Continuing Education Activity
Humerus fractures account for 4 to 6 percent of all fractures in young patients and 1 to 3 percent of all fractures in elderly patients. In young men, these fractures are usually a result of high-energy trauma while in the older population, these fractures are typically seen in women after a ground-level fall. Interestingly, humerus shaft fractures in polytrauma patients are independent predictors of intra-abdominal injury, long bone, and hand fractures. Typically, these injuries cause temporary disability in the younger population whereas permanent disability can be seen in the elderly population. This activity describes the evaluation, diagnosis, and management of humerus fractures and stresses the role of team-based interprofessional care for affected patients.
Objectives:
- Describe the anatomy pertinent to humerus fractures.
- Outline the complications of humerus fractures.
- Summarize the treatment considerations for humerus fractures.
- Explain interprofessional team strategies for enhancing care coordination and communication to advance the evaluation and management of humerus fractures and improve patient outcomes.
Introduction
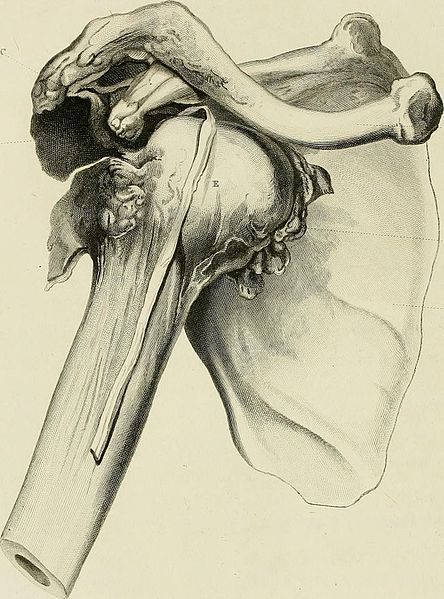
The proximal humerus has two necks. The anatomic neck is the old epiphyseal plate, and the surgical neck is the metaphyseal area below the humeral head. The blood supply is the anterior and posterior humeral circumflex artery with the axillary nerve as the major nerve of this region. The humeral shaft is a cylindrical bone that gradually becomes triangular distally. This bone serves as an insertion site for the pectoralis major, deltoid, and coracobrachialis and is the site of origin for the brachialis, triceps, and brachioradialis. The radial nerve is the major nerve of the humerus shaft which is seen in the spiral groove and is approximately 14 cm from the lateral epicondyle and 20 cm from the medial epicondyle. The major nerves of the distal humerus are the ulnar nerve and radial nerve. Distal humerus fractures comprise the supracondylar fractures, single condyle fractures, bi-column fractures and coronal shear fractures. Treatment options include open reduction and internal fixation, closed reduction and percutaneous pinning, and intramedullary nailing or bracing.[1][2][3]
Etiology
Humerus fractures occur as a result of trauma or pathologic fractures often due to metastatic disease. When these fractures are due to trauma, they occur from both high- and low-energy trauma.[4]
Epidemiology
Proximal humerus and humerus fractures account for 4% to 6% and 1% to 3% of all fractures respectively in both young and elderly patients. In young men, these fractures are usually a result of high-energy trauma while in the older population, this fracture is seen in women after a ground-level fall. Interestingly, humerus shaft fractures in polytrauma patients are independent predictors of intra-abdominal injury, long bone, and hand fractures. Typically, these injuries cause temporary disability in the younger population whereas permanent disability can be seen in the elderly.[5][6]
History and Physical
Common physical exam findings include erythema of the of the arm, inability to lift the arm due to pain, and holding onto the elbow of the injured arm for support. During the physical exam, neurovascular status pre- and postreduction is critical to identify any iatrogenic injury to neurovascular structures. In some instances, fracture reduction is necessary and is typically assisted by the influence of gravity with the arm in the anatomic position.
Evaluation
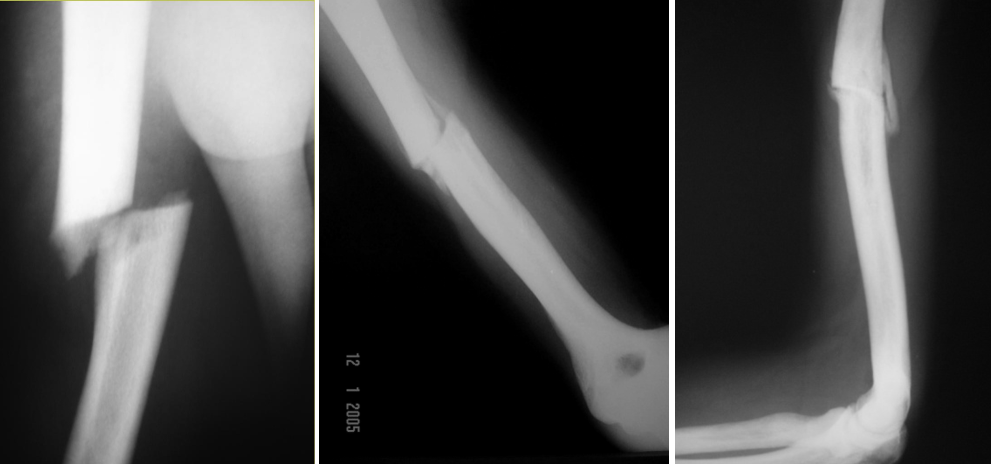
The recommended views for radiographic evaluation of the proximal humerus fracture include a true AP, scapular Y, and axillary. CT scan is performed for preoperative planning if there is intra-articular comminution or if the position of the head or greater tuberosity is uncertain. If a humerus shaft fracture is suspected, AP and lateral views including the joint below and above should be a part of the initial evaluation. With suspected distal humerus fractures, the recommended radiographic views include an AP and lateral of the humerus and elbow which should include the entire humerus and forearm.[7]
Treatment / Management
Nonoperative management with a sling and progressive rehabilitation of proximal humerus fractures is indicated in minimally displaced surgical neck fractures, greater tuberosity fractures displaced less than 5 millimeters, and patients who are not surgical candidates. Closed reduction and percutaneous pinning is indicated for two-part surgical neck fractures, 3-part and valgus-impacted four-part fractures with minimal metaphyseal comminution, and an intact medial calcar. Open reduction and internal fixation is indicated in greater tuberosity fractures displaced more than 5 millimeters and head-splitting fractures in young patients. Intramedullary rodding indications include surgical neck fractures or 3-part greater tuberosity fractures in younger patients and combined proximal humerus and humeral shaft fractures. Hemiarthroplasty is a viable option in anatomic fractures in elderly patients and fractures not amenable to open reduction and internal fixation. Total shoulder arthroplasty is indicated if the glenoid surface is compromised, while reverse total shoulder arthroplasty is indicated in individuals in a nonfunctioning rotator cuff or elderly individuals with reconstructable tuberosities.[8][9][1]
Traditionally, the mainstay of treatment of humerus shaft fractures is nonoperative. Due to the non-weight-bearing nature of the bone and the vast soft tissue envelope, slight deformity can be acceptable with favorable results. In most cases, nonoperative treatment consists of a Sarmiento brace. An advantage of using this brace is that the joints above and below the fracture are mobile, minimizing joint stiffness. Another advantage is removability of the brace, allowing for better axillary hygiene. Fracture alignment is maintained by the soft tissue envelope of the upper arm which has been described as the inner splint. Indications for nonoperative treatment include acceptable alignment less than 20 degrees anterior angulation, less than 30 degrees varus, valgus angulation, and less than 3 centimeters shortening. Absolute contraindications include severe soft tissue injury or bone loss, vascular injury requiring repair and brachial plexus injury. Typically, a coaptation splint is first used for 3 to 4 weeks until the swelling resolves. Next, a functional brace is utilized extending from approximately 2.5 centimeters distal to the axilla to 2.5 centimeters proximal to the humeral condyles. Weekly radiographs are recommended for the first 3 weeks to ensure adequate reduction. After this period, radiographs can be taken every 3 to 4 weeks.
Open reduction and internal fixation are indicated in open fractures, vascular injury requiring repair, brachial plexus injury, floating elbow (ipsilateral forearm fracture), and compartment syndrome. Other relative indications include polytrauma, bilateral humerus fractures, pathologic fractures, and burns or soft tissue injury precluding bracing. Benefits of this procedure include direct visualization of the fracture, anatomic fracture reduction, interfragmentary compression, identification of the radial nerve, and no violation of the adjacent joints. Disadvantages include the increased risk of soft tissue stripping, the risk of fracture at the end of the plate, and poor screw purchase in osteoporotic or comminuted bone. Dynamic compression plating is often the implant used when open reduction and internal fixation are performed, but locking plates can be helpful in osteoporotic bone. Minimally invasive plate fixation is another method that can be used but is not commonly performed. Some of the theoretical advantages of this method include a decreased amount of soft tissue injury and stripping which increases the healing potential in the injured area.
Depending on the location of the fracture, different surgical approaches are used. The deltopectoral approach or lateral approach can be used for proximal humerus fractures. The anterolateral approach is used for proximal to middle third shaft fractures. In this approach, the radial nerve is identified between the brachialis and brachioradialis distally. The posterior approach to the humerus is utilized for distal to middle third shaft fractures. During the approach, the triceps can either be split or elevated with lateral paratricipital exposure. The radial nerve is medial to the long and lateral heads of the triceps, while it is approximately 2 centimeters proximal to the deep head of the triceps and leaves the posterior compartment through the lateral intramuscular septum approximately 10 centimeters proximal to the radiocapetellar joint.
External fixation of the humerus shaft is not commonly performed but can be used as a method for stabilization in the unstable patient or open fractures with severe tissue loss.
Intramedullary nailing has comparable union rates and is another viable option for patients. Indications are pathologic fractures, segmental fractures, and comminuted fractures. This method is less invasive and typically involves shorter operating time. Disadvantages include an increased incidence of shoulder dysfunction, pain at the entry site, and rotational deformity.
Treatment of distal humerus fractures includes cast immobilization for Milch type I fractures. Closed reduction and percutaneous pinning are performed in displaced Milch Type I fractures, and open reduction and internal fixation is performed in supracondylar fractures, intercondylar/bicolumnar fractures, and Milch Type II fractures. Total elbow arthroplasty is indicated in elderly patients with distal bicolumnar fractures.
Prognosis
Proximal humerus and shaft fractures have favorable outcomes with a high union rate and low infection rate after operative and nonoperative management. Distal humerus fractures have less favorable outcomes. Approximately 75% of patients regain elbow motion and strength with the goal of a range of motion to between 30 and 130 degrees.
Complications
Radial nerve palsy is a feared complication of humerus shaft fractures that can occur during the injury, open reduction, and internal fixation or intramedullary nailing. In closed fractures, this is often a result of neuropraxia, while in open fractures it is a result so neurogenesis. This complication is more common in third distal fractures as this is the location where the radial nerve is closest to the humerus. In a closed fracture, radial nerve palsy is not an indication for open reduction and internal fixation with nerve exploration. Most palsies return with no treatment in 3 to 6 months. If no return of function is seen at 3 to 4 months, an EMG should be performed. Surgical exploration is indicated in open fractures, a closed fracture with the failure of improvement over 3 to 6 months, and fibrillations at 3 to 4 months on EMG.
Pearls and Other Issues
Proximal humerus fractures are classified based on the Neer classification as 2-, 3-, and 4-part fractures. These are classified as the greater and lesser tuberosity, articular surface, and shaft displaced more than 1 cm or greater than 45 degrees. Distal humerus fractures comprise of supracondylar fractures, single condyle fractures, bicolumnar fractures, and coronal shear fractures. These fractures can be classified as supracondylar fractures and distal single-column fractures and subclassified using the Milch classification. Milch type I fractures are fractures through the lateral trochlear ridge compared to Milch type II fractures with the lateral trochlear ridge intact. The Jupiter classification is used to identify five articular fragments: (1) the capitellum/lateral trochlea, (2) lateral epicondyle, (3) posterolateral epicondyle, (4) posterior trochlea, and (5)medial trochlea/epicondyle. With distal humerus fractures, if the elbow is flexed less than 90 degrees, a transcolumnar fracture is seen and a direct posterior injury results in an olecranon fracture compared to elbow flexion greater than 90 degrees with an intercondylar fracture.
Enhancing Healthcare Team Outcomes
Humerus fractures are relatively common in the elderly and in those who participate in intense physical sporting activities. The majority of patients with humerus fracture first present to the emergency department and hence the triage nurse and emergency room physician must be aware of the importance of prompt referral to an orthopedic surgeon. The outcomes for most patients with humerus fracture are good. Complete union can often take 6-10 weeks and even after recovery, some patients may exhibit a slight decrease in the shoulder range of motion. It is very important to follow up patients with humerus fracture to ensure that they are not developing the frozen shoulder; hence some type of exercise rehab program must be recommended.[2][10]