Continuing Education Activity
An esophageal diverticulum is a relatively rare disease in which there is an outpouching of the esophageal mucosa. Patients typically present if they develop symptoms of regurgitation or dysphagia. This activity highlights the role of the interprofessional team in caring for patients with this condition.
Objectives:
- Describe the different types of esophageal diverticulum.
- Recall the evaluation of a patient suspected of having an esophageal diverticulum.
- Summarize the treatment for esophageal diverticulum.
- Explain the need for a well-integrated, interprofessional team approach to improve care for patients with esophageal diverticula.
Introduction
An esophageal diverticulum is a relatively rare disorder of the esophagus.[1] It is an outpouching of the esophageal mucosa and is usually asymptomatic. Patients typically present when they have symptoms of regurgitation or dysphagia.
There are different ways to categorize esophageal diverticulum. Esophageal diverticula can be divided into true and false diverticula. True diverticula are outpouchings that include all layers of the esophageal wall while false diverticula only include the mucosa or submucosa.
An esophageal diverticulum can also be characterized by how it is formed: pulsion or traction.[2] Pulsion diverticula are created when there is increased intraluminal pressure causing herniation of the esophageal wall in an area of weakness and usually occur in the setting of dysmotility of the esophagus.[3] Traction diverticula occur when there is an external force on the esophageal wall such as mediastinal inflammation that adheres and pulls on the esophageal wall creating a defect or diverticulum.
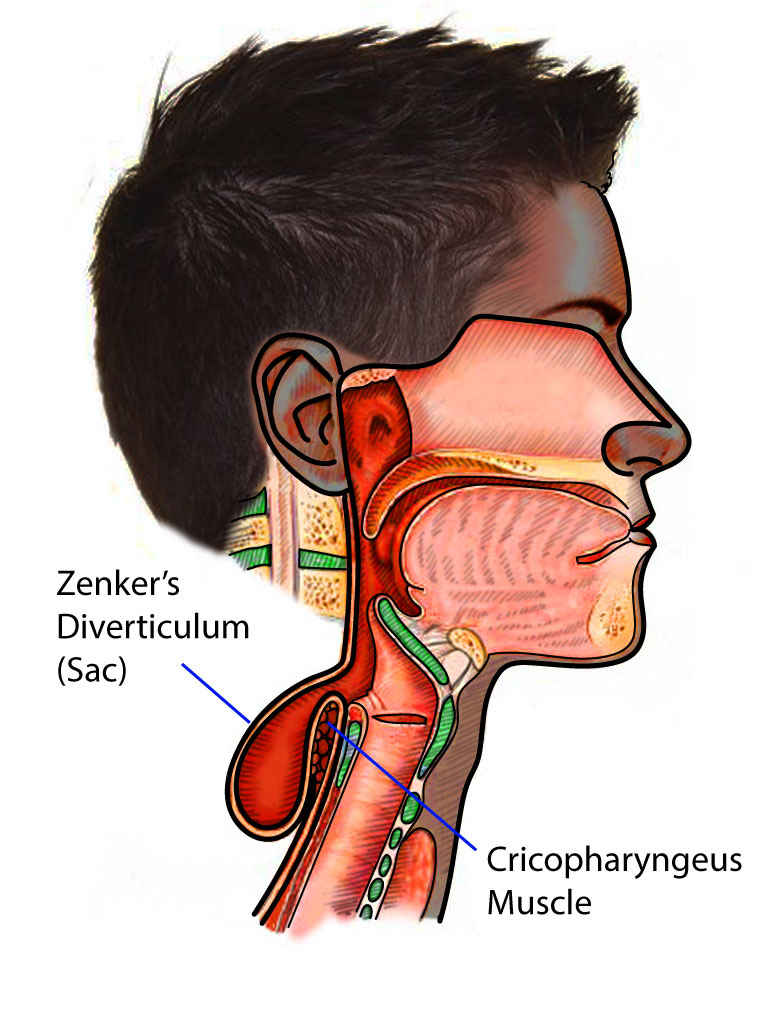
An esophageal diverticulum can also be categorized based on location as pharyngeal (Zenker) diverticula, mid-esophageal diverticula, and epiphrenic diverticula. Pharyngeal diverticula are considered false diverticula.[1][4] They usually occur in the hypopharynx where there is a weakness in the area known as Killian's triangle.[5] Killian's triangle is an area bound by the cricopharyngeus muscles and inferior pharyngeal constrictor muscles. These are usually formed by pulsion. A mid-esophageal diverticulum is usually true diverticulum and normally caused by traction from mediastinal inflammation. Epiphrenic diverticula are usually false diverticula located in the distal 10 cm of the esophagus. Similar to pharyngeal diverticula, they are also usually caused by pulsion from motility disorders that cause an increase in lower esophageal sphincter pressure such as achalasia.
An esophageal diverticulum can occur in individuals of all ages but overall are most common in adults. Zenker diverticulum is most common in the elderly.
Etiology
While the etiology of esophageal diverticula is not fully known, there is a thought that the diverticula form when there is an increase in luminal pressure, and the pressure pushes outward where there is a weakness in the lumen resulting in an outpouching of the mucosa.[2] It can also be seen as a complication from an esophageal motility disorder such as achalasia.
Epidemiology
Esophageal diverticula occur in less than 1% of the population[2]. They are found in approximately 1% to 3% of those presenting with dysphagia. It can occur in all ages but are typically diagnosed in the elderly. They are usually found more in men than in women.
Pathophysiology
There are different ways that esophageal diverticulum can form. Pulsion diverticula occur when there is an inadequate relaxation of either the upper or lower esophageal sphincter resulting in increased intraluminal pressure and subsequent herniation of the esophageal wall at an area of weakness.[1] These usually occur in achalasia and esophageal dysmotility. Traction diverticula occur when there is an external force on the esophageal wall that pulls on the esophageal wall creating a diverticulum. These usually occur in the middle esophagus due to mediastinal inflammation adhering to the esophagus and retracting it to form the defect. Traction diverticula may be seen in patients with tuberculosis, but in the USA, histoplasmosis is the most common cause.
In the lower esophagus, epiphrenic diverticulum is also known as pulsion diverticulum. The wall of the esophagus is pushed as a result of incoordination between the lower esophageal sphincter and the lower esophagus.
Zenker diverticulum occurs in between the muscle fibers where there is a weakness. A bulge will form and over time, the intraluminal pressure will enlarge the diverticulum. It does not appear that the cause of Zenker diverticulum is associated with incoordination between pharyngeal contraction and relaxation of the upper sphincter.
To date, there is no evidence that reflux plays a role in the etiology of esophageal diverticulum
Histopathology
The esophagus is composed of 4 layers; from the lumen going outward, they are the mucosa, submucosa, muscularis, and adventitia. True diverticula consist of all esophageal wall layers within the protrusion.[4] With false diverticula, only the mucosa and submucosa layers will be seen. Squamous cell carcinoma can rarely be found in conjunction with esophageal diverticula.
History and Physical
Symptomatic patients typically present with dysphagia.[4] Other presenting symptoms include regurgitation of intact food, aspiration pneumonia, weight loss, halitosis, and cough due to food being retained within the diverticulum. Patients rarely present with a mass in the neck. However, most patients are asymptomatic and may never be diagnosed with the diverticulum until they become symptomatic.
Besides dysphagia, other symptoms may include hypersalivation, cough, a sensation of food sticking at the back of the throat and regurgitation of food.
Evaluation
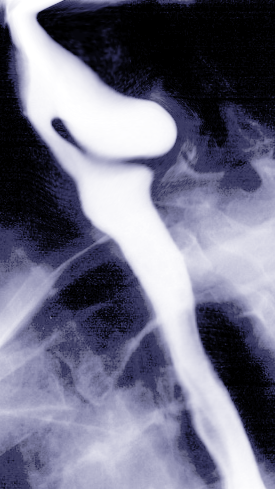
Most patients are diagnosed by barium esophagogram.[4] This study helps give information regarding location and size besides the diagnosis. Esophagogastroduodenoscopy can be done to confirm the diagnosis and is sometimes the initial diagnostic test. They can also be found incidentally on video swallow studies.
Endoscopy can be dangerous as there is a real risk of esophageal perforation.
Manometry studies are done to rule out motor disorders.
Treatment / Management
If patients are asymptomatic, then the diverticula are left intact.[4][6] This is usually the case in mid-esophageal and epiphrenic diverticula.[7] However, for symptomatic patients, there are surgical and endoscopic therapeutic options. This is more often seen in the pharyngeal diverticulum. Therapeutic options include diverticulectomy, diverticulopexy, and diverticular inversion, with or without myotomy, and myotomy alone.[8] Surgical options include open or laparoscopic approach. Most often, patients undergo minimally invasive myotomy and removal of the pouch endoscopically with either a soft or rigid endoscope.[9] If patients are not surgical candidates, then management with diet changes such as eating bland food and drinking water after every bite to help flush any food out of the diverticulum is recommended.
With Zenker diverticulum, surgery involves resection of the diverticulum and a small cricopharyngeal myotomy to lower sphincter pressure.
Today endoscopic treatments are gaining prominence over surgery. The procedure utilizes a rigid endoscope and dividing the connection between the esophagus and the diverticulum. In addition, a small myotomy is done.
Differential Diagnosis
Differential diagnoses include achalasia, esophageal cancer, esophageal stricture, gastroesophageal reflux, and presbyesophagus.[2] It is important to obtain a good history to help distinguish between these possible diagnoses.
Treatment Planning
Endoscopic myotomy (Dohlman Procedure) demands neck extension; therefore, it would not be an appropriate choice for patients with cervical stenosis who would not tolerate neck extension. The definitive management of symptomatic Zenker diverticulum is the surgical approach. The decision to use either an open or endoscopic transoral approach (rigid endoscope or a flexible endoscope) is made by clinicians based on several factors. The most important factors to be considered are 1. the ability to visualize the ZD and septum endoscopically, 2. patient's body habitus, 3. the ZD pouch feature in relation to the posterior wall, and 4. local expertise. Accordingly, patients with short necks decreased hyomental distance, and/or those patients with obesity are most often managed with an open approach. However, diverticula with less than 2 cm length are usually managed with endoscopic methods.
Transoral (endoscopic) approaches are categorized as minimally-invasive surgery and are associated with shorter procedural times, hospital stays, rapid resumption of oral intake, lower rate of complications. More significantly, in case of recurrence, the access would be easier. Endoscopic approaches are also associated with significantly high rates of symptom recurrence.
For patients who are considered poor surgical candidates, a flexible endoscopic approach is the procedure of choice. The main advantage of the flexible endoscopic approach is that it can be performed without general anesthesia. On the contrary, general anesthesia is required for open surgical and rigid endoscopic approaches. Hypothetically, a higher recurrence rate and the need for revision with a flexible endoscopy approach are expected. Bleeding and recurrence are more likely following flexible endoscopic techniques. However, dental injury and vocal fold palsy are expected as rare complications following the rigid endoscopy.[10][11][12]
Prognosis
Prognosis of these patients is dependent on their age and comorbidities as this will determine their surgical candidacy.[13] Risks and benefits need to be weighed. Most patients will have good results as far as immediate resolution of symptoms with surgical treatment with varied recurrence rates. However, surgical complications can be serious and need to be considered when deciding on whether to pursue surgical treatment and which surgical approach to pursue.
Complications
Esophageal diverticula complications are rare but include esophageal obstruction, perforation, and squamous cell carcinoma.[13]
Postoperative and Rehabilitation Care
Post-operative complications include bleeding, hematoma, infection, esophageal leaking at the repair site, fistula formation, mediastinal infection, esophageal perforation, esophageal stenosis, recurrent laryngeal nerve injury, and pneumomediastinum.[13] The rate of these complications will, of course, depend on the surgical or endoscopic approach and skill of the surgeon.
Pearls and Other Issues
Esophageal diverticula are a rare finding in the esophagus. However, it is something to consider in a patient with dysphagia and regurgitation, especially in the elderly. Most often, workup begins with a barium esophagogram and can be confirmed by manometry or endoscopy. It is important to consider this diagnosis when performing endoscopy as esophageal perforation is at increased risk when pushing the scope blindly into the pouch.
Enhancing Healthcare Team Outcomes
The diagnosis and management of esophageal diverticulum is best done with an interprofessional team. Most patients have no symptoms and the diverticulum is often discovered incidentally during the workup of another disorder. Symptomatic patients may present with non-specific complaints and it is vital to refer the patient to a gastroenterologist for workup. The treatment of esophageal diverticula is continuing to evolve and thus, patient education is key.
It is important for the diagnosing physician, whether it be the patient's primary care physician or gastroenterologist, to discuss the diagnosis with the patient and its implications prior to deciding on a treatment plan. A treatment plan will need to involve careful consideration of the patient's comorbidities prior to consultation with a surgeon.
Communication between the primary care clinicians, the gastroenterologist, and thoracic surgery is key to obtaining the best outcomes.