Continuing Education Activity
A brain abscess is a localized area of necrosis within the brain parenchyma, often stemming from infectious or traumatic origins. Infections in head and neck sites and microbial pathogens like Staphylococcus and Streptococcus contribute to its development. The abscess can originate locally (from the ear, teeth, sinuses, mastoid air cells, or epidural) or remotely (lung, heart, kidney). Brain abscesses may be associated with congenital heart disease in young children and are more prevalent in the third decade of life.
Clinicians participating in thi activity can expect to enhance their knowledge and skills in the diagnosis and management of brain abscesses. The program provides an overview of the evidence-based approaches, emphasizing accurate identification, appropriate imaging modalities, risk factors, and effective treatment strategies. Participants gain insights into the multidisciplinary collaboration required for optimal patient care. The activity aims to improve clinicians' competence in navigating the complexities of brain abscess cases, ultimately leading to more informed decision-making, enhanced patient outcomes, and a heightened ability to address the challenges associated with this neurological condition.
Objectives:
Identify the clinical manifestations and radiological features indicative of a brain abscess.
Implement appropriate diagnostic procedures, including neuroimaging and microbiological studies, to confirm the diagnosis of a brain abscess.
Apply evidence-based pharmacological interventions to treat brain abscesses, considering antibiotic selection and dosage factors.
Collaborate with colleagues, including neurosurgeons, radiologists, infectious disease specialists, and other relevant professionals, to optimize the management of brain abscesses.
Introduction
A brain abscess is a focal area of necrosis surrounded by a membrane within the brain parenchyma, usually resulting from infectious processes or, rarely, traumatic or surgical events.[1][2][3] Originating locally in areas like the ear, teeth, sinuses, mastoid air cells, or epidural, these abscesses can also develop remotely in sites such as the lung, heart, and kidney. In young children, brain abscesses may be associated with congenital heart disease. While brain abscesses may occur at any age, they are more prevalent in individuals in their third decade.
Etiology
Brain abscesses can originate locally and spread to other parts of the body. These abscesses may form from infections in nearby areas, such as the ear or sinuses, and can occasionally extend to more distant sites like the lung or heart.
Direct Local Spread
Infections in the head and neck region can give rise to a brain abscess. Otitis media (5%) and mastoiditis are linked to the inferior temporal lobe (see Image. Temporal Abscess) and cerebellar brain abscesses. Paranasal sinus infections contribute 30% to 50% of reported cases, leading to brain abscess development. Infections from frontal or ethmoid sinuses may extend to the frontal lobes, while dental infections commonly result in frontal lobar abscesses.[4]
Facial trauma, including those resulting from neurosurgical procedures, can result in necrotic tissue and brain abscess formation. The presence of metal fragments or other foreign bodies left in the brain parenchyma can also serve as a nidus for infection.[1][5]
Generalized Septicemia and Hematogenous Spread
Various conditions can cause hematogenous seeding of the brain. Common contributing factors include the lung, the most frequently associated organ. Pulmonary infections, such as lung abscesses and empyemas, are often observed in individuals with bronchiectasis, while cystic fibrosis represents a significant contributing factor.[6]
Additional factors contributing to the hematogenous brain seeding include pneumonia, pulmonary arteriovenous malformation, and bronchopleural fistula. In children, cyanotic congenital heart diseases are associated with more than 60% of cases. Bacterial endocarditis, ventricular aneurysms, and thrombosis are also identified as causative factors. Skin, pelvic, and intraabdominal infections are also frequently reported risk factors.[7]
Approximately 10% of patients with pulmonary arteriovenous malformations (PAVMs) develop brain abscesses. Bacteremia-associated brain abscesses commonly cause multiple abscesses, predominantly in the middle cerebral artery distribution and typically at the gray-white matter junction.
The most commonly isolated microbial pathogens from brain abscesses are staphylococcal and streptococcal. Staphylococcus aureus and Viridian streptococci are this category's most prevalent bacterial species.[8]
A list of causative pathogens in brain abscesses in a meta-analysis of 9699 patients from 123 studies is as follows:[9]
- Streptococcus species
- S pneumoniae
- Viridans streptococci
- Staphylococcus species
- Enterococcus
- Gram-negative enteric
- Klebsiella pneumoniae
- Escherichia coli
- Proteus species
- Actinomycetales
- Corynebacterium
- Nocardia
- Actinomyces
- Mycobacterium tuberculosis
- Haemophilus species
- Pseudomonas species
- Peptostreptococcus species
- Bacteroides species
- Fusobacterium species
- Fungi
- Parasites
Epidemiology
Brain abscesses are approximately 8% of intracranial masses in developing countries and 1% to 2% in Western countries, with roughly 4 cases occurring per million. The prevalence of brain abscesses in patients with AIDS is higher. Therefore, the prevalence rate has increased with the emergence of the AIDS pandemic.
Approximately 1500 to 2500 cases of brain abscesses are diagnosed annually in the US. The incidence of fungal brain abscesses has also risen because of the increased use of broad-spectrum antibiotics and immunosuppressive agents like steroids. Prevalence is highest in adult men younger than 30, with pediatric cases occurring most frequently in children aged 4 to 7. Neonates constitute the third high-risk group for brain abscesses.
Vaccination has contributed to reducing the prevalence of brain abscesses in young children. Data suggests that brain abscesses are more predominant in males than females, with a male-to-female ratio between 2:1 and 3:1. Geographical and seasonal differences have no significant impact. In developing countries with poor living standards, brain abscesses account for a disproportionate percentage of space-occupying intracranial lesions compared to developed nations.[10][11]
Pathophysiology
Histologic changes in brain abscesses depend upon the stage of the infection. In the early stage (first 1 to 2 weeks), referred to as focal cerebritis, the lesion is poorly demarcated and exhibits acute inflammatory changes like vascular congestion and localized edema. This early stage is commonly called cerebritis. After 2 to 3 weeks, necrosis and liquefaction occur, which is then covered by a distinct capsule consisting of an inner layer of granulation tissue, a middle collagenous layer, and an outer astroglial layer. The surrounding brain parenchyma is often edematous.
History and Physical
Symptoms are present in about two-thirds of cases for 2 weeks or less, with the diagnosis typically established around 8 days after the onset of symptoms. The course of the condition ranges from indolent to fulminant. Manifestations of brain abscesses tend to be nonspecific, contributing to a delay in diagnosis. Symptoms largely depend on the size and location of the space-occupying lesion or lesions. The triad of fever, headache, and focal neurologic deficit is observed in less than half of patients. The frequency of common signs and symptoms are as follows:
- Headache (69%-70%) is the most common medical symptom.[9]
- Mental status changes (65%), including lethargy progressing to coma, indicate severe cerebral edema and is a poor prognostic sign.
- Focal neurologic deficits (50%-65%) occur days to weeks after the onset of a headache.
- Pain, usually localized to the side of the abscess, may have a gradual or sudden onset. The pain is often severe in intensity and not relieved by over-the-counter pain medications.
- Seizures (25%-35%) can be the initial manifestation of brain abscess, with grand mal seizures being prevalent in frontal abscesses.
- Nausea and vomiting (40%) are most commonly linked to an occipital lobe abscess or an abscess that has leaked into a lateral ventricle.
- Nuchal rigidity (15%) is most commonly associated with an occipital lobe abscess or an abscess that has leaked into a lateral ventricle.
- Third and sixth cranial nerve deficits
- Rupture of abscess usually presents with a sudden worsening headache, followed by emerging signs of meningismus.
Evaluation
A comprehensive evaluation for suspected brain abscesses includes the following studies:
Routine tests: Complete blood count (CBC) with differential and platelet count, erythrocyte sedimentation rate (ESR), serum C-reactive protein (CRP), serologic test, and blood cultures (at least 2, preferably before antibiotic therapy).
Lumbar puncture: Rarely required and should only be performed after a prior head computed tomography (CT) and magnetic resonance imaging (MRI) scan to rule out increased intracranial pressure due to the potential risk of cerebrospinal fluid (CSF) herniation and potential fatality. In cases of acute patient presentation or suspicion of meningitis, blood cultures can be utilized to initiate antibiotic therapy.
Lumbar puncture results are typically nonspecific, characterized by an elevated protein level, pleocytosis with a variable neutrophil count, usually a normal glucose level, and sterile cultures. In the case of rupture, when the white blood cell count (WBC) becomes high, additional findings may include elevated CSF lactic acid and abundant red blood cells (RBCs) in the CSF.
Stereotactic Computed Tomography or Surgical Aspiration
Samples obtained can be employed for various diagnostic purposes, including culture, Gram stain, serology, histopathology, and polymerase chain reaction (PCR). Additionally, these analyses contribute to tailoring targeted treatment strategies and monitoring the response to therapy, enhancing overall patient care.
Computed Tomography
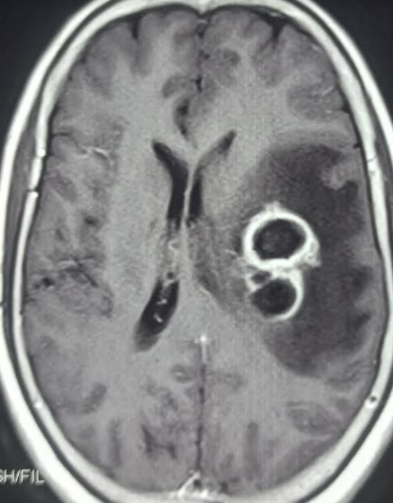
Although not as sensitive as an MRI, a CT scan is often obtained in an emergency (see Image. Multiple Brain Abscesses).[12] Imaging findings are contingent on the stage of the lesion. Early cerebritis often manifests as an irregular low-density area that does not enhance or may exhibit infrequent patchy enhancement. As cerebritis progresses, a more distinct rim-enhancing lesion becomes visible.
Enzmann et al reported that CT findings of patchy enhancement in early cerebritis evolve into a rim of enhancement in late cerebritis, eventually forming the brain abscess. A key histopathologic difference is that rim enhancement in late cerebritis is not associated with collagen deposition, as seen in an abscess surrounding a purulent cavity. Serial CT examinations in patients with late abscesses demonstrate progressively decreasing edema and mass effect. The brain abscess wall is usually smooth and regular, with a 1 mm to 3 mm thickness, surrounded by parenchymal edema.
The ring of enhancement may not be uniform in thickness, appearing relatively thin on the medial or ventricular surface in the deep white matter, where vascularity is less abundant. Administration of steroids can suppress edema and contrast enhancement. Multi-location with subjacent daughter abscesses, or satellite lesions, is frequently observed. The presence of gas, if detected, is suggestive of gas-forming organisms.
Magnetic Resonance Imaging
MRI is the preferred imaging modality for diagnosing and following lesions due to its heightened sensitivity, particularly for early cerebritis and satellite lesions, particularly those located in the brain stem. Additionally, it facilitates a more accurate estimation of necrosis and the extent of the lesion. MRI allows for greater contrast between cerebral edema and the brain and is also more sensitive in detecting the spread of inflammation into the ventricles and subarachnoid space (see Image. Brain Abscess).[13][14]
Conventional Spin-Echo Imaging with Contrast
Classic MRI findings of an abscess include a contrast-enhanced rim surrounding a necrotic core. The rim is T1 isointense to hyperintense relative to white matter and T2 hypointense. On MRI, the characteristic smooth tri-laminar structure of the rim on T2W imaging proves helpful in differentiating from other ring-enhancing lesions. Central necrosis shows variable hyperintensity on T2 depending on the degree of protein content and is hypointense on T1.
Diffusion-Weighted Magnetic Resonance Imaging
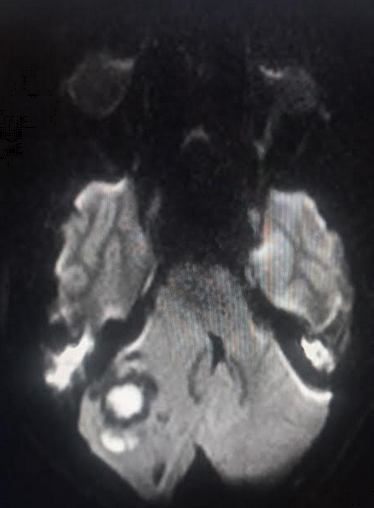
Diffusion-weighted imaging (DWI) distinguishes brain abscesses from other ring-enhancing brain lesions. Abscesses typically appear hyperintense on DWI, indicating restricted diffusion, a characteristic feature of viscous materials like pus (see Image. Cerebellar Abscess). In contrast, neoplasms like gliomas lack restricted diffusion, appearing as hypointense or variable hyperintense signals, notably lower than those observed in abscesses.
Diffusion-tensor imaging based on 3-dimensional diffusivity is commonly employed to evaluate white matter tracts. Fractional anisotropy, a quantitative variable derived from diffusion-tensor imaging, is calculated to gauge the degree of tissue organization. In brain abscesses, this variable reflects the degree of tissue organization and tends to be higher, possibly due to organized leukocytes within the abscess cavity.
Proton MR spectroscopy probes tissue metabolism, and spectral analysis reveals elevated succinate, which, although not commonly seen, is highly specific for an abscess. Other significant metabolites include elevated acetate, alanine, and lactate signals. Amino acids derived from neutrophil-driven protein breakdown suggest a pyogenic abscess. MR spectroscopy can aid in further differentiating between anaerobic and aerobic metabolism by detecting elevated succinate and acetate peaks, observed only in anaerobic infections due to glycolysis and subsequent fermentation. Additionally, lactate peaks are lowest in strict anaerobes owing to metabolic lactate consumption.
Brain Biopsy
Biopsy through needle aspiration or surgical drainage is typically recommended in most patients to establish the diagnosis and identify the etiologic agent.[15] However, an open or stereotactic brain biopsy may be necessary to confirm a specific parasitic or fungal abscess. There are situations where a biopsy may be needed or can be delayed, including:
- The presence of a brain abscess in the setting of bacteremia, especially when antibiotic therapy aligns with the results of a blood culture.
- Strong support for the diagnosis is provided by epidemiologic, clinical, serologic, and neuroimaging findings (eg, neurocysticercosis and toxoplasmosis).
- Abscesses located in inaccessible or vital regions of the brain.
- A Glasgow coma score of >12 and lesions measuring <2.5 cm.
Treatment / Management
A brain abscess can lead to elevated intracranial pressure and has significant morbidity and mortality. The management strategies are typically divided into medical and surgical approaches.
Medical management is an option for deep-seated, small abscesses (<2 cm), cases with coexisting meningitis, and a few other selected instances. Usually, a combination of medical and surgical approaches is considered.[2]
CT and MRI of the brain imaging results play a crucial role in management by localizing the abscess and delineating details, including dimensions and the number of abscesses. Typically, large abscesses (>2 cm) are considered for aspiration or excision, depending on the surgical skills of the operator. The approach for multiple abscesses includes a prolonged course (4-8 weeks) of high-dose antibiotics with or without aspirations, guided by weekly CT scanning.
The choice of antibiotic regimen should be carefully selected based on the microorganisms isolated from blood or CSF. Certain antibiotics, such as first-generation cephalosporins, aminoglycosides, and tetracyclines, are ineffective in treating brain abscesses as they cannot cross the blood-brain barrier.
Specific antibiotic regimens according to microorganisms are as follows:
- Gram-positive bacteria, including streptococci: third-generation cephalosporin (eg, cefotaxime, ceftriaxone) or penicillin G, are effective.
- S aureus and S epidermis, usually associated with penetrating brain trauma or neurosurgical procedures, should be covered with vancomycin. Vancomycin is also effective for Clostridium species. Linezolid, trimethoprim-sulfamethoxazole, or daptomycin can be considered in cases of vancomycin resistance.
- Fungal infections, including Candida and Cryptococcus, must be treated with amphotericin B.
- For Aspergillus and Pseudallescheria boydii, voriconazole can be considered.
- Toxoplasma gondii infection is treated with pyrimethamine and sulfadiazine, which can be combined with highly active antiretroviral therapy (HAART) in cases of HIV.
Steroids can be considered in select cases to reduce the mass effect, improve antibiotic penetration, and alleviate cerebral edema.[16] However, their use should be judicious, carefully weighing potential benefits against the risk of exacerbating an underlying infection or delaying wound healing.
The surgical approach plays a pivotal role in managing brain abscesses, and the choice of procedure depends on the operator's skill and preference. Available techniques include ultrasound or CT-guided needle aspirations via the stereotactic method, burr hole, and craniotomy for loculated multiple abscesses. Intravenous or intrathecal agents targeting specific microorganisms are often considered in conjunction with surgical therapy.[17]
Differential Diagnosis
The differential diagnoses encompass a range of conditions including:
- Bacterial meningitis
- Brain tumors
- Demyelination
- Epidural/subdural abscess
- Encephalitis
- Fungal or parasitic infestations such as cryptococcosis and cysticercosis
- Mycotic aneurysm
- Septic dural sinus thrombosis
Treatment Planning
Antimicrobial therapy for normal healthy adults without renal impairment is outlined below.
Table 1. Intravenous Therapy Against Brain Abscesses
| Antimicrobial agent |
Dose |
Comments |
| Amikacin |
5 mg/kg 3 times a day |
Not routinely used for treating brain abscesses but considered in cases with multidrug-resistant gram-negative infection.
Target peak serum concentrations of 25 to 40 µg/mL and trough serum concentrations of <8 µg/mL (ideally <4 µg/mL) are recommended.
|
| Ampicillin |
2 g 6 times a day |
|
| Aztreonam |
2 g 3-4 times a day |
Generally reserved for patients with severe beta-lactam allergies. |
| Cefepime |
2 g 3 times a day |
|
| Cefotaxime |
2 g 4-6 times a day |
|
| Ceftaroline |
600 mg 3 times a day |
Alternative therapy for MRSA not responding to vancomycin or linezolid; is usually combined with another agent effective against MRSA. |
| Ceftazidime |
2 g 3 times a day |
|
| Ceftriaxone |
2 g 2 times a day |
|
| Ciprofloxacin |
400 mg 2-3 times a day |
Generally reserved for patients with severe beta-lactam allergies. |
| Daptomycin |
6 to 10 mg/kg once a day |
Has poor central nervous system penetration and is used when other alternatives are unavailable for suspected S aureus (or proven MRSA) in patients who cannot tolerate vancomycin. Should be combined with rifampin therapy.
|
| Gentamicin |
1.7 mg/kg 3 times a day |
Not routinely used for treating brain abscesses but considered in cases with multidrug-resistant gram-negative infection.
A peak serum concentration of 7 to 10 µg/mL and trough serum concentration of <2 µg/mL (ideally <1 µg/mL) is usually recommended.
|
| Linezolid |
600 mg 2 times a day |
Alternative therapy for suspected S aureus (or proven MRSA) in patients who are unable to tolerate vancomycin.
Patients with poor IV access who have had an appropriate initial response can be switched to oral therapy.
|
| Meropenem |
2 g 3 times a day |
|
| Metronidazole |
7.5 mg/kg 3 to 4 times a day; maximum dose: 4 g/day |
|
| Moxifloxacin |
400 mg once a day |
Generally reserved for patients with severe beta-lactam allergies. |
| Nafcillin |
2 g 6 times a day |
|
| Oxacillin |
2 g 6 times a day |
|
| Penicillin G |
4 million units 6 times a day |
|
| Rifampin |
600 mg once a day |
Usually combined with other agents to enhance the antimicrobial activity. Not recommended as monotherapy. |
| Tobramycin |
1.7 mg/kg 3 times a day |
Not routinely used for treating brain abscesses but considered in cases with multidrug-resistant gram-negative infection.
A peak serum concentration of 7 to 10 µg/mL and trough serum concentration of <2 µg/mL (ideally <1 µg/mL) is usually recommended.
|
| Trimethoprim-sulfamethoxazole (co-trimoxazole) |
5 mg/kg 2 to 3 times a day |
|
| Vancomycin |
15 to 20 mg/kg 2 to 3 times a day |
|
Table references.[18][19]
Prognosis
With the advent of antimicrobials and imaging studies such as CT scanning and MRI, the mortality rate has reduced from 10% to 5%. The rupture of a brain abscess remains a fatal complication. The long-term neurological outcomes after infection depend on early diagnosis and prompt administration of antibiotics.
Complications
Complications that can arise secondary to a brain abscess include:
- Meningitis
- Ventriculitis
- Increased intracranial pressure
- Brain herniation
- Seizures
- Septicemia
- Neurological deficits
- Thrombosis of intracranial blood vessels
- Death
Deterrence and Patient Education
The patient should be educated on the importance of completing an entire course of prescribed antibiotics and, if necessary, taking anticonvulsants. Patients should promptly report to the hospital if they experience a new onset fever or exhibit features of raised intracranial pressure.
Pearls and Other Issues
Key facts to keep in mind about brain abscesses are as follows:
- A brain abscess is a localized area of necrosis in the brain often caused by infections.
- Infections in the head and neck can lead to brain abscesses.
- Abscesses can originate locally or spread from distant sites like the lung.
- It is more common in individuals in their third decade of life.
- In young children, it is associated with congenital heart disease.
- Commonly caused by Staphylococcus and Streptococcus.
- Nonspecific symptoms, with less than 50% presenting the classic triad.
- Combination of medical and surgical approaches.
Enhancing Healthcare Team Outcomes
Brain abscesses caused by bacterial infections remain a serious challenge to the central nervous system despite advancements in neuroimaging and neurosurgery, improved antibiotics, and newer microbiological techniques.[17] In cases where the condition goes undiagnosed or untreated, it is associated with extremely high morbidity and mortality. Successful treatment necessitates an integrated approach with a systemic perspective to diagnosis and treatment, involving a collaborative effort from various healthcare professionals.[20] A recommended interprofessional team includes:
- Neurosurgeons perform neurosurgical drainage when necessary.
- Radiologists help to locate and evaluate the extent of the abscess.
- Laboratory technologists identify the type of microorganisms growing in the abscess.
- Neurologists monitor patients for neurological deficits.
- Infectious disease specialists determine the cause and recommend appropriate antibiotics.
- Pharmacists manage the choice of antibiotics, address symptoms such as emesis and fever, and assess potential drug-drug interactions.
- Intensivists monitor the neurologic vitals in an intensive care unit (ICU) setting.
- Internists oversee patients for comorbidities like HIV and syndrome of inappropriate secretion of antidiuretic hormone (SIADH).
- Nurses play a crucial role in monitoring the vitals, administering medications, assessing for gross neurological deficits, and educating the family on the home management of such patients.
All interprofessional team members, irrespective of their discipline, should feel empowered to share any findings or deterioration they observe in the patient's condition. Effective communication within the team is crucial, ensuring that all relevant information is conveyed to the team properly. This collaborative approach facilitates timely and appropriate therapeutic interventions, ultimately enhancing patient outcomes.
Nevertheless, the optimal management of a brain abscess remains a subject of controversy. Current evidence-based medicine appears to lack conclusive data on critical aspects such as which patients should be managed with medication alone, the antibiotics with the best penetrability in a brain abscess, the criteria for surgical intervention, the efficacy of antibiotics, the ideal surgical approach, and the long-term outcomes.
To date, randomized clinical trials addressing the management of brain abscesses are lacking, mainly due to the urgent need for immediate treatment to prevent morbidity in this medical emergency. Despite the lack of comprehensive data, research studies focused on children with brain abscesses suggest that a combined or interprofessional approach may be the most effective way to reduce the morbidity and mortality associated with this severe infection.[21]