Continuing Education Activity
Monoarticular arthritis is an inflammation of one joint that may later involve other joints of the body. The differential diagnosis and treatment of subclasses of monoarticular arthritis like infectious arthritis, crystal-induced arthritis, gout, pseudogout, and septic arthritis are also discussed. This activity reviews different types of monoarticular arthritis concerning their clinical presentation and will help clinicians and other interprofessional team members to recognize early signs and symptoms of monoarticular arthritis, which prompt early interventions.
Objectives:
- Explain the etiology of various kinds of monoarticular arthritis.
- Review the risk factors associated with monoarticular arthritis.
- Describe the epidemiology of monoarticular arthritis.
- Outline the importance of communication and healthcare delivery between health practitioners in the evaluation, management, and treatment of monoarticular arthritis.
Introduction
Monoarthritis is inflammation of one joint characterized by joint swelling, pain, warmth, and sometimes fever and periarticular erythema. Arthritis is often associated with joint stiffness and total loss or decreased range of motion.
Etiology
The etiology of monoarticular arthritis can be acute or chronic. Acute causes include infection, trauma, crystal-induced arthritis, avascular necrosis, and mechanical derangement.[1] Chronic conditions usually cause polyarthritides (i.e., involving more than one joint) such as systemic rheumatic diseases, which includes seronegative spondyloarthritis, osteoarthritis, and rheumatoid arthritis; however, polyarthritis can initially manifest as monoarthritis.
Virtually every bacterium can potentially cause septic arthritis, but depending on host risk factors, it can subdivide into gonococcal and non-gonococcal septic arthritis. Gonococcal arthritis results from sexually transmitted bacteria Neisseria gonorrhea; a gram-negative diplococcus, when spread in blood, can lead to disseminated gonococcal infection (DGI).[2][3] It can present as a triad of symptoms like vesiculopustular skin lesions, tenosynovitis, and arthritis (arthritis-dermatitis syndrome). However, DGI without skin lesions has also appeared in the literature.[4][5] The risk factor for DGI includes young individuals with multiple sexual partners, complement deficiencies, HIV, menstruation disorders, intrauterine device (IUD), pregnancy, and history of pelvic disease/surgery. The diagnosis is possible with a detailed history and physical, blood cultures, culture of synovial fluid of the affected joint and skin lesions like pharynx, urethra, cervix, or rectum.
Staphylococcal aureus (S. aureus) is the most common cause of nongonococcal septic arthritis; followed by Streptococcus species and gram-negative bacteria.[6][7] Septic arthritis generally affects larger joints of the body like the knee and hip, but wrist and ankle can also be affected. Septic arthritis can develop either from hematogenous seeding due to bacteria in the blood (bacteremia), direct inoculation of joint secondary to trauma or penetrating wounds (animal or human bite), or contiguous spread of infection from bone into the joint cavity.[8] The risk factors include intravenous drug use, prosthetic joints, indwelling catheters, chronic kidney disease, diabetes, malignancy, rheumatoid arthritis, and immunocompromised patients. Septic arthritis is a medical emergency, and synovial fluid analysis with gram stain and culture are the most important steps in the diagnosis. Clinically, collection of arthrocentesis and blood cultures should take place before the administration of antibiotics. Mycobacterium and fungi are rare causes of monoarticular septic arthritis. In these cases, predisposing factors like immunocompromised state or travel to endemic areas are usually present in the history of the patient.
Late stages of Lyme disease can also present as monoarticular arthritis and frequently involves the knee joint. Lyme serology is necessary for the diagnosis because synovial or tissue culture is always negative. Certain viruses like hepatitis B, hepatitis C, parvovirus, Epstein Barr virus (EBV), human immunodeficiency virus (HIV), alphavirus (e.g., chikungunya virus) and Zika virus can manifest with monoarticular arthritis/ arthralgia.[9] Most viral illnesses are self-limited; however, travel history, vaccination status, and targeted serology may be indispensable to rule out serious medical conditions like HIV and hepatitis.
Crystal-induced arthritis characteristically presents with deposition of chemical compounds, monosodium urate (MSU) in gout, calcium pyrophosphate dehydrates (CPPD) in pseudo-gout, and calcium hydroxyapatite in calcific periarthritis (calcium crystal disease).[10] A classic gout attack involves the single joint of the lower limb usually the first metatarsophalangeal joint (podagra), or in the midfoot, ankle or knee. Gout is an inflammatory process associated with the formation and reversible deposition of uric acid (MSU crystals) in the joints, and extra-articular tissues of the body. Classic presenting features include severe pain, swelling, erythema, and disability but rarely causes joint destruction.[11] Risk factors comprised excessive alcohol use, male gender, dehydration, trauma, surgery, metabolic disorders (e.g., diabetes), hypertension, chronic kidney disease, and drugs (hydrochlorothiazide, loop diuretics) that can predispose the patient to a gout flare. Diagnostic confirmation is with the evaluation of synovial fluid aspirate of the affected joint and visualization of intracellular MSU crystals under the polarized light. The crystals are negatively birefringent under polarized light.
Pseudogout is an acute attack of synovitis by deposition of CPPD crystals in a joint. The crystals are positively birefringent under the polarized light, as seen in the joint aspirate and connective tissues of the body.[12] Pseudogout frequently involves the knee joint but can also present in the ankle, shoulder and wrist joints. Clinically, it may be associated with metabolic and endocrine disorders like hemochromatosis.[13] Seronegative spondyloarthritis (e.g., psoriatic arthritis, reactive arthritis) can manifest as monoarthritis and likely affect joints of the lower extremity.[14] Certain chronic conditions such as osteoarthritis, rheumatoid arthritis, and bone neoplasms may arise as monoarthritis and later involve other joints of the body.
Epidemiology
Each year, nearly 20000 cases (7.8 cases per 100000 person-years) of septic arthritis occur in the United States. DGI is the most common cause of monoarticular arthritis in a young sexually active person (75% of cases), with 2.8 cases per 100000 person-years.[15] In the past, the prevalence of DGI was thought to be higher in females, but recently due to the increasing rate of HIV in men who engage in sex with other men, DGI is increasing in the male population in the United States.[16] S. aureus is the most common cause of septic arthritis in Europe and all non-gonococcal septic arthritis cases in the United States.[16] The prevalence and incidence of gout have been on the rise and accounts for more than 7 millions emergency visits in the United States. The rate of gout is higher in men as compared to women and affects 3% of the population worldwide.[17]
Pathophysiology
Septic arthritis can develop either from hematogenous seeding due to bacteremia, direct inoculation of joint secondary to trauma or penetrating wounds (animal or human bite), or contiguous spread of infection from bone into the joint cavity. Gout and pseudogout are caused by deposition of crystals into the joint fluid. The most common findings for monoarticular arthritis include joint swelling, pain, warmth, and sometimes fever and periarticular erythema, joint stiffness, and total loss or decreased range of motion.
History and Physical
History and physical are the key aspects of clinical evaluation that help in establishing the chronology of symptoms. They aid in selecting the relevant diagnostic testing and prevent unnecessary work up in the patient. According to American Academy of Family Physician (AAFP) guidelines, important elements of patient history includes age, gender, recent trauma, family history of joint diseases, review of systems, medication use, illnesses, travel history, tick bites, diet, alcohol use, occupational assessment, and intravenous drug use require careful consideration when suspecting monoarticular arthritis.[4][18]
The presence or absence of effusion or synovitis can be helpful to narrow the diagnosis to inflammatory arthritis and systemic rheumatic diseases. Warmth and swelling over a joint can be palpated through a physical exam and are hallmark signs of synovitis.[19]
Evaluation
Laboratory tests (blood chemistries, urinalysis) and diagnostic modalities (X-rays, CT scans, MRI) should be considered to confirm clinical impression and to plan future treatment. According to AAFP guidelines, complete blood count (CBC), erythrocyte sedimentation rate (ESR), and arthrocentesis for cell count and culture should be done for the evaluation of septic arthritis whereas microscopic evaluation of crystals and uric acid level along with afore-mentioned test are helpful in the diagnosis of crystal-induced arthritis.[18] Urine PCR, synovial fluid analysis for N. gonorrhea, and blood cultures should be done in case of gonococcal arthritis, while HLA-B27 and radiologic imaging may be used to confirm ankylosing spondyloarthritis.
Radiological imaging should be done in case of trauma or focal bone pain to rule out fracture or necrosis of the bones. X-rays of an affected joint can also help to see other abnormalities, including the presence of effusions, calcifications, tophaceous erosions, and inspection of joint cartilage and space. Ultrasound can also detect joint effusion and guide arthrocentesis procedure for joint areas that are difficult to access. CT-scan and MRI are reserved for deep-seated joints such as hip and shoulder. Overlying cellulitis is a contraindication for synovial fluid aspiration.
Treatment / Management
Treatment of monoarticular arthritis depends on the etiology and severity of the condition. Generally, pain control and reducing damage to the joint are the primary goals of the treatment. Appropriate antimicrobial therapy may be administered in case of septic arthritis to prevent the spread of infection to the surrounding tissues. Intra-articular or systemic steroids and anti-inflammatory drugs may be used to suppress the immune system in crystal-induced arthritis, urate-lowering or uricosuric drugs are used to prevent future recurrence of the disease.
Differential Diagnosis
The most important feature of diagnosis of monoarticular arthritis is to differentiate joint pain from the soft tissue conditions like bursitis or tendinitis that tend to mimic similar symptomology. Timing of symptoms is particularly crucial in this regard. For example, rapid onset of monoarticular pain in seconds or minutes can be signs of trauma, fracture, dislocation/derangement or presence of a loose body in joint. Pain that has onset over several hours to days generally indicates infection or crystal-induced arthritis, whereas pain over days to weeks may be an early sign of chronic conditions like osteoarthritis or rheumatoid arthritis.[18] Certain factors like intravenous drug use or patient on immunosuppression medications can potentially increase the risk of septic arthritis. Triad of symptoms, including urethritis, conjunctivitis, and arthritis after an infection is telltale signs of reactive arthritis.[20]
Treatment Planning
Treatment will depend on the etiology of monoarticular arthritis. Empiric antibiotics are necessary for septic arthritis based on likely etiology, which will later be tailored based on synovial fluid cultures. Provide analgesia for gout and pseudogout within 24 hours of symptom onset for best results. Corticosteroids, non-steroidal antiinflammatory drugs (NSAIDS) and colchicine are equally effective in treating acute flares of gout and pseudogout with NSAIDs being the first line treatment.[21] NSAIDs are the first-line treatment with indomethacin, historically being the first-line choice, but no evidence exists for its superiority to other NSAIDs.[21]
Colchicine is another treatment option but does not provide analgesia and is less effective if given beyond 72 to 96 hours after symptoms begin. It should be used with caution in patients with hepatic or renal impairment, and side effects include nausea, vomiting, and diarrhea.[22] Another second-line treatment for those who cannot tolerate NSAIDs is corticosteroids.[22] Caution is necessary when using corticosteroids with patients with diabetes mellitus as it can alter there blood glucose levels.
Prognosis
Prognosis of monoarticular arthritis depends on factors such as time to diagnosis, and initiation of treatment.
Complications
Septic arthritis without treatment may rapidly lead to severe complications such as osteomyelitis, necrosis, bony erosions, fibrous ankylosis, sepsis, and death. Gout can lead to joint damage/deformity, tophi, kidney stones, and renal failure.
Deterrence and Patient Education
Arthritis simply means inflammation of a joint. Various possible causes can affect a joint. It can be an injury from trauma, age-related osteoarthritis, a bacterial infection in the case of septic arthritis, autoimmune-like rheumatoid arthritis, and others. The early sign and symptoms include joint pain, red and/or warm skin over the joint, stiffness, and decreased range of motion. The patient should see a primary care physician who determines if a specialist consult (i.e., rheumatology, orthopedist) is required. A comprehensive history and physical exam, laboratory tests, and imaging studies are sufficient to determine the etiology of arthritis. The mainstay of treatment is by medications, but sometimes surgery is also required if a foreign body is involved, or there is internal damage to the joint.
Pearls and Other Issues
- Septic arthritis is an emergent condition that necessitates empiric antibiotics and synovial fluid analysis
- Gout and pseudogout treatment should focus on pain control
- Use caution when prescribing colchicine especially in patients with hepatic and renal impairment
Enhancing Healthcare Team Outcomes
It is vital for clinicians, including nurse practitioners, to recognize early signs of inflammation in a joint, especially septic arthritis. Joint aspiration should take place, and the patient started immediately on antibiotics if the fluid reveals the presence of bacteria. Early interventions can lower morbidity and mortality for patients.
All patients need to follow up to ensure that the condition is not worsening. Some patients may benefit from temporary offloading of the extremity, and others may require an ambulatory device. Physical therapy is recommended for all patients to regain muscle strength and joint function. The pharmacist should educate the patient on pain management. The dietitian should recommend a weight loss program if obese and consumption of a healthy diet. Finally, the nurse should educate the patient on safe sex practicies to prevent gonococcal arthritis.
Monoarticular arthritis requires an interprofessional team approach, including physicians, specialists, therapists, specialty-trained nurses, and pharmacists, all collaborating across disciplines to achieve optimal patient results. [Level V]


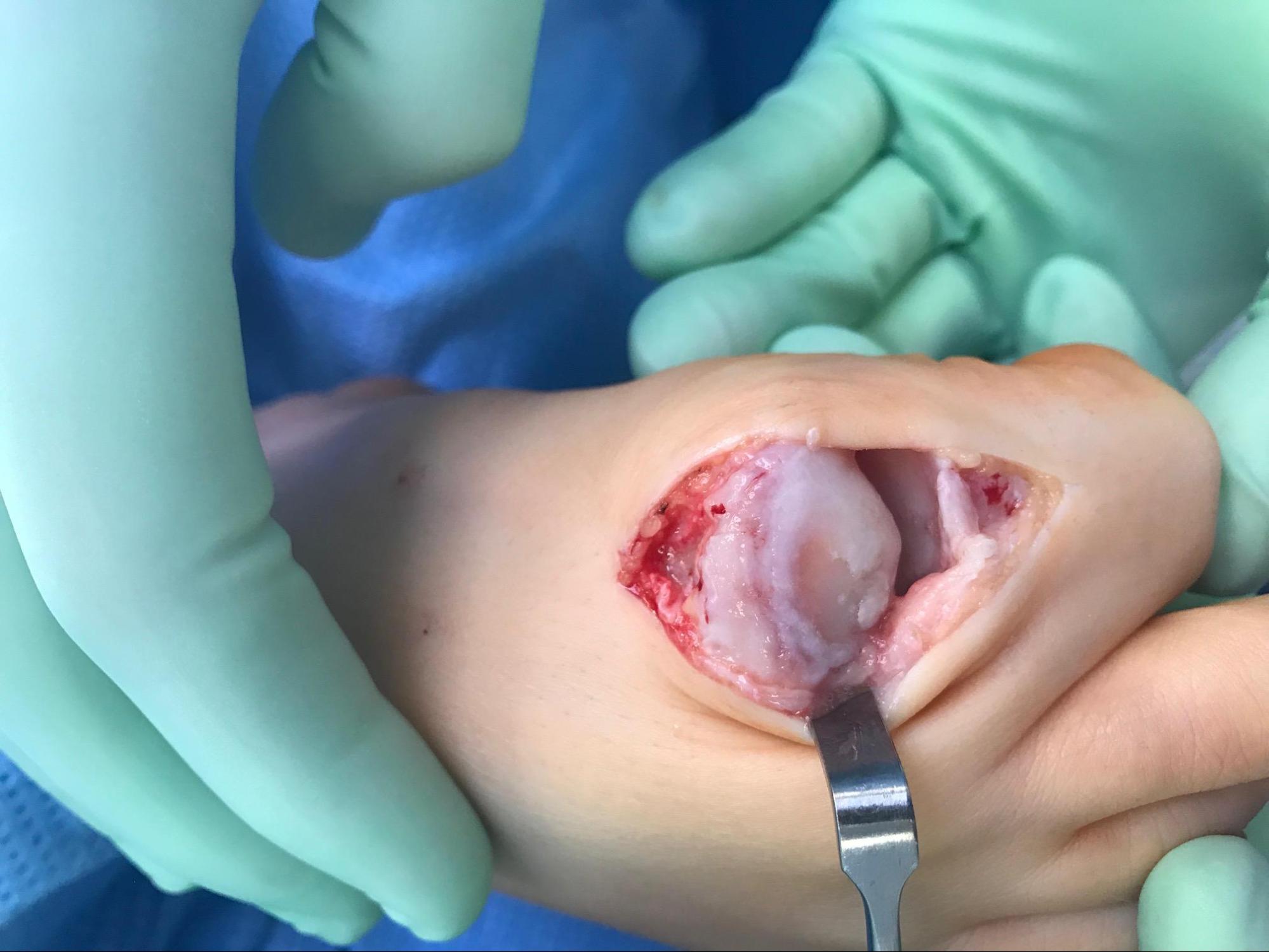
![Gout, [SATA]](/pictures/getimagecontent//6491)