Continuing Education Activity
Biliary duct hamartomas, otherwise known as Von Meyenburg complexes, are dilated cystic bile ducts, which are embryologic remnants that failed to involute during the period of embryogenesis. They are typically small (less than 5mm) and present as multiple lesions scattered throughout the liver. They are rare, asymptomatic, and with a relatively benign disease course. There is a possible association with malignant transformation; thus, suspicious or evolving lesions should be investigated further for a definitive diagnosis. This activity describes the evaluation and management of multiple biliary duct hamartomas and explains the role of the interprofessional team in improving care for patients with this condition.
Objectives:
- Describe the epidemiology of multiple biliary duct hamartomas.
- Review the typical imaging findings associated with multiple biliary duct hamartomas.
- Identify the treatment considerations for patients with malignant transformation of multiple biliary duct hamartomas.
- Outline the importance of collaboration and communication amongst the interprofessional team to enhance care coordination for patients with multiple biliary duct hamartomas.
Introduction
Multiple biliary duct hamartomas or “von Meyenburg complexes” are rare, benign liver malformations characterized by cystic dilated biliary ducts that were first discovered in 1918 by Von Meyenburg. They are usually incidentally found at autopsy or laparotomy due to the asymptomatic clinical course.[1][2][3][4] They are usually diagnosed on imaging as single or multiple small cystic nodules ranging from 0.05 cm to 1.5 cm in size. Although incidental findings can mimic metastatic liver disease as well as other clinically significant diseases, which may prompt an extensive diagnostic work-up and even surgical intervention. [5] Thus, proper diagnosis with specific imaging findings or confirmation with histological evaluation is required.[6][7]
Etiology
Biliary duct hamartomas, otherwise known as Von Meyenburg complexes, are dilated cystic bile ducts, which are embryologic remnants that failed to involute during the period of embryogenesis. They are typically small (<5mm) and present as multiple lesions scattered throughout the liver, often referred to as "a starry night."[8] They are rare, asymptomatic, and with a relatively benign disease course. They are most commonly found during laparotomy for another procedure, on imaging, or at autopsy. Etiology is unknown; however, biliary duct hamartomas are thought to develop from the smaller embryonic interlobular bile ducts, which fail to involute.[9]
Several studies have found an increased frequency in cirrhotic livers due to chronic viral hepatitis or alcohol liver disease or secondary to inflammation or ischemia, which may demonstrate that these lesions can be acquired and environmental exposure can play an important role.[2][4][5]In addition, biliary duct hamartomas are more common in patients with polycystic liver and polycystic kidney disease or those with congenital hepatic fibrosis.[2]
Epidemiology
The prevalence of multiple biliary duct hamartomas ranges from 0.6% to 5.6% in adults seen at autopsy and 0.35% in needle biopsy of liver lesions for diagnosis.[3][4][10] Prevalence in children is 0.9%.[11] Although they have been observed in infants and children under two years of age, most patients are greater than 35 years old. [8] Females are affected three times more than males.[4] According to one autopsy study, approximately 5% of the population have bile duct hamartomas.[12]
Pathophysiology
Bile duct hamartomas are thought to arise from the abnormal development of intrahepatic bile ducts. Histologically, they are composed of inflammatory cells, bile ducts, and fibrosis. No BRAF V600E mutations have yet been identified in biliary hamartomas despite bile duct adenomas having that mutation.[13] Biliary duct hamartomas have a minor risk of malignant transformation to intrahepatic cholangiocarcinoma or, less commonly, hepatocellular carcinomas.[5]
Histopathology
Macroscopically, biliary duct hamartomas appear as multiple small grey-white nodules scattered throughout both liver lobes within the subcapsular and periportal areas. These lesions typically do not communicate with the biliary tree, although they can.[3][9] Microscopically, they are composed of a collection of dilated branching cystic bile ducts lined with a single layer of cuboid epithelial cells surrounded by an abundant fibro-collagenous stroma. The lesions measure about 0.1 cm to 1.5 cm each. The bile duct lumens typically contain bile-stained granular material.[2][3][10] They are thought to arise from congenital bile duct remnants that have failed to involute.[3]
History and Physical
Typically, patients are clinically asymptomatic with an unremarkable physical exam, as the diagnosis is usually incidental to laparotomy for another procedure. Rarely will patients present with fevers, jaundice, abdominal distension, and right upper quadrant or epigastric pain.[3][10][11] Abdominal pain is the most common presenting symptom among those who are symptomatic. While most physical exams are unremarkable, positive Murphy's sign and right upper quadrant tenderness to palpation were prevalent.[5]
Evaluation
As a result of the incidental and usually benign nature of multiple biliary duct hamartomas, no evaluation is necessary for the diagnosis. However, while most patients will have normal lab results, some can present with mild elevations in liver function tests, specifically aspartate aminotransferase (AST) and gamma-glutamyl transpeptidase (GGT). Patients should have a baseline CA 19-9 level drawn, which can be slightly elevated with multiple biliary duct hamartomas. Some patients have seen hyperbilirubinemia, hypoalbuminemia, and increased C-reactive protein.[5]
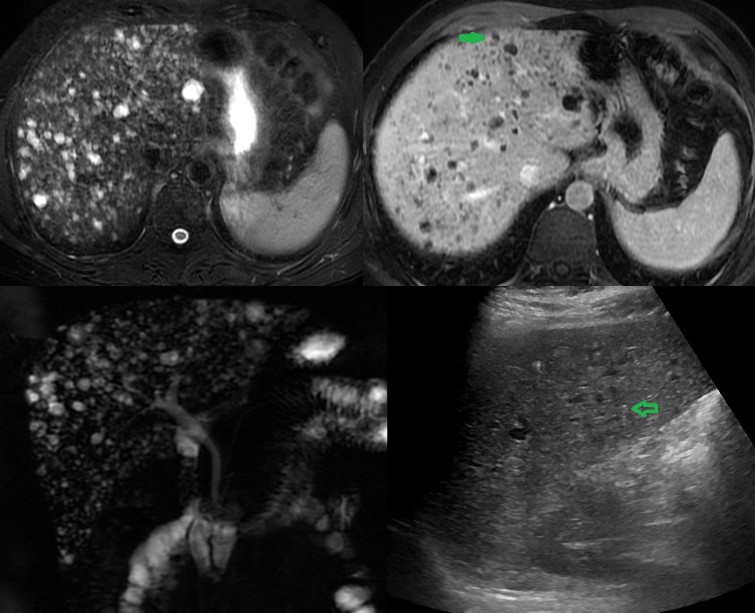
Typically these lesions are found initially on ultrasound or computed tomography (CT) done for a different reason. On ultrasound, these lesions appear as multiple hyper and hypoechoic areas within the liver with comet-tail artifacts. On CT, they appear as multiple, nodular, irregular cystic liver lesions with low attenuation and no enhancement with intravenous contrast injection. The most sensitive imaging modality is magnetic resonance imaging or magnetic resonance cholangiopancreatography (MRI/MRCP), which shows multiple T1 hypointense and T2 hyperintense diffuse cystic liver lesions of variable sizes 0.1 cm to 1.5 cm which do not communicate with the biliary tree and do not enhance with intravenous gadolinium injection.[10][11][14]
The most specific finding on MRCP for biliary duct hamartomas is mural nodules, which are endocytic polypoid projections due to conjunctive septa that are isointense on T1-weighted images and hyperintense on T2-weighted images. The presence of mural nodules can help diagnose multiple biliary duct hamartomas with accuracy and help avoid misdiagnosis.[15] While biopsies are not necessary for diagnosis, most patients will undergo biopsies as part of the workup. A biopsy is the best diagnostic tool to rule out malignancy.[5]
Treatment / Management
Aside from the possible risk of malignant transformation, multiple biliary duct hamartomas is a benign, otherwise asymptomatic conditions with no long-term adverse outcomes, and no treatment is required.[11] However, suspicious lesions should be followed regularly with repeat imaging and possible liver biopsy for a definitive diagnosis. Any changes of the lesion on repeat imaging, warning signs, such as weight loss, or any elevations from tumor markers (CA 19-9) from baseline should warrant further workup with possible surgical resection when the diagnosis is definitive and the lesion is operable.[4][11]
Differential Diagnosis
The diagnosis of multiple biliary duct hamartomas is usually incidental at autopsy or on radiographic imaging. However, when discovered on imaging, it is essential to determine a correct diagnosis due to its close resemblance to metastatic disease of the liver, especially in a patient with extra-hepatic malignant tumors. Typically, liver metastases are ill-defined with variable sizes on plain computed tomography (CT) imaging with varying degrees of enhancement with IV contrast.[3] Bile duct hamartomas, on the contrary, typically do not enhance with IV contrast on CT imaging, are usually uniform, and measure 1 mm to 15 mm in size.[2]
Other differential diagnoses include bile duct adenomas, peribiliary cysts, microabscesses of the liver, intrahepatic biliary stones, and Caroli’s disease. Bile duct adenomas have small round tubules with small inconspicuous lumens, while bile duct hamartomas have dilated lumens with inspissated bile.[2] Peribiliary cysts are located specifically within the hepatic hilum within connective tissue along the portal vein, do not communicate with the biliary tree, and typically enlarge and compress the biliary tree over time, which is contrasted to the diffuse scattered nature of biliary duct hamartomas.[3][9]
Microabscesses of the liver are usually present as multiple round loculated hypodense lesions on CT. They are seen in patients with immunosuppression, fever, and epigastric pain, which can be differentiated from bile duct hamartomas by signs of sepsis, which are not typically seen in the latter.[3] Caroli disease is characterized by intrahepatic bile duct dilation communicating with the biliary tree, differentiated from bile duct hamartomas with MRCP by contrast enhancement with intravenous gadolinium.[3][14]
Surgical Oncology
The clinical problem posed by this benign tumor is for the surgeon or surgical oncologist who encounters such a lesion during a laparotomy for another malignant lesion. Typically, the surgeon will perform a liver biopsy for a frozen section once this lesion is encountered. It can be difficult to distinguish benign hamartomas from metastatic disease in the liver. A pathologist who receives the specimen for the frozen section and is unaware of this entity may label the lesion as metastatic carcinoma or Carolis disease. However, these lesions do not communicate with bile ducts, and no treatment is necessary.
Prognosis
Due to the asymptomatic clinical course in most and incidental findings at autopsy for patients who die of unrelated diseases, the prognosis is typically great. However, patients with malignant transformation typically have a very poor 5-year survival rate of 15% to 40%.[16] Some patients with diffuse biliary duct hamartomas often have persistently elevated liver function tests on their laboratory testing, at which point liver transplantation would be recommended.[8]
Complications
Small subsets of patients experience a malignant transformation of multiple biliary duct hamartomas to either intrahepatic cholangiocarcinoma (more common) or hepatocellular carcinoma. Risk factors for possible malignant transformation include long-term tobacco use, large biliary duct hamartomas (> 2 cm), and bile stasis.[17]
It is essential to have periodic long-term follow-ups with these patients with a definitive diagnosis of multiple biliary duct hamartomas. Patients require a baseline CA 19-9 level, which can be slightly elevated with multiple biliary duct hamartomas. Any changes to MRI/MRCP imaging, in addition to elevations in tumor markers, warrants further evaluation with liver lesion biopsy and possible resection of lesions if operable with a definitive diagnosis.[11]
Deterrence and Patient Education
Educational materials for the patient, as well as clinicians and other healthcare personnel, should include the following:
- Complete understanding of the broad differential diagnoses for multiple biliary duct hamartomas
- Specific findings on ultrasound, computed tomography, and magnetic resonance imaging
- importance of long-term follow-up for these patients due to possible malignant transformation to help prevent adverse outcomes
Enhancing Healthcare Team Outcomes
Patients with multiple biliary duct hamartomas typically require no extensive workup, but an interprofessional healthcare team approach is recommended. This team includes clinicians (MDs, DOs, NPs, and PAs), specialists (particularly a radiologist), and nursing staff. While the disease is generally benign, it has the potential for malignant transformation, so the entire team must remain vigilant, including the patients themselves.
It is crucial that radiologists understand this disease and its appearance on imaging to help differentiate it from more malignant or life-threatening liver lesions. Surgeons and oncologists must be aware of this disease in the case of malignant transformation requiring liver resection and chemotherapy or radiation for treatment. It is a condition where the differential is extremely important since getting it wrong can result in either missing a more malignant disease or treating the patient inappropriately if it is not malignant. Good communication and education with the pathologist and surgeon are paramount to dealing with benign liver lesions and improving patient outcomes. Nurses can help coordinate the various clinicians and specialists on the case, ensure all team members have accurate and updated patient information, as well as counsel the patients regarding their condition and how to monitor for signs of possible malignant transformation. In this way, the interprofessional team approach to management is the most appropriate means to achieve optimal outcomes. [Level 5]