[1]
Shi D, Bai J, Zhang L, Wang X. The "Hand as Foot" teaching method in axillary artery anatomy. Asian journal of surgery. 2022 Feb:45(2):800-801. doi: 10.1016/j.asjsur.2021.12.001. Epub 2021 Dec 29
[PubMed PMID: 34973859]
[2]
Yang K, Lee H, Choi IJ, Jeong W, Kim HT, Wei Q, Lee JH. Topography and Anatomical Variations of the Axillary Artery. BioMed research international. 2021:2021():6393780. doi: 10.1155/2021/6393780. Epub 2021 May 24
[PubMed PMID: 34124252]
[3]
Stowell JT, McComb BL, Mendoza DP, Cahalane AM, Chaturvedi A. Axillary Anatomy and Pathology: Pearls and "Pitfalls" for Thoracic Imagers. Journal of thoracic imaging. 2022 May 1:37(3):W28-W40. doi: 10.1097/RTI.0000000000000639. Epub 2022 Feb 10
[PubMed PMID: 35142752]
[4]
Loukas M, du Plessis M, Owens DG, Kinsella CR Jr, Litchfield CR, Nacar A, Lu O, Tubbs RS. The lateral thoracic artery revisited. Surgical and radiologic anatomy : SRA. 2014 Aug:36(6):543-9. doi: 10.1007/s00276-013-1234-x. Epub 2013 Nov 27
[PubMed PMID: 24281130]
[5]
Jaiswal LS, Neupane D, Yadav P. Rare variation of the right brachial artery. ANZ journal of surgery. 2022 May:92(5):1281-1282. doi: 10.1111/ans.17291. Epub 2021 Oct 17
[PubMed PMID: 34661957]
[6]
Olinger A, Benninger B. Branching patterns of the lateral thoracic, subscapular, and posterior circumflex humeral arteries and their relationship to the posterior cord of the brachial plexus. Clinical anatomy (New York, N.Y.). 2010 May:23(4):407-12. doi: 10.1002/ca.20958. Epub
[PubMed PMID: 20235185]
[7]
Mills NL, Dupin CL, Everson CT, Leger CL. The subscapular artery: an alternative conduit for coronary bypass. Journal of cardiac surgery. 1993 Jan:8(1):66-71
[PubMed PMID: 8422491]
[8]
Rodríguez-Niedenführ M, Burton GJ, Deu J, Sañudo JR. Development of the arterial pattern in the upper limb of staged human embryos: normal development and anatomic variations. Journal of anatomy. 2001 Oct:199(Pt 4):407-17
[PubMed PMID: 11693301]
[9]
Benes M, Kachlik D, Belbl M, Kunc V, Havlikova S, Whitley A, Kunc V. A meta-analysis on the anatomical variability of the brachial plexus: Part I - Roots, trunks, divisions and cords. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2021 Nov:238():151751. doi: 10.1016/j.aanat.2021.151751. Epub 2021 Apr 30
[PubMed PMID: 33940116]
Level 1 (high-level) evidence
[10]
Fakoya AOJ, Aguinaldo E, Velasco-Nieves NM, Vandeveer ZT, Morales-Marietti N, Mathew S, Afolabi AG, McCracken T. Unusual Splitting of Medial Cord of the Right Brachial Plexus and Its Relation to the Axillary Artery and Subscapular Artery: A Case Report. Open access Macedonian journal of medical sciences. 2019 Jun 30:7(12):2006-2009. doi: 10.3889/oamjms.2019.561. Epub 2019 Jun 30
[PubMed PMID: 31406546]
Level 3 (low-level) evidence
[12]
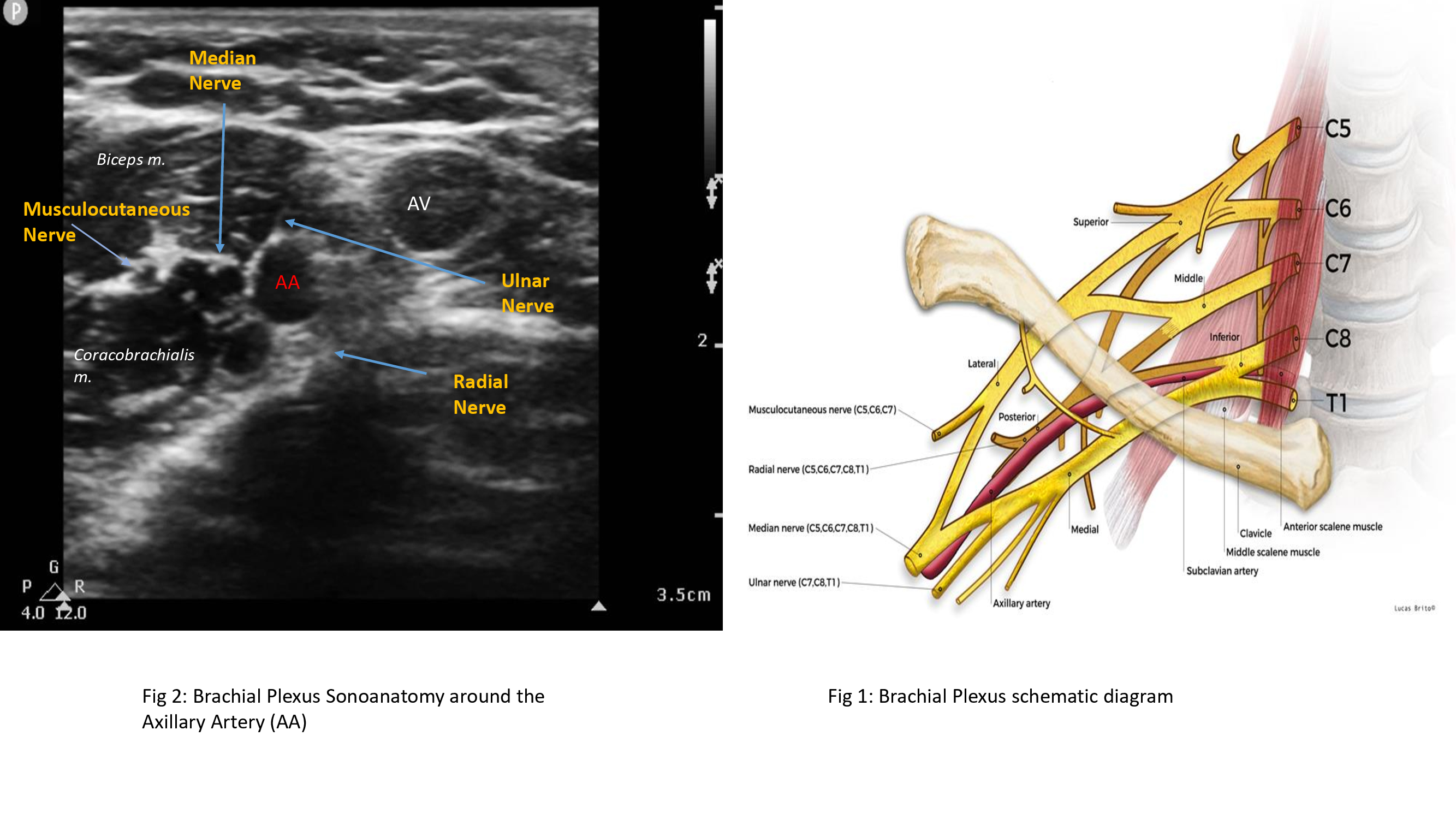
Gili S, Abreo A, GóMez-Fernández M, Solà R, Morros C, Sala-Blanch X. Patterns of Distribution of the Nerves Around the Axillary Artery Evaluated by Ultrasound and Assessed by Nerve Stimulation During Axillary Block. Clinical anatomy (New York, N.Y.). 2019 Jan:32(1):2-8. doi: 10.1002/ca.23225. Epub 2018 Oct 20
[PubMed PMID: 30341965]
[13]
Burzotta F, Brancati MF, Porto I, Saffioti S, Aurigemma C, Niccoli G, Leone AM, Coluccia V, Crea F, Trani C. Comparison of Right and Left Upper Limb Arterial Variants in Patients Undergoing Bilateral Transradial Procedures. Circulation. Cardiovascular interventions. 2015 Dec:8(12):e002863. doi: 10.1161/CIRCINTERVENTIONS.115.002863. Epub
[PubMed PMID: 26643739]
[15]
Rogovskyi VM, Gybalo RV, Lurin IA, Sivash YY, Oklei DV, Taraban IA. A Case of Surgical Treatment of a Gunshot Wound to the Left Scapular Region With Damage to the Distal Axillary and Proximal Brachial Arteries. World journal of surgery. 2022 Jul:46(7):1625-1628. doi: 10.1007/s00268-022-06577-y. Epub 2022 Apr 28
[PubMed PMID: 35484404]
Level 3 (low-level) evidence
[16]
Tetik O, Yilik L, Besir Y, Can A, Ozbek C, Akcay A, Gurbuz A. Surgical treatment of axillary artery aneurysm. Texas Heart Institute journal. 2005:32(2):186-8; discussion 185
[PubMed PMID: 16107110]
[17]
Bertoglio L, Grandi A, Melloni A, Kahlberg A, Melissano G, Chiesa R. Percutaneous AXillary Artery (PAXA) Access at the First Segment During Fenestrated and Branched Endovascular Aortic Procedures. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2020 Jun:59(6):929-938. doi: 10.1016/j.ejvs.2020.01.027. Epub 2020 Feb 20
[PubMed PMID: 32089506]
[18]
Branzan D, Steiner S, Haensig M, Scheinert D, Schmidt A. Percutaneous Axillary Artery Access for Endovascular Treatment of Complex Thoraco-abdominal Aortic Aneurysms. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2019 Sep:58(3):344-349. doi: 10.1016/j.ejvs.2019.01.011. Epub 2019 Jul 30
[PubMed PMID: 31375342]
[19]
Agrusa CJ, Connolly PH, Ellozy SH, Schneider DB. Safety and Effectiveness of Percutaneous Axillary Artery Access for Complex Aortic Interventions. Annals of vascular surgery. 2019 Nov:61():326-333. doi: 10.1016/j.avsg.2019.05.046. Epub 2019 Aug 5
[PubMed PMID: 31394224]
[20]
Stone MA, Ihn HE, Gipsman AM, Iglesias B, Minneti M, Noorzad AS, Omid R. Surgical anatomy of the axillary artery: clinical implications for open shoulder surgery. Journal of shoulder and elbow surgery. 2021 Jun:30(6):1266-1272. doi: 10.1016/j.jse.2020.09.018. Epub 2020 Oct 15
[PubMed PMID: 33069906]
[21]
Bucci G, Lucar-López G, Sanchez-Gonzalez J, Malagelada F, Palencia Lopez J, Guevara-Noriega KA. Axillary artery injury and brachial plexus palsy as a complication of proximal humerus fractures. Journal of orthopaedics. 2017 Sep:14(3):340-341. doi: 10.1016/j.jor.2017.06.001. Epub 2017 Jun 24
[PubMed PMID: 28706376]
[22]
Michalakis D, Lerais JM, Goffette P, Royer V, Brenot R, Kastler B. [True isolated atherosclerotic aneurysm of the axillary artery]. Journal de radiologie. 2003 Sep:84(9):1016-9
[PubMed PMID: 13679756]
[23]
Szuchmacher PH, Freed JS. Axillary aneurysms. New York state journal of medicine. 1980 Apr:80(5):795-6
[PubMed PMID: 6930558]
[24]
Branco BC, Boutrous ML, DuBose JJ, Leake SS, Charlton-Ouw K, Rhee P, Mills JL Sr, Azizzadeh A. Outcome comparison between open and endovascular management of axillosubclavian arterial injuries. Journal of vascular surgery. 2016 Mar:63(3):702-9. doi: 10.1016/j.jvs.2015.08.117. Epub 2015 Oct 23
[PubMed PMID: 26506937]
[25]
Charmode S, Mehra S, Kushwaha S. Revisiting the Surgical Approaches to Decompression in Quadrilateral Space Syndrome: A Cadaveric Study. Cureus. 2022 Feb:14(2):e22619. doi: 10.7759/cureus.22619. Epub 2022 Feb 26
[PubMed PMID: 35371758]