Introduction
The pelvis joints include the pubic symphysis and the lumbosacral, sacroiliac, and sacrococcygeal joints. The bony pelvis also articulates with the lower limb via the acetabulofemoral, or hip, joint on its lateral aspect. The lumbosacral joints include multiple articulations of the fifth lumbar vertebra (L5) and the first sacral element (S1). There is an intervertebral (IV) joint between the vertebral bodies of the fifth lumbar vertebra and the first sacral vertebra with an interposed intervertebral disc. In addition, there are two articular, or zygapophyseal, joints serving as an articulation between the L5 and S1 articular processes. The sacroiliac joint is a bilateral compound joint, with synovial and syndesmotic portions, that serves as an articulation between the auricular surfaces of the ilium and sacrum and their tuberosities. This joint transmits a significant amount of the weight of the upper extremities and torso to the lower limbs, which serves to explain the unusually restricted mobility of this partly synovial joint.
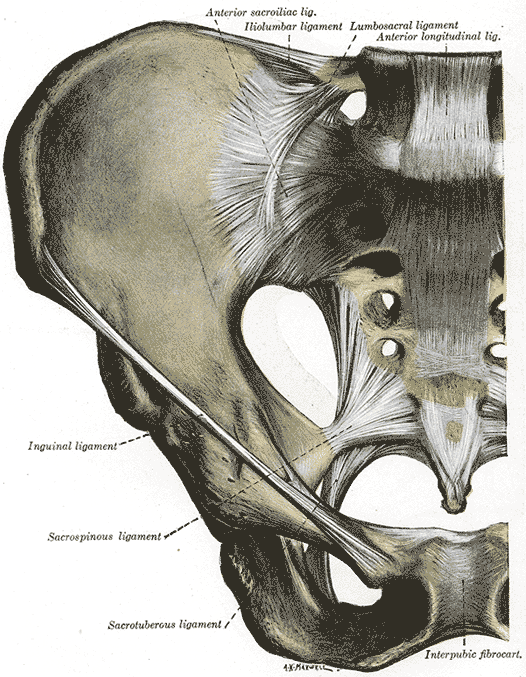
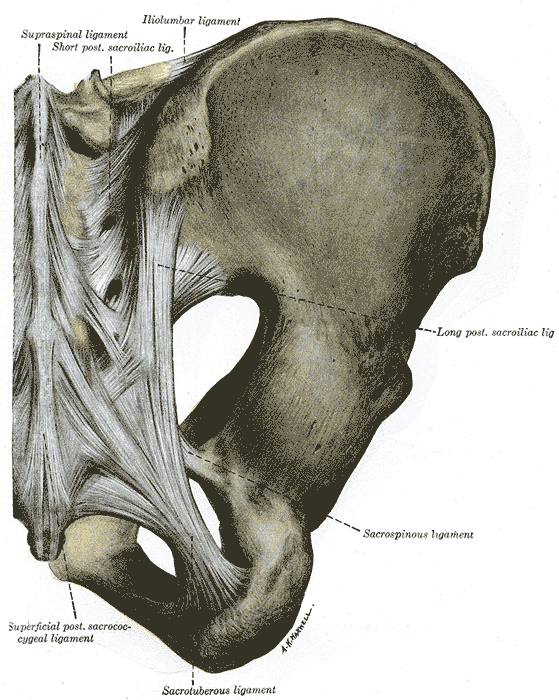
The sacrococcygeal joint is an articulation between the fifth sacral element (S5) of the sacrum, the first coccygeal vertebra (Co1) of the coccyx, and the intervertebral disc between them. Finally, the pubic symphysis is an anteroinferior and midsagittal fibrocartilaginous pelvic joint serving as the articulation for the right and left pubic bodies. The pubic symphysis is covered in hyaline cartilage and is somewhat moveable. The pelvic joints are variable in their degree of movement and contribute to the transmission of forces through the pelvic girdle and the lower limbs. The pelvic joints are reinforced by several ligaments, some of which include the sacrotuberous, sacrospinous, and iliolumbar ligaments. The ligaments supporting the pubic symphysis are flexible and further relaxed during pregnancy due to an increase in relaxin and other hormones. Understanding the basic anatomy of the pelvic joints and ligaments has significance in obstetrics, orthopedics, sports medicine, emergency medicine, and numerous other clinical fields.
Structure and Function
The pelvic girdle is a bony ring comprised of several elements that ultimately form the hip bones and sacrum. The single sacrum is formed from five once-separate sacral vertebrae that typically fuse in adolescence or adulthood. The paired hip bones, also known as the os coxae or innominate, are composed of three once-independent bones that fuse later in life: the ilium, ischium, and pubis. Each hip bone has an articulation with the sacrum, the femur, and the contralateral side. The hip bones serve to resist biomechanical forces in sitting and standing, serve as a muscle attachment site for muscles of the trunk and lower limb, transfer weight between the axial and inferior appendicular skeleton, and protect and support the abdominal and pelvic viscera.
The structure of the pelvis in both size and shape differs between males and females. Females tend to have a broader pelvic inlet and outlet. Additionally, the height of the ilia, the shape and dimensions of the sacrum, the subpubic angle, the angle of the greater sciatic notch, and several other features of the pelvis are of utility in sex determination in recovered skeletons or forensic studies.[1][2][3][4] The pelvic girdle has several ligamentous attachments, most reinforcing and restricting motion at the various pelvic joints.
Lumbosacral Complex
The most superior of the pelvic joints, the lumbosacral joint, is actually multiple joints, including the L5/S1 intervertebral joint with intervertebral disc and two articular or zygapophyseal joints. Reference to the lumbosacral joints as the lumbosacral junction or lumbosacral complex emphasizes this anatomy. The L5/S1 intervertebral joint, or anterior lumbosacral joint, has similar characteristics to the lumbar vertebral joints, except that it typically has the largest surface area of the intervertebral joints. In this case, the intervertebral joints are important in allowing movements of the vertebral column between the lumbar and sacral spine. The L5/S1 intervertebral joint is reinforced by several ligaments, most notably the anterior and posterior longitudinal ligaments. The two lumbosacral articular facet joints, or zygapophyseal joints, are wider than those along the rest of the spine.
The orientation of the articular process and facets contributing to the L5/S1 articulation allow interlocking and prevent slippage at this site. In particular, the iliolumbar and lateral lumbosacral ligaments reinforce these joints. The lumbosacral complex transmits the weight of the head, torso, and upper limbs to the pelvic girdle. The pelvic girdle then sends those forces to the contralateral side through the ischiopubic rami, which serve as bony struts, to the femur when standing, and to the ischial tuberosities when seated. The ligamenta flava and anterior longitudinal, posterior longitudinal, sacroiliac, iliolumbar, interspinous, intertransverse, and lateral lumbosacral ligaments strengthen the iliolumbar complex. The iliolumbar ligament, in particular, is the most important in restricting lumbosacral joint motion.
Sacroiliac Joint
The right and left sacroiliac joints, or SI joints, are articulations between the auricular surfaces of the sacrum and ilium and their tuberosities. The sacroiliac joints are particularly strong joints with significant ligamentous reinforcement to withstand their role in weight-bearing. Together, they support and inferiorly transmit the weight of the torso, upper limbs, and head. The joints are unusual in their morphology because they are compound synovial and syndesmotic joints. The articular surface of the sacroiliac joint is divided into an anterior and posterior portion. The anterior part of the sacroiliac joint is a synovial joint that serves as the articulation between the hyaline cartilage-lined auricular surfaces of the ilium and sacrum.
The articular joint surfaces are somewhat crescentic, with flattened but irregular surfaces that are congruent to limit mobility and increase the strength and stability of the joint. The posterior portion of the sacroiliac joint is a fibrous joint that serves as the syndesmotic articulation between the tuberosities of the sacrum and ilium.[5] The sacroiliac joint is reinforced by several ligaments. The anterior sacroiliac ligament is a thin, weak ligament that is a thickening of the anterior aspect of the sacroiliac joint's fibrous capsule, with multiple delicate extensions between the superior anterolateral sacrum, preauricular sulcus, and ilium.
The posterior sacroiliac ligament is a strong ligament on the posterior aspect of the sacroiliac joint that tightly binds the two bones. It has multiple fibrous extensions extending between the first and second sacral tubercles and the iliac tuberosity, the third sacral tubercle, and the posterior superior iliac spine (PSIS). Part of the posterior sacroiliac ligament is continuous with the sacrotuberous ligament that extends from the posterolateral sacrum and coccyx to the ischial tuberosity. The interosseus sacroiliac ligament is part of the same fibrous tissue as the posterior sacroiliac ligament. The interosseus sacroiliac ligament is a strong and extensive ligament attaching to the sacral and iliac tuberosities that helps to hold the sacrum and ilium together and supports the joint in weight-bearing. The posterior sacroiliac and interosseus sacroiliac ligaments work in concert with the iliolumbar ligament to assist the tight articulation of the sacroiliac joint.
Sacrococcygeal Joint
The fifth sacral element and the base of the coccyx articulate at the sacrococcygeal joint. It is a symphysis or secondary cartilaginous joint with hyaline cartilage and a fibrous disc. There is little motion across this joint, which is reinforced by the anterior and posterior sacrococcygeal ligaments, which are elongated ligaments extending across the sacrum and coccyx.
Pubic symphysis
Each hemipelvis meets anteriorly at the pubic symphysis along the anterior aspect of the pelvis and in the midsagittal plane. The pubic symphysis is a secondary cartilaginous joint, syndesmosis, or amphiarthrosis with an interposed fibrocartilaginous disc. This interpubic disc is slightly moveable and tends to be broader and thicker in females. The ligaments of the pubic symphysis that strengthen and limit movements of the joint are the superior pubic ligament, inferior pubic ligament, anterior pubic ligament, and posterior pubic ligament. These ligaments extend across the relevant borders of the pubic bodies and connect them to the interposed disc and contralateral bone. The moveability of the pubic bones at the pubic symphysis increases in women during pregnancy due to hormones, such as relaxin.
Embryology
The development of the human pelvis is a complex process involving the formation of multiple separate bony elements that fuse relatively late in development. Any errors in the lengthy process or intricate developmental events and their sequence may result in bony malformation. Much like the rest of the skeletal system, the bony pelvis follows a basic developmental plan proceeding through the formation of an initial structure of primordial mesenchyme that converts into cartilage via chondrification and gradually forms bone via primary and secondary ossification.[1]
Primary ossification centers, the sites where bone formation first occurs, typically appear in utero but may continue their development postnatally. Secondary ossification centers form after the development of primary centers and tend to appear postnatally and into adolescence. The pelvic joints form from mesenchyme and are associated with developing their surrounding bony elements.
The sacrum develops as part of the axial skeleton, while the hip bones or os coxae develop as proximal portions of the lower limb. The sacroiliac joint forms at the junction of the axial and appendicular skeleton, while the lumbosacral and sacrococcygeal joints participate in the axial skeleton. The axial skeleton develops from somites first emerging near the skull around 20 days post-fertilization, with three to four subdivisions growing each day to ultimately form the entire vertebral column. By approximately day 29, the five sacral somites typically appear, followed by the coccygeal somites. Chondrification of these structures begins in the sixth or seventh week of development, with the formation of hyaline cartilage bone models visible in radiologic studies.
Meanwhile, the appendicular skeletal elements first appear around 28 days post-fertilization. Chondrification centers of the ilium, ischium, and pubis appear within nine weeks but develop rapidly. They first appear in the pubis and ischium during week 6. By the eighth week, a shallow cartilaginous acetabulum and primordial pubic symphysis are visible. By ten weeks, primary ossification centers can be seen at the iliac crest, and the sacrum and ilium begin to fuse, thus forming the sacroiliac joint.[1] As subsequent primary and secondary ossification occurs, the form of the bony elements changes somewhat dramatically, and the completion of this process may continue well into adulthood.
Blood Supply and Lymphatics
The blood supply to the pelvis and pelvic joints originates from the descending aorta. The aorta bifurcates into the common iliac arteries at approximately the level of the umbilicus. The common iliac arteries bifurcate at the pelvic brim into the internal and external iliac arteries. The external iliac exits the pelvis through the inguinal ligament, which becomes the femoral artery supplying the lower extremity. The internal iliac artery splits into two major divisions, the anterior and posterior divisions of the internal iliac artery, which supply the pelvic organs, perineum, gluteal muscles, and nearby structures.
The anterior division further divides into several branches that vary significantly, partly due to differences in male and female reproductive anatomy. Anterior division arteries often include the umbilical, uterine (in females), superior vesicular, vaginal (in females), inferior vesicular (in males, variable in females), obturator, middle rectal, inferior gluteal, and internal pudendal arteries. These arteries supply pelvic organs, such as the bladder, prostate, uterus, vaginal canal, and seminal glands, as well as the pelvic floor, femoral head, and ilium. The posterior division of the internal iliac artery includes fewer branches, including the iliolumbar, lateral sacral, and superior gluteal arteries. The median sacral artery is an additional nearby vessel that arises from the bifurcation of the abdominal aorta.
The pelvic joints are served by the nearby arteries with considerable anatomic variation in this region. The bony portion of the lumbosacral joint is supplied by the iliolumbar, lateral sacral, and median sacral arteries. The lumbosacral intervertebral disc is avascular and served by diffusion from the adjacent vertebrae. Given its large territory, the sacroiliac joint is supplied by several vessels, including the iliolumbar, superior gluteal, and lateral sacral arteries. The sacrococcygeal joint receives its blood supply from lateral and median sacral arteries. The pubic symphysis is primarily supplied by the inferior epigastric, obturator, and deep external pudendal arteries.
The pelvis contains several groups of lymph nodes, including the internal, external, and common iliac lymph nodes. Additionally, they include the sacral, pararectal, lumbar, and inguinal nodes. There is an extensive network between the groups of lymph nodes; however, the nodes trace the venous system back to the common iliac veins and superiorly drain towards the cisterna chyli before traversing the thoracic duct. Extensive communication through rich lymphatic channels exacerbates the spread of cancer between the abdominal and pelvic organs.[6]
Nerves
The pelvic structures are richly innervated by large nervous plexuses in the region. The pelvic splanchnic nerves supply the parasympathetic innervation of pelvic structures, while the sympathetic innervation of pelvic structures is served by the hypogastric plexus. The sympathetic innervation of the pelvic organs arises from the superior hypogastric plexus as well as the inferior hypogastric plexus. However, the inferior hypogastric plexus carries both sympathetic and parasympathetic fibers. Parasympathetic output causes gastrointestinal peristalsis, contraction of muscles for defecation and urination, as well as erectile function. The sympathetic output is largely antagonistic to parasympathetic output in the pelvis but is also responsible for muscle contraction during orgasm.[6]
Somatomotor and somatosensory innervation arise from two major plexuses, the sacral and coccygeal plexuses. The sacral plexus arises from L4 to S4 spinal nerves and includes the longest nerve in the body, the sciatic nerve. The sciatic nerve is composed of nervous fibers arising from the L4 to S3 nerve roots and innervates the entire skin and most of the leg and foot muscles. The sacral plexus also gives rise to the pudendal nerve, superior and inferior gluteal nerves, and the nerves to the quadratus femoris, piriformis, and obturator internus. Pelvic parasympathetic innervation arises from the pelvic splanchnic nerves served by the S2 to S4 spinal roots. The coccygeal plexus arises from S4, S5, and coccygeal nerves and are responsible for the innervation of the coccygeus and levator ani muscles of the pelvic floor.
The somatic innervation of the pelvic joints varies by region. The ventral and dorsal rami of the L5 and S1 spinal nerves supply the lumbosacral joint. The sacroiliac joint has variation in its innervation, but it is typically served by the ventral rami of L4 and L5 spinal nerves, the dorsal rami of L5-S2 spinal nerves, and the superior gluteal nerve. The sacrococcygeal joint is innervated by S4 and Co1 spinal nerves. The innervation of the public symphysis appears to be highly variable, with numerous reports of nervous contributions from the iliohypogastric, ilioinguinal, genitofemoral, and pudendal nerves.
Muscles
The pelvic girdle contributes to several essential functions, especially in locomotion, despite being composed of relatively fixed joints. Several muscles originate from pelvic attachments on the external and internal surfaces of the pelvic girdle. The muscles originating from the external pelvic girdle assist primarily with locomotion, with attachments along the femur and femoral head within the acetabulum. Additionally, these muscles are crucial for stability and proprioception. The internal surfaces of the pelvic girdle serve as attachments for muscles forming the pelvic “floor.” The pelvic floor muscles support the pelvic viscera by supplying structural integrity, preventing prolapse, and contributing to the control of the anal sphincter, urinary sphincter, and vaginal canal.
The pelvic musculature subdivides into three major categories; muscles that cross the lumbosacral joint, hip joint muscles, and muscles located wholly within the pelvis that form the pelvic floor. Pelvic muscles that cross the lumbosacral joint attach the pelvis to the trunk. These muscles assist with the sacral and lumbar spine in flexion and extension and the lumbar spine in rotation and lateral flexion. Lumbosacral flexion is performed with contraction of the rectus abdominis anteriorly as well as the external and internal oblique muscles. The psoas major is believed to also play an accessory role in flexion. Extension occurs with contraction of the erector spinae muscle group, consisting of the iliocostalis, longissimus, and spinalis muscles, and assisted by the multifidus muscles.
Pelvic muscles that cross the hip joint are also divisible at the hip into general territories; the hip flexors are in an anterior location, the hip extensors are posterior, the adductors are medial, and the abductors are lateral. These groups derive their names from their major actions, i.e., the hip flexors assist with flexion; however, this is an oversimplification as many of the muscles contribute to more than one motion. The hip flexors are the psoas major, iliacus, sartorius, pectineus and rectus femoris. The hip extensors are the gluteus maximus and hamstrings (long head of biceps femoris, semimembranosus, and semitendinosus). The adductor longus, adductor brevis, adductor magnus, gracilis, and pectineus comprise the adductor group. The tensor fascia lata (TFL), gluteus minimus, and gluteus medius are hip abductors.
Finally, the pelvic floor muscles consist of thin layers. The pelvic floor muscles are located entirely within the pelvis and therefore do not move the pelvis. Instead, these muscles stabilize the sacroiliac joint as well as the pubic symphysis, in addition to creating a stable floor for pelvic viscera.[6]
Physiologic Variants
Lumbosacral transitional vertebrae (LSTV) is an increasingly recognized anatomic variant of the lumbosacral joint associated with altered patterns of degenerative changes in up to 35% of the general population. LSTV is considered a congenital spinal anomaly along a morphological spectrum from partial to complete L5 sacralization and partial to complete S1 lumbarization. Sacralization is where the transverse process of the fifth lumbar vertebra fuses to varying extents with the first segment of the sacrum. Complete sacralization of L5 results in only four apparent lumbar vertebrae, with the fifth incorporated into the sacrum.
Lumbarization, in contrast, is when S1 separates from the sacrum to some degree. Complete lumbarization involves a separate S1 segment that appears as a sixth lumbar vertebra. Both have clinical consequences in terms of potential symptoms and surgical considerations. In sacralization, the height of the pars interarticularis and widths of the laminae are smaller, predisposing the patient to spondylolysis and spondylolisthesis. In lumbarization of S1, facets are smaller and often asymmetric, predisposing to accessory joints and may cause low back pain. Additionally, researchers have observed a protective effect of transitional vertebrae in which they mimic outcomes post-fusion operation.[7]
Six variants of the sacroiliac joints have been observed: accessory joints, an iliosacral complex, bipartite iliac bony plate, crescent-like iliac bony plate, semicircular defects at the sacral or iliac side, and ossification centers.
Accessory sacroiliac joint: The accessory sacroiliac joint is found medial to the posterior superior iliac spine and lateral to the second sacral foramen, among a rudimentary transverse tuberosity. On CT imaging, accessory joints have articular surfaces that resemble osseous projects from the ilium to the sacrum. An accessory joint can be present at birth; however, they more commonly result from weight-bearing stress. Accessory joints are more commonly present in the obese and older populations, as well as a higher prevalence in women with three or more childbirths compared to 2 or fewer. Patients may present with low back pain in conjunction with degenerative changes identified on radiologic imaging, such as subchondral sclerosis, osteophytes, and ankyloses on articular surfaces.
Iliosacral complex: Iliosacral complex forms from a projection from the ilium articulating with a complementary sacral recess. These complexes can be unilateral or bilateral, and like accessory joints, these complexes exist at the posterior sacroiliac joint from the level of the first to the second sacral foramen. This variant has been seen more in older patients greater than 60 years, as well as women who are obese more so than women of healthy weight.
Bipartite iliac bony plate: Bipartite iliac bony plate is located at the posterior portion of the sacroiliac joint and appears as described, consisting of two parts and appears unilaterally.
Semicircular defects on the iliac/sacral side: The fourth variant is semicircular defects on either the sacral or iliac aspects of the articular surface of the sacroiliac joint. These can be unilateral or bilateral and, again, are present at the posterior portion of the sacroiliac joint from the level of the first to the second sacral foramen. This defect has been observed more in women than men and in patients older than 60 years.
Crescent-like iliac bony plate: The fifth variant is a crescent-like articular surface which may be present unilaterally or bilaterally. CT imaging demonstrates a crescent-like iliac plate with an accompanying bulged sacral surface. This defect is usually found at the posterior portion of the sacral iliac joint, spanning the first and second sacral foramen levels. This defect was observed only in women and, more commonly, in patients greater than 60 years old.
Ossification centers of the sacral wings: The sixth anatomical variant observed is ossification centers presenting as triangular osseous bodies located within the joint space at the anterior portion of the sacroiliac joint. This defect is found at the level of the first sacral foramen, typically unilaterally.[8][9]
Surgical Considerations
Surgeons operating on the lumbosacral joint have several approaches from which to choose and must consider the goals of the procedure versus the risks of complications and contraindications to specific approaches. Approaches to access the lumbar spine include posterior, transforaminal, minimally invasive transforaminal, lateral, oblique, and anterior approaches. Some approaches are preferable for certain lumbar fusion levels over others. Additionally, successful fusion rates associated with restoration of disc height, segmental lordosis, and total lumbar lordosis vary with the approach. Risks of complications such as dural injury, blood vessel injury, or muscular injury also differ.[10]
Surgeons operating in proximity to the pelvis must consider numerous potential anatomic surgical or postoperative complications. The surgeon must consider the anatomy of the gastrointestinal tract, urinary tract, nerves, blood vessels, and reproductive organs, particularly in females. Additionally, considerations regarding risks of infection, hemorrhage, and thromboembolism are critical. The risk of these complications depends upon the surgical approach and co-morbidities of the individual patient.
Serious urinary tract complications may occur, and the ureters are most often involved. There are several important locations along the course of the ureter to be considered: (1) pelvic brim, (2) base of the broad ligament, and (3) ureterovesical junction. What is possibly most important to the orthopedic or trauma surgeon operating on the pelvis or its related joints is the ureter at the pelvic brim. At this location, the ureter courses over the external iliac artery and accompanying vein approximately 1 cm lateral to the origin of the hypogastric artery. The hypogastric artery may be the single most crucial vessel to identify and avoid mistaking for the ureter.
Anatomical complications involving the small and large intestines or appendix are usually incidental. However, intestinal involvement in neoplasm, pelvic inflammatory disease, endometriosis, or congenital anomalies increases the risk. Often the bowel is prepared pre-operatively in anticipation of these potential complications.[11]
Clinical Significance
The pelvic joints can potentially develop arthritis, malignancy, trauma, fracture, dislocation, inflammatory conditions, and pregnancy symptoms. One prevalent complaint is pelvic joint pain. For instance, the lumbosacral joint is prone to injury due to herniation of the L5/S1 intervertebral joint, fracture, trauma, or degenerative changes. The lumbosacral joint can be a source of pain, mainly due to the ligaments that cover it. If deformed by an alteration of the morphology and articular biomechanics, the latter can send pain signals, especially for movements such as extension and ipsilateral bending.[12] The pubic symphysis is also a source of potential pain due to misalignment or laxity and nerve irritation, often occurring during pregnancy. The painful afferent signals in pubic symphysis pain can derive from the pudendal and genitofemoral nerves and/or branches of the iliohypogastric and ilioinguinal nerves.[13] The sacrococcygeal joint is responsible for back pain in about 40% of all cases. The pain comes from the nociceptors connected to S1 to S3 and L4 to L5.[14]
The sacroiliac joint can be a source of pain that explains about 15% to 30% of all causes of back pain. The sacroiliac joint is a significant source of pelvic joint pain due to inflammation or sacroiliitis. The nerve fibers carrying are via L4 to L5 or L5 to S4 spinal nerves.[15][16] The pain of sacroiliitis may be debilitating, and it typically worsens with ambulation. The pain may result from joint laxity and can be a referred pain (muscular, visceral, or nerve entrapment). Sacroiliac pain may be felt in the buttocks, lower back, posterior thigh, hip, or groin. It may also correlate with paresthesias and urinary retention, frequency, or urgency. Women typically report worsening of this pain during menstruation. Most patients are not able to find a comfortable position causing potential anxiety or depression. The diagnosis of sacroiliitis is not easy because the pelvis contains many structures which can also present with similar symptoms.
The pelvis is also rich with many large nerves, which, if compressed or irritated, can lead to radicular pain. Neither a CT scan nor MRI is sensitive enough to identify disorders causing pain in the pelvis. Some experts recommend a PET scan, but this imaging study is not always available and tends to be prohibitively expensive. Diagnosing many pelvic joint disorders means ruling out other pathologies and using clinical judgment. Treatment may include rest, NSAIDs, exercise, ice or heat, surgical repair, or nerve blocks. Unfortunately, many patients remain dissatisfied with treatment.