[1]
Voskoboinik A, Prabhu S, Ling LH, Kalman JM, Kistler PM. Alcohol and Atrial Fibrillation: A Sobering Review. Journal of the American College of Cardiology. 2016 Dec 13:68(23):2567-2576. doi: 10.1016/j.jacc.2016.08.074. Epub
[PubMed PMID: 27931615]
[2]
Ettinger PO, Wu CF, De La Cruz C Jr, Weisse AB, Ahmed SS, Regan TJ. Arrhythmias and the "Holiday Heart": alcohol-associated cardiac rhythm disorders. American heart journal. 1978 May:95(5):555-62
[PubMed PMID: 636996]
[3]
Thornton JR. Atrial fibrillation in healthy non-alcoholic people after an alcoholic binge. Lancet (London, England). 1984 Nov 3:2(8410):1013-5
[PubMed PMID: 6149396]
[4]
Gallagher C, Hendriks JML, Elliott AD, Wong CX, Rangnekar G, Middeldorp ME, Mahajan R, Lau DH, Sanders P. Alcohol and incident atrial fibrillation - A systematic review and meta-analysis. International journal of cardiology. 2017 Nov 1:246():46-52. doi: 10.1016/j.ijcard.2017.05.133. Epub
[PubMed PMID: 28867013]
Level 1 (high-level) evidence
[5]
Kodama S, Saito K, Tanaka S, Horikawa C, Saito A, Heianza Y, Anasako Y, Nishigaki Y, Yachi Y, Iida KT, Ohashi Y, Yamada N, Sone H. Alcohol consumption and risk of atrial fibrillation: a meta-analysis. Journal of the American College of Cardiology. 2011 Jan 25:57(4):427-36. doi: 10.1016/j.jacc.2010.08.641. Epub
[PubMed PMID: 21251583]
Level 1 (high-level) evidence
[6]
Marcus GM, Vittinghoff E, Whitman IR, Joyce S, Yang V, Nah G, Gerstenfeld EP, Moss JD, Lee RJ, Lee BK, Tseng ZH, Vedantham V, Olgin JE, Scheinman MM, Hsia H, Gladstone R, Fan S, Lee E, Fang C, Ogomori K, Fatch R, Hahn JA. Acute Consumption of Alcohol and Discrete Atrial Fibrillation Events. Annals of internal medicine. 2021 Nov:174(11):1503-1509. doi: 10.7326/M21-0228. Epub 2021 Aug 31
[PubMed PMID: 34461028]
[7]
Lowenstein SR, Gabow PA, Cramer J, Oliva PB, Ratner K. The role of alcohol in new-onset atrial fibrillation. Archives of internal medicine. 1983 Oct:143(10):1882-5
[PubMed PMID: 6625772]
[8]
Hansson A, Madsen-Härdig B, Olsson SB. Arrhythmia-provoking factors and symptoms at the onset of paroxysmal atrial fibrillation: a study based on interviews with 100 patients seeking hospital assistance. BMC cardiovascular disorders. 2004 Aug 3:4():13
[PubMed PMID: 15291967]
Level 3 (low-level) evidence
[9]
Noessler N, Schweintzger S, Kurath-Koller S. Holiday heart syndrome: an upcoming tachyarrhythmia in today's youth? Cardiology in the young. 2021 Jun:31(6):1054-1056. doi: 10.1017/S1047951121000329. Epub 2021 Feb 9
[PubMed PMID: 33557971]
[10]
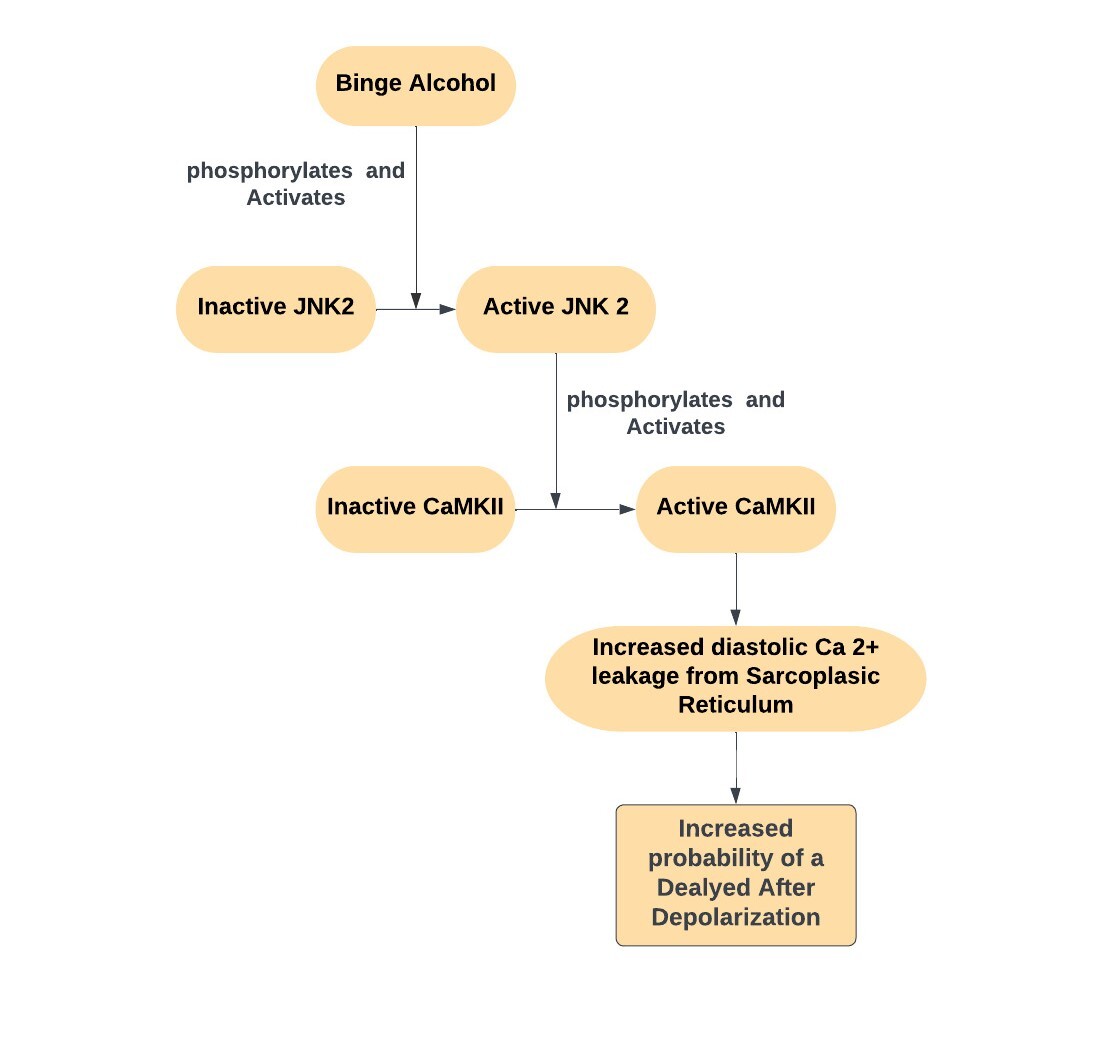
Yan J, Thomson JK, Zhao W, Gao X, Huang F, Chen B, Liang Q, Song LS, Fill M, Ai X. Role of Stress Kinase JNK in Binge Alcohol-Evoked Atrial Arrhythmia. Journal of the American College of Cardiology. 2018 Apr 3:71(13):1459-1470. doi: 10.1016/j.jacc.2018.01.060. Epub
[PubMed PMID: 29598867]
[11]
Staerk L, Sherer JA, Ko D, Benjamin EJ, Helm RH. Atrial Fibrillation: Epidemiology, Pathophysiology, and Clinical Outcomes. Circulation research. 2017 Apr 28:120(9):1501-1517. doi: 10.1161/CIRCRESAHA.117.309732. Epub
[PubMed PMID: 28450367]
Level 2 (mid-level) evidence
[12]
Andrade J, Khairy P, Dobrev D, Nattel S. The clinical profile and pathophysiology of atrial fibrillation: relationships among clinical features, epidemiology, and mechanisms. Circulation research. 2014 Apr 25:114(9):1453-68. doi: 10.1161/CIRCRESAHA.114.303211. Epub
[PubMed PMID: 24763464]
[14]
Marcus GM, Dukes JW, Vittinghoff E, Nah G, Badhwar N, Moss JD, Lee RJ, Lee BK, Tseng ZH, Walters TE, Vedantham V, Gladstone R, Fan S, Lee E, Fang C, Ogomori K, Hue T, Olgin JE, Scheinman MM, Hsia H, Ramchandani VA, Gerstenfeld EP. A Randomized, Double-Blind, Placebo-Controlled Trial of Intravenous Alcohol to Assess Changes in Atrial Electrophysiology. JACC. Clinical electrophysiology. 2021 May:7(5):662-670. doi: 10.1016/j.jacep.2020.11.026. Epub 2021 Jan 27
[PubMed PMID: 33516710]
Level 1 (high-level) evidence
[15]
Ragland G. Electrolyte abnormalities in the alcoholic patient. Emergency medicine clinics of North America. 1990 Nov:8(4):761-73
[PubMed PMID: 2226285]
[16]
Tonelo D, Providência R, Gonçalves L. Holiday heart syndrome revisited after 34 years. Arquivos brasileiros de cardiologia. 2013 Aug:101(2):183-9. doi: 10.5935/abc.20130153. Epub
[PubMed PMID: 24030078]
[17]
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, Ellinor PT, Ezekowitz MD, Field ME, Furie KL, Heidenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. 2019 Jul 9:140(2):e125-e151. doi: 10.1161/CIR.0000000000000665. Epub 2019 Jan 28
[PubMed PMID: 30686041]
Level 1 (high-level) evidence
[18]
Elisaf M, Merkouropoulos M, Tsianos EV, Siamopoulos KC. Pathogenetic mechanisms of hypomagnesemia in alcoholic patients. Journal of trace elements in medicine and biology : organ of the Society for Minerals and Trace Elements (GMS). 1995 Dec:9(4):210-4
[PubMed PMID: 8808192]
[19]
Ballard HS. The hematological complications of alcoholism. Alcohol health and research world. 1997:21(1):42-52
[PubMed PMID: 15706762]
[20]
Piccioni A, Tarli C, Cardone S, Brigida M, D'Addio S, Covino M, Zanza C, Merra G, Ojetti V, Gasbarrini A, Addolorato G, Franceschi F. Role of first aid in the management of acute alcohol intoxication: a narrative review. European review for medical and pharmacological sciences. 2020 Sep:24(17):9121-9128. doi: 10.26355/eurrev_202009_22859. Epub
[PubMed PMID: 32965003]
Level 3 (low-level) evidence
[21]
Knight E, Lappalainen L. Clinical Institute Withdrawal Assessment for Alcohol-Revised might be an unreliable tool in the management of alcohol withdrawal. Canadian family physician Medecin de famille canadien. 2017 Sep:63(9):691-695
[PubMed PMID: 28904034]
[22]
Craig-Brangan KJ, Day MP. Update: 2017/2018 AHA BLS, ACLS, and PALS guidelines. Nursing. 2019 Feb:49(2):46-49. doi: 10.1097/01.NURSE.0000552705.65749.a0. Epub
[PubMed PMID: 30676559]
[23]
Krishnamoorthy S, Lip GY, Lane DA. Alcohol and illicit drug use as precipitants of atrial fibrillation in young adults: a case series and literature review. The American journal of medicine. 2009 Sep:122(9):851-856.e3. doi: 10.1016/j.amjmed.2009.02.012. Epub
[PubMed PMID: 19699381]
Level 2 (mid-level) evidence
[24]
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW, American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology. 2014 Dec 2:64(21):e1-76. doi: 10.1016/j.jacc.2014.03.022. Epub 2014 Mar 28
[PubMed PMID: 24685669]
Level 1 (high-level) evidence
[25]
Ruigómez A, Johansson S, Wallander MA, García Rodríguez LA. Predictors and prognosis of paroxysmal atrial fibrillation in general practice in the UK. BMC cardiovascular disorders. 2005 Jul 11:5():20
[PubMed PMID: 16008832]