other chemicals.
- Superficial inflammation from any cause can lead to irritation and rubbing of the brows and lashes with pigmentation, skin laxity and lash loss.
- Psoriasis
- Atopic dermatitis, which may be associated with allergic rhinitis, keratoconjunctivitis, vernal conjunctivitis causes loss of lashes on the lateral third of the brows (termed Hertoghe’s sign).
- Acne rosacea results in blepharitis, keratitis, and telangiectatic changes on the cheeks and nose
- Alopecia areata may result in a patchy lash loss. The lashes have an “exclamation mark” configuration of broken hairs: this is pathognomonic of this disease.
- Discoid lupus erythematosus and systemic lupus erythematosus: chronic blepharoconjunctivitis and madarosis may occur.
- Scleroderma en coup de sabre, which is localized scleroderma will show a segmental loss of eyebrows and lashes
- Hypothyroidism may cause brittle hairs mostly affecting the brows, but also lashes
- Hyperthyroidism may cause ciliary madarosis
- Malignancy: basal cell carcinoma, squamous cell carcinoma, Merkel cell carcinoma, mycosis fungoides (cutaneous T-cell lymphoma), sebaceous cell carcinoma. Recalcitrant dermatitis and chronic blepharoconjunctivitis or recurrent chalazia should be indications for biopsy of the eyelid and eyelid margin.
- Chemotherapy
- Herpes zoster is a common cause of madarosis of the upper or lower eyelid. Secondary syphilis can cause outer eyebrow loss and eyelash loss. Leprosy as a cause is seen less frequently now. HIV/AIDS may cause madarosis or trichomegaly.
- Drugs: Systemic drug toxicity and local topical agents may cause madarosis.
- Trauma: Eyelid lacerations, chemical, and thermal injuries and tattooing can all cause madarosis.
- Trichotillomania is a condition in which patients pull hair (scalp being the most common, followed by eyelashes). As these are episodic, may be confused with alopecia areata. A biomicroscopic examination will show broken hairs of different lengths with no underlying skin condition. Trichoteiromania is a loss of hair by repeated rubbing and trichotemnomania is a loss by obsessive shaving.
- Congenital diseases: numerous diseases are associated with hair loss, including ectodermal dysplasias, Ichthyosis-cheek-eyebrow syndrome, localized autosomal recessive hypotrichosis, ectodermal dysplasias, Rothmund-Thompson syndrome.
Management
With such a disparate list of causes of eyelash milphosis (madarosis), the underlying condition has to be diagnosed and treated. Eyebrow transplants may of be used for superciliary madarosis. Eyelash transplants have not gained popular acceptance because of the risk of trichiasis and lack of lifelike hair on the lid margin. Successful take is not predictable (depending upon the underlying disease and condition of the eyelid). Composite eyebrow grafts may be used to reconstruct eyelids with segmental eyelash loss.
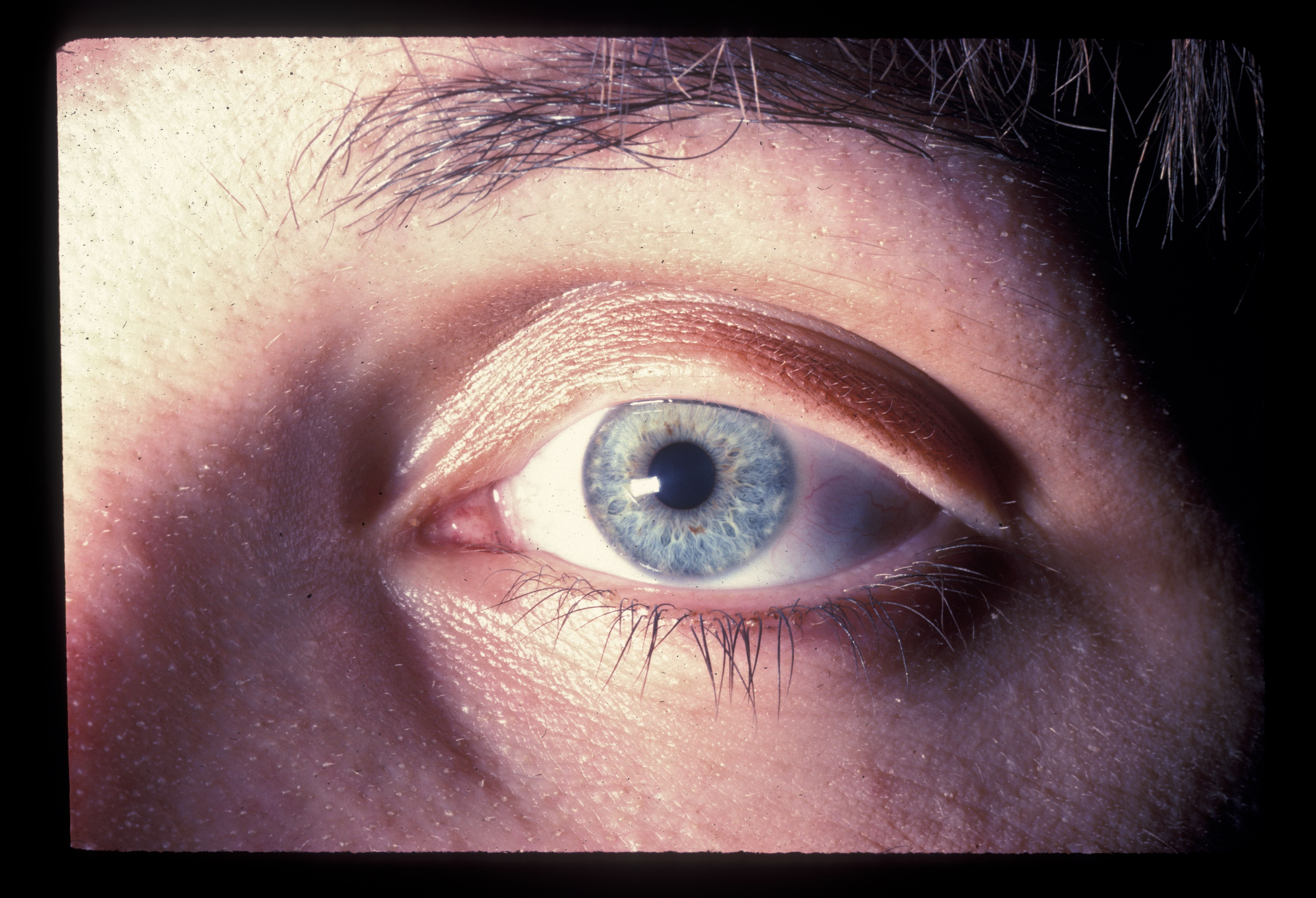
Hypertrichosis is an increase in hair in any area of the body taking the patient’s age, gender, and ethnicity into consideration. Eyelash hypertrichosis is known as trichomegaly.[6] As with madarosis, the list of diseases associated with hypertrichosis and trichomegaly is long:
- Congenital hypertrichosis languinosa and generalized hypertrichosis cause an increase in hair on the body as well as eyelashes.
- Neurofibroma
- Cornelia de Lange syndrome
- Goldstein Hutt syndrome
- Phenylketonuria
- Type I oculocutaneous albinism
- Tyrosinemia
Eyebrow Hypertrichosis is seen in:
- Coffin-Siris syndrome
- Gingival fibromatosis with hypertrichosis
- Hermansky-Pudiak syndrome
- Mannosidosis
- Nevoid hypertrichosis (isolated area of hypertrichosis)
- Stiff skin syndrome
- Langer-Giedion syndrome
- Duplication supercilia (two distinct brows)
- Mucopolysaccharidoses
- Rubenstein-Taybi syndrome
- Cornelia de Lange syndrome
Acquired Hypertrichosis (Hypertrichosis lanuginosa acquisita [HLA])[7]
- Drugs
- Metabolic diseases
- Endocrine diseases
- Paraneoplastic processes: patients may develop increased lanugo develop lanugo hairs in the periocular, ear, forehead and nose areas. In paraneoplastic processes, hypertrichosis may develop before malignancy is recognized.
- Lawrence-Seip syndrome consists of lipoatrophy resulting hypertrichosis of the head with the involvement of the forehead, eyebrows, eyelashes, and cheeks.
Trichomegaly (increased eyelash and/or eyebrow length)
- Anorexia nervosa
- Atopic dermatitis
- Allergic rhinitis (results in long smooth lashes)
- Dermatomyositis
- Hypothyroidism
- Malnutrition
- Pregnancy
- Hypothyroidism
- Porphyria
- Systemic lupus erythematosus
- Linear scleroderma
- Vernal keratoconjunctivitis
- Uveitis
- Voght Koyanagi Harada syndrome
- HIV/AIDS may cause trichomegaly as well as madarosis
- Many drugs have been associated with trichomegaly, causing thickening and even curling. The common ones are being prostaglandin analogs used to treat glaucoma (e.g., latanoprost, bimatoprost), epithelial growth factor receptor tyrosine kinase inhibitors, cyclosporine, topiramate, tacrolimus, and interferon-alpha.
- Cone-rod dystrophy
- Goldstein Hutt syndrome
- Kabuki makeup syndrome
- Olver-Macfarlane syndrome
- Phenylketonuria
- Type I oculocutaneous albinism
- Tyrosinemia
Management
Treatment is similar to that which is outlined under trichiasis if there is irritation of the eye or in the presence of associated trichiasis.
Synophrys is commonly termed “unibrow” or "monobrow." Synophrys is seen in centrofacial lentiginosis, cretinism, Sup (3q) syndrome, fetal trimethadione syndrome, Hajdu Cheney syndrome, and Waardenburg's syndrome. Laser hair removal may be used to separate the brows. [8]
Cilia Incarnata
Cilia Incarnata is a term used to describe an eyelash that burrows under the skin to either the surface (cilium incarnatum externum) or posteriorly through the tarsal conjunctiva (cilium incarnatum internum). These conditions are discussed in detail elsewhere. The eyelash root is normal, just the direction of growth of the shaft of the lash is abnormal. A patient with cilia incarnata internum will present a history of irritation of the eye with localized punctate keratopathy, a patient with cilia incarnata externum may present asymptomatically or with a complaint of "a bump." Both conditions are diagnosed by examining under the biomicroscope. Simple removal of the lash is almost always curative.
Eyelash Ptosis
Eyelash ptosis is defined as a downward curve or bend to the upper eyelid lashes. Normal upper eyelashes have an upward curve. A normal eyelash curve, bend, and position are determined by underlying integrity of the orbicularis oculi muscle, the Riolan’s muscle which is part of the orbicularis oculi muscle at the eyelid margin and the tarsal plate and elastin. If any of these structures are affected by trauma or disease, eyelash ptosis can occur.
The commonest medical condition associated with eyelash ptosis is the Floppy Eyelid Syndrome (FES) where the tarsal plate, the orbicularis muscle, and eyelid elastin are all affected. The findings are almost always asymmetric as the side the patient sleeps on will have more pronounced findings of eyelid floppiness and eyelash ptosis. Patients will present with red, irritated eyes, mucoid discharge from the eyes which is worse in the mornings, a papillary conjunctival inflammation, sleep apnea and a history of weight gain (and loss).[9]
The commonest non-medical cause of eyelash ptosis is seen in patients treating their lashes with prostaglandin analogs for glaucoma which also results in trichomegaly.
Other conditions associated with eyelash ptosis are:
- Ptosis, congenital and acquired
- Leprosy
- Facial nerve palsy
- Dermatochalasis with anterior lamellar slide.
Lower Eyelid Lash Ptosis (upward slant to lashes)
- Epiblepharon is the commonest cause. This is commonly seen in Asian races. A medial lower eyelid fold of skin and orbicularis is found making the medial lashes turn upward, which may be termed lower eyelid lash ptosis. Although many patients show regression with age, some patients require a modified Hotz procedure to evert the medial lower eyelid.
- Thyroid orbitopathy, although this is more of a mechanical malposition caused by surrounding structures (the orbicularis in epiblepharon and proptosis and periorbital edema in thyroid orbitopathy).
Management
Treatment depends upon the cause. We tell all patients with the floppy eyelid syndrome that a permanent cure is defined and long-term weight loss. Indeed, we have seen impressive improvement without any surgical treatment when a patient successfully loses and maintains the decreased weight. Although the use of shields and lubricants can help, the definitive “cure” is for the patient to lose weight. Surgical resection of redundant rubbery upper and lower eyelids in a full-thickness manner is reserved for recalcitrant cases, with the proviso that this does not cure the condition and merely helps to create a firmer eyelid to protect the cornea. If there are continued weight gain and weight loss, together with “face sleeping,” the condition recurs. Also, the lashes often need to be trimmed as they tend to be long with a downward slope. Cessation of prostaglandin analogs causes a reversal of the lash changes within a few months in patients with glaucoma drop-induced lash ptosis
Cilium Inversum ("upside down lash")
Sometimes, the same condition will receive two names. Cilium inversum appeared in 1923 in the BMJ (Tibbles), followed by Schrieber in 1924. Subsequently, there have been no further reports because this condition of cilium inversum is the same as cilium incarnatum internum Definition: the finding is exactly that seen in cilium a report in 1924 by Schrieber.
Ectopic or Accessory Cilia[10]
Ectopic or accessory cilia are lashes that are Definition: lashes that found away from their normal location which is the eyelid margin. Weigmann first described this in 1936. This condition is seen when the lashes grow through the tarsal plate and present in an area of the upper or lower eyelid, but the roots of the lashes are not at the eyelid margin. True ectopic cilia are seen congenitally. Traumatic ones are, of course, displaced cilia and are not true ectopic cilia. A positive family history of ectopic cilia may be obtained. With accessory cilia, histology will reveal the presence of apocrine sweat glands attached to the follicle which is necessary to diagnose the hairs as eyelashes. The lashes are managed with surgical resection or cryotherapy to remove the offending lashes permanently.
Buried Lash with Granuloma
A granuloma may form around a broken lash which embeds itself in the conjunctiva causing local inflammation. This may be seen on the tarsal conjunctiva, or, more infrequently, in the forniceal conjunctiva. Simple removal of the lash is curative.
Vellus Hair Cyst Eyelid/Orbit[11]
Sometimes, a vellus cyst may develop in the orbit and resemble an orbital tumor. Again, simple removal of the granuloma and offending lash are curative.
Poliosis
Canities is the natural gradual graying of hair shafts because of tyrosine production decrease in the hair bulb whereas poliosis is the decrease or absence of pigment in hair anywhere on the body. It is caused by abnormalities of hair melanocytes or hair melanin in the follicles. Poliosis is seen in many conditions:
- Piebaldism
- Conjunctival melanoma
- Vitiligo
- Sarcoidosis
- Inflammatory systemic diseases
- Blepharitis
- Vernal keratoconjunctivitis
- Topical prostaglandin analogs
- Medications like chloramphenicol, cyclosporin A, chloroquine.
- Oculocutaneous albinism will manifest with fair lashes
- Griscelli syndrome (hypopigmentation of skin and hair with neurological deficits)
- Vogt-Koyanagi-Harada syndrome (uveitis, serous retinal detachment).
- Sympathetic ophthalmia
- Cicatricial pemphigoid
- Herpes zoster
- Irradiation
- Idiopathic uveitis
- Tuberous sclerosis
- Marfan syndrome
- Waardenburg syndrome (white forelock with scalp hair, eyebrow, and eyelash poliosis).
- A mycotic infection called white Piedra is caused by a yeast (Trichosporon) resulting in white nodules which may be mistaken for poliosis. This is treated with topical and systemic azoles.
- There is no medication available to restore lash pigmentation.
Heterochromia is a rare condition of eyelash color differences between the right and left eyelashes.
Abnormal Darkening of Lashes
Abnormal darkening of eyelashes may be seen in Diabetes type II and as a side effect of prostaglandin F2 alpha agents (which increase melanin production and melanocytes).
Malformed Hair/Brittle Hair
Monilethrix (a rare autosomal dominant disease) and pili torti (gives corkscrew hairs and involves eyebrows, lashes, temporal and occipital scalp) cause brittle hair. Scurvy is caused by vitamin C deficiency with corkscrew hairs, perifollicular hemorrhages, gingival hemorrhage, fractured and bent hairs (swan-neck deformity). Menkes syndrome is a disorder of copper metabolism and highly fatal condition. Hair will show “steel wool” quality and have seizures, hypotonia, and failure to thrive.
Trichorrhexis Invaginate is seen in the Netherton syndrome with atopic dermatitis and lichenification. Trichorrhexis invaginate refers to bamboo hair where the hair shaft will have nodules along it which is pathognomonic for Netherton disease. Brow hair is affected as is scalp hair.
Benign Tumors of Hair Follicle
Pilomatrixoma presents as a firm lesion with whitish nodules usually away from the eyelid margin.
Trichoblastoma
Trichilemmoma rarely affect the lid margin or canthus
Trichoepithelioma
Trichofolliculoma presents as a nodule with fine, white hair in the middle.
Inverted Follicular Keratosis
Malignant Tumors of Hair Follicle
Primary mucinous carcinoma arises from eccrine sweat glands and presents as a nodule or ulcer.
Infection of Hair Follicle
Common bacteria found naturally on lashes are Propionibacterium, Streptophyta, Staphylococcus, Corynebacterium, and Enhydrobacter. In the presence of blepharitis, Staphylococcus, Streptophyta, Corynebacterium, and Enhydrobacter are increased. Propionibacterium, on the other hand, is often decreased in blepharitis.
An infection of the gland of Zeis (sebaceous gland) and gland of Moll (apocrine gland) will give rise to a “stye” also called an external hordeolum (as opposed to an internal hordeolum, which is a chalazion, or infection of the Meibomian gland within the tarsal plate). Infection along the eyelid margin will have secondary effects on the hair follicles. Staphylococcal blepharitis results in crusts on lashes, squames or scales on the lid margins, telangiectatic vessels and collarettes around lashes. There may be associated Meibomian gland dysfunction. In more chronic blepharitis, there may be madarosis, poliosis, tylosis, trichiasis and eyelid margin irregularities.
Lash Infestation
Demodex folliculorum and Demodex brevis are parasites that are found on eyelashes. [12] Numbers increase with age so that by age 70, almost 100% of people will have these parasites. D. Folliculorum lives on hairs in brows, scalp, ears, and lashes. D. brevis is seen in Meibomian glands and sebaceous glands of the face. Demodex is an impressive parasite under magnification: it has a head, four pairs of legs, a body and tail which contain the digestive system and no anus, so the ingested material is eventually released when the parasite bursts. The parasite has a life cycle of 15 – 18 days. The released contents cause inflammation of the eyelid margin. With an increasing numbers of Demodex comes an increased incidence of blepharitis and demodicosis of the eyelid margin. Gelatinous debris is seen along the eyelid margin and cylindrical dandruff around the lashes is pathognomonic of demodex. Pubic hair is infested with Phthirus pubis which can be transmitted to eyelashes by hand and sexual transmission. This can result in Phthiriasis palpebrum: the parasite has brown scales which are actually the parasite’s feces. [13] Nits are unhatched parasites which will be seen along the lid margin and fixed to the lashes. The patient develops eyelid margin irritation, itching, and inflammation. Management of Phthiriasis palpebrarum requires mechanical removal of the parasite and the nits.
Iatrogenic Conditions
An explosion in periocular and periorbital aesthetics has led to lash tinting, application of lash extensions with glues, eyelash and eyelid cosmetics, dyes, and other sundry procedures and use of chemicals. Inevitably, contact dermatitis is on the rise, often caused by glues and lash tinting dyes. Eyelid margin tattoos performed to enhance the appearance of the eyelashes can cause "leakage" of the dye with diffusion needing laser treatments to reduce the pigmentation. With tattoo inks being imported, allergic reactions are also being seen. Lash tinting uses dyes containing Eyelash tinting, extensions, phenylenediamine which are known to cause allergic dermatitis. Overuse of mascara can lead to lash cuticle cracking and also milphosis.
Trauma
A not uncommon injury to lashes is caused by inadvertent application of super glue (cyanoacrylate) into the eye when the tube is mistaken for an ocular ointment. These injuries have continued since 1982 when cyanoacrylate was begun to be sold in small tubes which resemble eye ointment tubes. Nail glue often comes in bottles which look like eye medication bottles. Most modern super glues harden immediately upon contact with moisture which makes it impossible for the patient to open the eyelids. The eyelids and lashes will be glued together. Although the eyelid margins may be stuck to each other, commonly it is the upper and lower eyelid lashes that are stuck. Warm soaks and irrigation will help to loosen the glue on the lashes and eyelids and can sometimes allow the eyelids to be prised open. However, it is often necessary to cut or trim the lashes to allow the lids to be opened. The eye should be examined for any hardened fragments of glue which should be removed after a topical anesthetic has been applied. The cornea should be examined for abrasions and the standard corneal abrasion management should be undertaken. [14] If there is partial adherence of the eyelids and the cornea can be examined to ensure there is no trauma, it is not unreasonable to prescribe topical ointment three times a day and warm soaks. This allows the super glue to soften over a few days when the lids can be gently prised open with little cutting of lashes.
Pathophysiology
Trichiasis
Trauma and inflammation distort the tissue around the lash root, causing the lash to grow in an abnormal direction, in this case inwards towards the eye. The eyelid position is normal although some of the cicatrizing diseases may cause an inward turn of the eyelid margin before going on to frank cicatricial entropion.
Distichiasis
Metaplasia of the Meibomian glands results in the formation of lashes instead of the sebum-producing glands and may be seen congenitally or following eyelid inflammation.
Madarosis
Trauma, inflammation or ischemia by malignancy are involved in madarosis. The exact mechanism in conditions such as hyperthyroidism and hypothyroidism are not known.
Trichomegaly
When caused by drugs such as latanoprost and bimatoprost, the anagen phase of the lash cycle is prolonged, resulting in longer, thicker lashes. The same mechanism may be involved when trichomegaly is seen with other drugs.
Cilia incarnata internum and externum
In both these conditions, it is thought that the natural growth path of a lash is impeded as the condition is almost always seen affecting a solitary lash. With the resistance, the may take the path of least resistance and grow outwards under the skin (externum) or through the tarsal plate and tarsal conjunctiva (internum).
Eyelash Ptosis
An abnormality in any of the structures that are responsible for the proper orientation of the lash follicle and shaft can result in eyelash ptosis. These structures are the pre-tarsal orbicularis oculi, Riolan’s muscle (which is the inferior part of the orbicularis oculi), the tarsal plate and the elastin. All of these are affected in conditions like the floppy eyelid syndrome and facial paralysis, giving rise to lash ptosis.
Poliosis
Abnormalities of hair melanin in the follicles or hair melanocytes can cause poliosis.
Demodex
An increase in the number of the normal parasites Demodex folliculorum and Demodex brevis occurs with age so that by the age of 70 years, almost everyone will have these parasites. As their numbers increase, they cause increased symptoms of irritation, itching, and discomfort.
History and Physical
Most of the lash conditions are diagnosed by clinical examination: the relevant findings have been presented above.
In the presence of trichiasis, a careful examination of the eyelid margin, the tarsal conjunctiva, the fornix, the bulbar conjunctiva, and the cornea is vital to exclude some of the more serious conditions which may initially present just with trichiasis.
Trichiasis with Evidence of Lash Loss
Examine the eyelid margin under the biomicroscope for vessels, ulceration, plaques, irregularities which may indicate eyelid malignancy (basal cell carcinoma, squamous cell carcinoma).
Trichiasis with Evidence of Lash Loss and Thickened Eyelid
Beware the sebaceous carcinoma which can present like a chalazion, vague lid thickening or with loss of lashes as well as trichiasis. Here a full-thickness specimen of the eyelid is sent fresh to the pathologist for special stains and immunohistochemistry.
Trichiasis with Conjunctival Scarring
Examine the tarsal conjunctiva and the fornix for scarring and symblepharon. Trichiasis can be the first presentation of mucous membrane pemphigoid (MMP) disease.
Trichiasis with Conjunctival Scarring, Entropion, Corneal Opacification
Advanced stage trachoma will present with frank cicatricial entropion, corneal scarring, decreased vision, and conjunctival inflammation. The earlier stage of the disease will show follicular conjunctivitis with limbal follicles and limbal neovascularization.
Madarosis
Always examine the area of madarosis for underlying growth/thickening/ulceration/vascularization which may be indicative of a malignancy.