Introduction
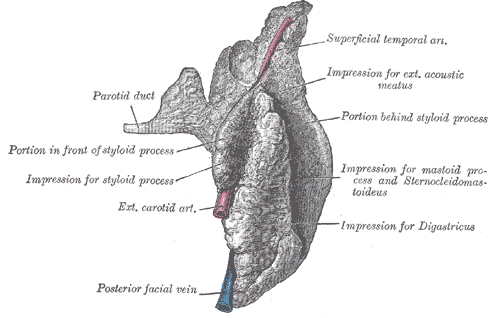
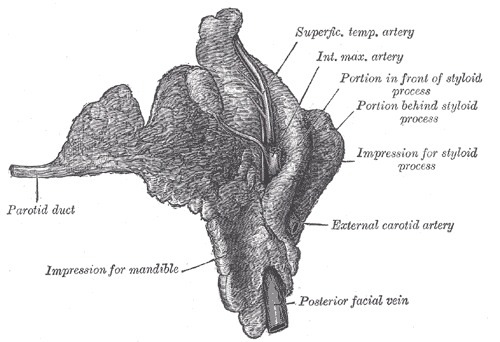
The parotid gland is the largest of the three paired major salivary glands, including the submandibular and sublingual glands. It is located in the retromandibular fossa, space mainly occupied by this gland. It is bordered superiorly by the zygomatic arch, anteriorly by the masseter muscle, and posteriorly by the sternocleidomastoid muscle. However, the superficial lobe extends anteriorly, covering the mandibular ramus and the posterior area of the masseter muscle.[1] See Images. The Mouth, Right Parotid Gland, Posterior and The Mouth, Right Parotid Gland, anterior.
The parotid gland and the other salivary glands play an essential function in the oral cavity because they secret saliva, facilitating chewing, swallowing, speaking, and digesting.[2]
The facial nerve courses through the body of the parotid gland, creating a unique relationship between them, which requires focused attention when performing parotidectomies or other surgery in the region.[3]
Structure and Function
The parotid glands can be palpated anterior and inferior to the lower half of the ear on the lateral surface of the cheek. They extend inferiorly to the lower border of the mandible and superiorly to the zygomatic arch. Each parotid gland comprises a superficial lobe and a deep lobe divided by the facial nerve and the posterior facial vein. Between the lobes of the gland, there is also fatty tissue that facilitates mandibular movements. The superficial lobe lies lateral to the facial nerve and overlies the lateral surface of the masseter muscle. The deep lobe lies medial to the facial nerve and is situated between the mastoid process of the temporal bone and the mandibular ramus. A fascial capsule called the parotid sheath surrounds the parotid glands.[1]
The parotid main excretory duct (Stensen's duct) projects from the anterior portion of the superficial lobe and runs over the masseter muscle until it reaches its anterior border, from where it turns medially to penetrate the buccinator muscle [1]. It opens into the buccal cavity at the level of the buccal mucosa of the maxillary second molar.[1]
The salivary glands share the same histological structure - a secretory portion called acini and a web of arborized ducts that open into the buccal cavity realizing saliva.[2] The parotid is a serous gland composed mainly of serous acinar cells, but it may contain accessory glandular tissue formed by mucinous acinar cells. Therefore, saliva excreted by the parotid is serous and watery. Each serous acinus is surrounded by myoepithelial cells that contract to help expel secretions from the acini. Furthermore, an extracellular matrix, stromal cells, immune cells, myofibroblasts, and nerves are found in the periphery of the acini.[4]
Saliva is first produced in the acinar lumen and then altered into a mixture of electrolytes and macromolecules as it is actively transported through the ducts. The saliva is hypotonic when it reaches the mouth, but salivary flow rates can influence the electrolyte composition. In addition to electrolytes, saliva also contains mucin and digestive enzymes. The most important enzyme is amylase, which initiates the digestion of carbohydrates.[2]
Embryology
The parotid gland starts developing in the 6th week of gestation [2] via a process of proliferation, budding length, and branching. The excretory ducts and acini derive from the ectoderm, whereas the gland's capsule and connective tissue come from the mesenchyme. The intimate relationship with the facial nerve is established from the beginning.[5]
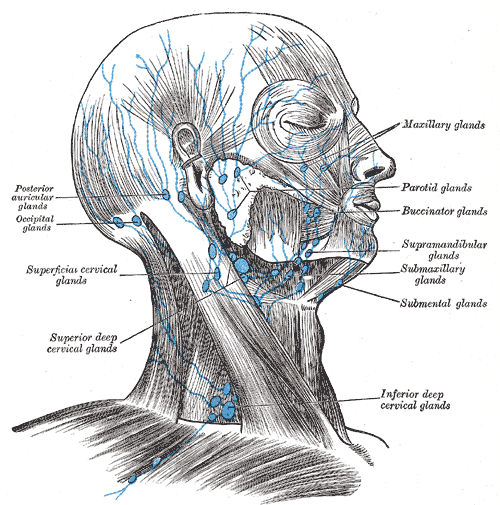
Blood Supply and Lymphatics
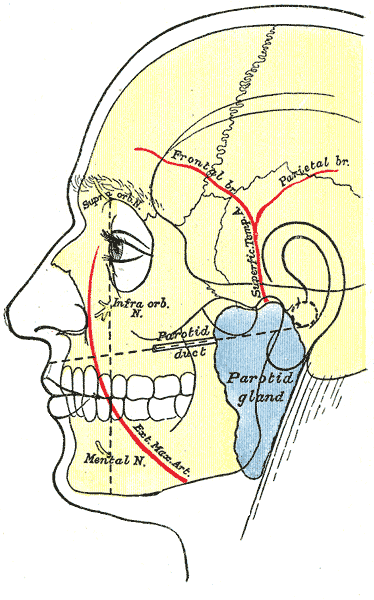
Blood Supply
The external carotid artery provides blood supply to the parotid. It bifurcates into two terminal branches, the superficial temporal artery, and the maxillary artery (see Image. Surface Markings of Special Regions of the Head). The superficial temporal artery gives off the transverse facial artery, which runs anteriorly between the zygoma and parotid duct and supplies the parotid duct, parotid gland, and masseter muscle. The maxillary artery supplies the infratemporal fossa and the pterygopalatine fossa after exiting the medial portion of the parotid.[5] Finally, the retromandibular vein - which forms from the confluence of the superficial temporal and maxillary veins - provides venous outflow for the parotid. It courses deep to the facial nerve, and it may exhibit variable anatomy before joining the external jugular vein.[5]
Lymphatics
The parotid gland is in intimate relation with the lymph nodes (see Image. Lymph Nodes of the Head and Neck). It is the only salivary gland with two nodal layers, which drain into the superficial and deep cervical lymph system. Most nodes are located within the superficial lobe between the gland and the parotid capsule.[2] It is worth noting that skin cancers of the face or scalp can enlarge the lymph nodes in the parotid gland, indicating the regional spread of carcinoma. Lymph nodes located in the parotid substance drain the gland, middle ear, nasopharynx, palate, and external meatus; the superficial preauricular lymph nodes drain the anterior pinna, temporal scalp, eyelids, and lacrimal glands.[5]
Nerves
Sympathetic and parasympathetic fibers innervate the parotid gland. Sympathetic innervation causes vasoconstriction, and parasympathetic innervation, from the glossopharyngeal nerve (CN IX), produces the secretion of saliva.[5] The parasympathetic fibers originate in the inferior salivatory nucleus in the medulla and travel through the jugular foramen to the inferior ganglion. A small branch of the glossopharyngeal nerve, called the tympanic or Jacobsen's nerve, forms the tympanic plexus within the middle ear. These preganglionic fibers become the lesser petrosal nerve and course through the middle cranial fossa before exiting through the foramen ovale. They synapse in the otic ganglion, and the postganglionic parasympathetic fibers join the auriculotemporal nerve to innervate the parotid gland to secrete saliva.
The neurotransmitters acetylcholine (ACh) and norepinephrine (NE) act within the parotid. ACh binds muscarinic receptors to stimulate acinar activity and ductal transport. It also uses second messenger activity, producing inositol triphosphate leading to increased calcium concentration within the cells. As a result, salivary secretion increases. Norepinephrine transmits sympathetic nervous impulses via postganglionic sympathetic fibers to the salivary glands - sympathetic outflow thickens saliva. NE binds beta-adrenergic receptors activating the adenylate cyclase second messenger system, producing cAMP, phosphorylating proteins, and activating enzymes.
The facial nerve courses through the parotid gland, providing motor supply to the muscles of facial expression but does not provide innervation to the gland.
The parotid gland is closely related to two muscles: sternocleidomastoid and masseter. The accessory nerve provides innervation to the sternocleidomastoid muscle,[6] which forms the posterior border of the retromandibular fossa. The superficial lobe of the parotid gland partly covers the mandibular ramus and the posterior part of the masseter muscle. The masseter muscle receives innervation by the masseteric nerve, a branch of the mandibular nerve.[7]
Surgical Considerations
The parotid gland is the location of 80% of salivary tumors.[5] The most common primary parotid tumor is pleomorphic adenoma (see Image. Parotid Mass). The management of neoplasias of the parotid typically includes surgical resection. Because the facial nerve courses through the glandular substance of the parotid gland, identifying this nerve is crucial when performing surgical procedures in the gland to prevent injuries. Some bony and soft tissue landmarks commonly used to identify the facial nerve trunk include the cartilaginous tragal pointer, the tympanomastoid suture, the posterior belly of the digastric muscle, the styloid process, and the retromandibular vein.[3]
If an obstructing stone (sialolithiasis) causes refractory inflammation despite medical treatment, a procedure called sialoendoscopy can be performed for relief. It uses an endoscope to visualize the stone to aiding the management.
Clinical Significance
Sialadenitis
- Sialadenitis is the inflammation of the salivary gland caused by obstruction and infection by bacteria, viruses, or stones.
- Signs and symptoms include pain, swelling of the gland, and fever.
- The most common microorganisms involved in the condition are staphylococcal bacteria and the mumps virus [8]
- Treatment includes antibiotics for bacterial infections, oral hydration, warm compresses, and drugs that induce salivary secretion. For cases of refractory infection, surgical management may be indicated (i.e., abscess drainage) [9]
Sialolithiasis
- Sialolithiasis is a benign condition caused when a stone or calculus is lodged in a salivary duct. It is the most common cause of obstructive salivary gland disease and is responsible for half of all major salivary gland disorders [10]
- Signs and symptoms include pain and swelling in the affected duct, particularly during and after eating [11]
- Ultrasound imaging is the first step in the diagnosis. CT scan, MRI, and MR sialography can be used in patients with a high suspicion for ductal obstruction that had a negative or inconclusive ultrasound study [10]
- The goal of treatment is to increase saliva flow through the duct with oral hydration and drugs that induce salivary secretion. Surgical removal of the calculus is required for chronic sialolithiasis that has failed conservative treatment [12]