Continuing Education Activity
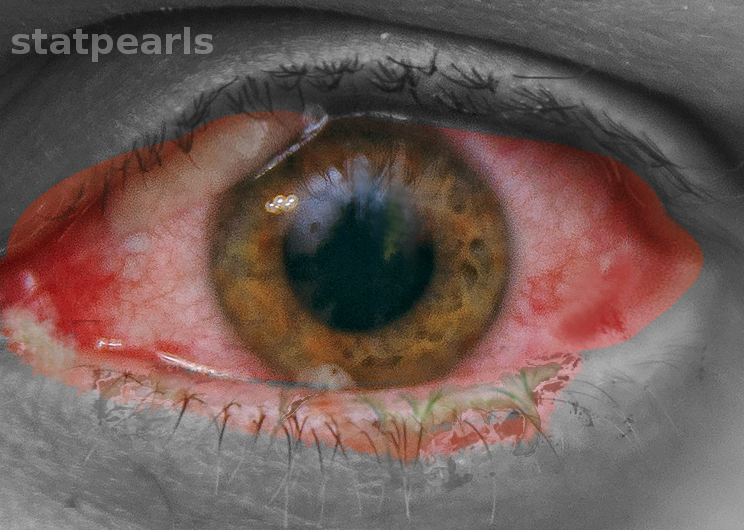
Conjunctivitis, also informally known as "pink eye," makes up the majority of ophthalmologic disorders seen at primary care clinics. Patients present complaining of eye redness, which may or may not be accompanied by pain, itching, and discharge. Dilation of conjunctival blood vessels secondary to viral or bacterial infection, chemical exposures, or allergies results in the redness seen on the examination. While viral and allergic conjunctivitis occurs more frequently, bacterial conjunctivitis is responsible for increased morbidity and provides a more challenging clinical scenario for physicians. This activity reviews the evaluation and treatment of bacterial conjunctivitis and explains the role of the healthcare team in managing patients with this condition.
Objectives:
- Review the etiology of bacterial conjunctivitis.
- Summarize the appropriate history and physical exam findings of bacterial conjunctivitis.
- Describe the treatment and management options available for bacterial conjunctivitis.
- Explain the importance of communication among the inter-professional team concerning the initiation of antibiotic therapy and identify ways to affect the growing problem of microbial resistance positively.
Introduction
Conjunctivitis, also informally known as "pink eye," makes up the majority of ophthalmologic disorders seen at primary care clinics. Patients present complaining of eye redness, which may or may not be accompanied by pain, itching, and discharge. Dilation of conjunctival blood vessels secondary to viral or bacterial infection, chemical exposures, or allergies results in the redness seen on the examination.[1] While viral and allergic conjunctivitis occurs more frequently, bacterial conjunctivitis is responsible for increased morbidity and provides a more challenging clinical scenario for physicians.[2][3]
Etiology
Patterns of spread for bacterial conjunctivitis include hand to eye, eye contact with fomite, and person to person through respiratory droplets.[4] The most common causative organism of bacterial conjunctivitis in children is Haemophilus influenzae, followed by Streptococcus pneumoniae and Moraxella catarrhalis.[5][6][7] Bacterial pathogens in adults are more often staphylococcal species with Haemophilus influenzae and Streptococcus pneumoniae responsible for a smaller percentage of cases.[2] Staphylococcus aureus is more commonly found in adults and the elderly but is also present in pediatric cases of bacterial conjunctivitis.[4] There has also been an increase in the frequency of conjunctivitis secondary to methicillin-resistant Staphylococcus aureus (MRSA).[2] Contact lens wearers are more susceptible to gram-negative infections.[4] Pseudomonas aeruginosa is more likely to be the isolate from critically ill, hospitalized patients.[4] Neonates can be affected by the vertical, oculogenital transmission of Neisseria gonorrhoeae and Chlamydia trachomatis resulting in acute bacterial conjunctivitis.[1] These organisms can also cause a hyperacute infection in sexually active adolescents and adults.[1]
Epidemiology
Acute conjunctivitis of all causes is estimated to occur in 6 million individuals annually in the United States.[8] Encounters for red eyes account for one to four percent of general practitioner visits in the developed world with acute bacterial conjunctivitis the most commonly diagnosed.[4] A peak occurrence of bacterial conjunctivitis reportedly runs from December to April.[4] Conjunctivitis of bacterial etiology is the second most commonly occurring infectious cause and affects children with increased frequency.[2] A 1981 study determined that in approximately 54 percent of pediatric acute, infectious conjunctivitis cases, bacteria were the responsible pathogen.[3] In 2017, a survey of 3000 children with acute conjunctivitis reported that only ten percent of cases were attributable to bacteria.[8] Both studies concurred that physicians' empiric treatment of conjunctivitis resulted in significantly higher rates of antibiotic administration than may be necessary.[3][8]
Pathophysiology
Direct transmission of pathogens onto the conjunctiva leads to infectious conjunctivitis. Conjunctivitis can occur when the epithelial layer of the eye is compromised, or there is disruption in overall defense mechanisms. An immunocompromised state may also predispose to bacterial conjunctivitis.[2]
History and Physical
Patients with bacterial conjunctivitis often present complaining of redness, tearing, and discharge from one or both eyes.[1] The clinician should question patients about the duration of symptoms as the disease course can be divided into hyperacute, acute (less than 3 to 4 weeks), and chronic (greater than four weeks).[4] Associated pain, itching, vision loss, and photophobia also contribute to clinical decision making.[1] A comprehensive history should also include the occurrence of trauma, previous similar episodes, any prior treatment, contact lens use, immune status, and sexual history.[1] Any otic symptoms should also be elucidated as children with bacterial conjunctivitis can have concurrent otitis media.[6]
Certain clinical features can indicate a bacterial origin to conjunctivitis; however, findings are often variable, and there is cross-over between conjunctivitis symptoms of different etiologies.[2] Clinically distinguishing bacterial conjunctivitis from other forms is essential as it can help direct therapies and potentially curb unnecessary empiric antibiotic administration. Traditionally, a purulent or mucopurulent discharge has been associated with the diagnosis of bacterial conjunctivitis while watery discharge has been more consistent with viral or allergic conjunctivitis.[2] A 2003 study contested this assertion based on a lack of evidence to support discharge characteristics correlating with the cause of conjunctivitis.[2][9] A later study by the same authors concluded that three findings were significantly predictive of bacterial conjunctivitis, including glued eyes, lack of itching, and no previous history of conjunctivitis.[2][9] A 2006 prospective study of children with conjunctivitis described five clinical history and physical examination variables associated with bacterial culture-positive infections. These included a history of gluey or sticky eyelids in the morning, examination findings of mucoid or purulent discharge, eyelids or eyelashes crusting or gluing on examination, absence of burning sensation, and lack of watery discharge.[4] The inconsistencies of these findings concerning discharge as a predictor of bacterial infection might be attributable to the 2003 survey focusing on history, while the 2006 study included in-office physical examination findings. These differences reinforce the idea of variability in the presentation of bacterial conjunctivitis.
Classic physical examination findings of bacterial conjunctivitis are conjunctival erythema and purulent discharge.[1] A complete ocular examination should include assessment of visual acuity and corneal involvement.[2][3] Although slit lamps are beneficial to a comprehensive physical assessment, they are not routinely available in primary care offices.[2] An otoscopic examination is warranted If ear symptoms are reported in children to diagnose concurrent acute otitis media.[6]
Evaluation
Laboratory and radiographic testing have limited application in the diagnosis and evaluation of bacterial conjunctivitis. However, conjunctival cultures are the recommended course in cases where ophthalmia neonatorum is suspected, or where copious purulent discharge makes the diagnosis of gonococcal or chlamydial infection more likely.[1][2] Cultures may also be obtained in the event of recurrent conjunctivitis or in cases where therapy has failed.[2]
Treatment / Management
Management of acute bacterial conjunctivitis centers around the decision to initiate antimicrobials based on the physician's clinical assessment and with the consideration of benefits of treatment, the natural course of the disease if left untreated, antibiotic resistance, and the philosophy of antibiotic stewardship. Several clinical features make the diagnosis of bacterial conjunctivitis more likely; however, the presentation remains variable. Distinguishing bacterial conjunctivitis from other etiologies can be difficult, and practitioners often err on the side of empiric antibiotic therapy.[3] Studies have indicated that around 50 percent of pediatric infectious conjunctivitis presentations are attributed to bacteria, while physicians prescribe antibiotics in up to 80 to 95 percent of these cases.[3][10] Ophthalmologists utilize antimicrobial therapy in a smaller percentage of cases than general practitioners.[3][10] Treatment with topical antibiotics has demonstrated a decrease in symptoms, improved resolution times, decreased transmission, and hastened return to school or work.[2][3][6][7]
The natural course of untreated bacterial conjunctivitis is the resolution of the infection within one week.[4] Another consideration is the continued resistance patterns of ocular, bacterial pathogens.[6] With an understanding of the described management variables, uncomplicated bacterial conjunctivitis can be treated empirically with topical antibiotics, or managed expectantly without antimicrobials.[2] In complicated cases involving patients with immunocompromise, contact lens use, and suspected gonococcal or chlamydial infections, antibiotic therapy should be provided.[2] If the decision is made to initiate empiric treatment, the antibiotic chosen should be broad-spectrum and include coverage of gram-positive and gram-negative ocular bacteria.[6] Topical aminoglycosides, polymyxin B combination drugs, macrolides, and fluoroquinolones are the most commonly prescribed ophthalmic agents.[2][6][8] The duration of treatment is generally five to seven days.[6]
Recently, data has shown recorded emerging resistance to most classes of these drugs.[6] Topical erythromycin has been a therapeutic choice for years; however, microbial resistance and unsatisfactory coverage for Haemophilus influenzae have limited its usefulness. Topical polymyxin B/trimethoprim and several fluoroquinolones effectively manage most cases of acute bacterial conjunctivitis.[1][6] Newer fluoroquinolones have the least documented resistance; however, they are costly.[6] They should be considerations in areas of increased local antibiotic resistance.[1][8] Bacterial conjunctivitis secondary to gonococcal or chlamydial infections requires systemic treatment.[2] Oral antibiotics are also indicated in cases of bacterial conjunctivitis with concurrent acute otitis media.[6] Ophthalmia neonatorum secondary to Chlamydia trachomatis requires oral or intravenous erythromycin in addition to topical erythromycin for 14 days.[1][11][12] When gonorrhea is the cause of the newborn infection, hospital admission, a single dose of intravenous or intramuscular ceftriaxone, and eye irrigation are the indicated therapy until resolution of the infection.[2]
Follow up for acute bacterial conjunctivitis should be encouraged if there is no improvement in symptoms after one to two days.[4]
Differential Diagnosis
The differential diagnosis for bacterial conjunctivitis includes viral and allergic conjunctivitis.[4] Clear discharge and itching are more characteristic of allergies and viral infections.[2][4] Trauma can also present with similar symptoms to conjunctivitis of bacterial origin. Keratitis and iridocyclitis should be ruled out as corneal infections, and iris inflammation can lead to significant morbidity.[4]
Prognosis
The prognosis for uncomplicated bacterial conjunctivitis is good with complete resolution and rare adverse events with both antibiotic treatment and expectant management strategies.[2][6]
Complications
Complications from bacterial conjunctivitis are uncommon; however, severe infections can result in keratitis, corneal ulceration and perforation, and blindness.[2][4][6]
Consultations
Referral to an ophthalmologist is the recommendation in cases of vision loss, non-response to treatment, recurrent infections, corneal involvement, and severe pain or discharge.[2]
Deterrence and Patient Education
Patients should receive education on the signs and symptoms concerning for complications of bacterial conjunctivitis. Contact lens wearers must be instructed to remove lenses until completion of the treatment course and resolution of symptoms. Transmission prevention is essential, with an emphasis on handwashing. Adolescents and adults with gonococcal or chlamydial infection should have counseling on safe sex practices and partner treatment.[1] The education of parents and school administrators can decrease missed school days for children.[3][4] Upon initiation of treatment, pediatric patients may return to regular school activities.[3][4]
Enhancing Healthcare Team Outcomes
Bacterial conjunctivitis provides a common and challenging clinical scenario for practitioners. The variability of presentations makes differentiating bacterial conjunctivitis from other etiologies difficult and has led to the over-prescribing of antibiotics.[2][3] An interprofessional team is highly recommended to improve outcomes. The majority of patients first present to the nurse practitioner or primary care provider, and these clinicians should make appropriate referrals to an ophthalmologist if the diagnosis is in doubt or there is vision loss. At the same time, the primary clinicians should educate patients on hand washing and not sharing personal care items with others during the acute process.
Several studies have sought to define characteristics of conjunctivitis that make a bacterial origin more likely and have proposed these findings to improve the management of the condition.[2][9] Antimicrobial therapy has demonstrated benefits to patients; however, most uncomplicated cases resolve spontaneously without adverse outcomes.[2][3][4] Appropriate management strategies can include antibiotic treatment, as well as reassurance and patient education without antimicrobial use.
Interprofessional consultation with pharmacists, infectious disease specialists, and ophthalmologists may provide information on local antibiotic resistance patterns and guide clinician therapy. The pharmacist should verify agent selection and dosing/duration, perform medication reconciliation to prevent any drug-drug interactions, and deliver patient counseling on the importance of medication compliance, reporting any concerns to the prescribing/order physician. Nursing can evaluate and assist in monitoring patient compliance, treatment progress, and adverse medication reactions on followup visits, or in the case of inpatients, as they administer the medications, and communicate to the prescriber any issues they encounter.
Ophthalmology referral is necessary in complicated cases, and communication with specialists may reinforce the physician's decision to start, or not to start, antibiotic therapy in uncomplicated cases.[1] Evaluating the available data on the diagnosis and management of bacterial conjunctivitis, as well as observing evidence-based practices, can improve patient outcomes and support community health through antibiotic stewardship. [Level II]
Bacterial conjunctivitis requires an interprofessional team approach, including physicians, specialists, specialty-trained nurses, and pharmacists, all collaborating across disciplines to achieve optimal patient results. [Level V]