Continuing Education Activity
Astrocytoma originates in astrocytes, which are a kind of glial cells in the cerebrum which are star-shaped. It is the most common glioma, usually affecting the brain and sometimes the spinal cord. Amongst brain tumors, glial tumors comprise 60% of the tumors. They are a common cause of mortality and morbidity in both the young and old both. Astrocytomas are one of the common brain tumors. To avoid the high morbidity and mortality associated with this condition, they must be promptly diagnosed and treated. This article reviews the evaluation and treatment of astrocytoma and highlights the role of the interprofessional team in evaluating and treating patients with this condition.
Objectives:
- Identify the etiology of astrocytoma.
- Outline the appropriate evaluation of astrocytoma.
- Review the management options available for astrocytoma.
- Describe the interprofessional team strategies for improving care, coordination and communication in astrocytoma and improve outcomes.
Introduction
Astrocytoma originates in astrocytes, which are a kind of glial cells in the cerebrum which are star-shaped. It is the most common glioma, usually affecting the brain and sometimes the spinal cord. Amongst brain tumors, glial tumors comprise 60% of the tumors. They are a common cause of mortality and morbidity in both the young and old.
Etiology
No underlying cause has been identified for the majority of primary brain tumors, the only established risk factor being exposure to ionizing radiation. Evidence for an association with other factors like exposure to electromagnetic fields (cellular telephones), head injury, or occupational risk factors is unproven. A minority of patients have a family history of brain tumors. Children who receive prophylactic radiation for acute lymphocytic leukemia (ALL) may have 22 times more chance of developing central nervous system malignancy within about 5 to 10 years. It has been shown that pituitary adenoma radiation therapy carries 16x more risk of glioma development.[1] There is a genetic susceptibility to glioma development, for example, in diseases like Turcot syndrome, p53 mutations (Li - Fraumeni), and NF1 syndrome. Amongst low-grade astrocytomas, about 66% demonstrate p53 mutations.[2]
Epidemiology
Age-standardized rate of incidence of gliomas was 4.7/100,000 person-years.
Mortality/Morbidity
Typical survival ranges are:
- WHO grade I (pilocytic astrocytomas) - more than 10 years
- WHO grade II (low-grade diffuse astrocytomas) - more than 5 years
- WHO grade III (anaplastic astrocytomas) - about 2 to 5 years
- WHO grade IV (glioblastoma) - about 1 year
Race
Minimal racial differences have been found
Gender
No gender dominance in pilocytic astrocytomas. A male: female ratio 1.18:1 in low-grade astrocytomas is there. In anaplastic astrocytoma, there is a substantial male dominance, with a male: female incidence being 1.87:1.
Age
The likelihood of pilocytic astrocytoma is increased in the first 2 decades. Whereas in the age group of 30-40, lowgrade astrocytomas are predominant, which comprise about one-fourth of adult cases.
The distribution of lowgrade astrocytomas is as follows:
- 10%: less than 20 years
- 60%: 20 to 45 years
- 30%: greater than 45 years
Anaplastic astrocytoma has a mean age of about 40 years.
Pathophysiology
The local effects of astrocytoma are a result of multiple mechanisms. These include direct invasion and competition for oxygen, leading to hypoxic injury to normal brain parenchyma. Apart from this, free radicals, neurotransmitters, and inflammatory mediators are also responsible for disturbing the homeostasis. The mass effect due to the tumor is also responsible for the various clinical signs and symptoms.
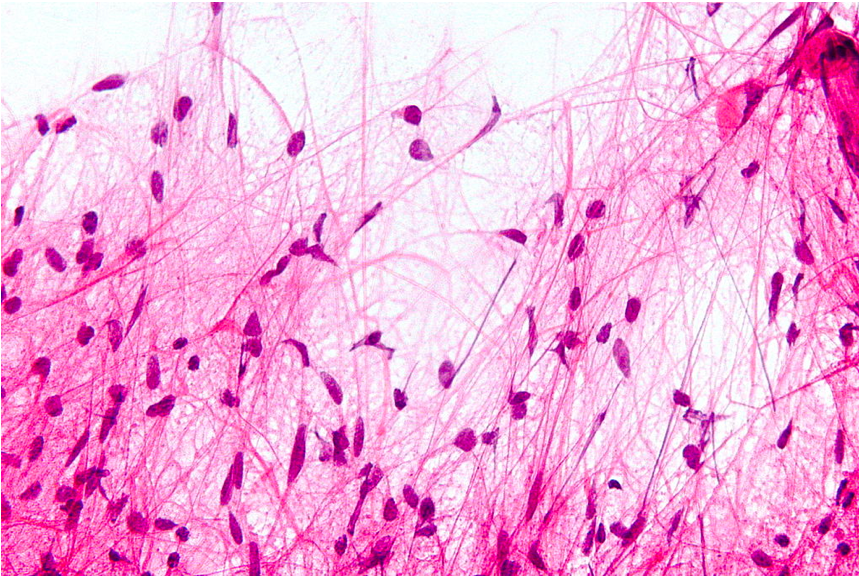
Histopathology
Common Types Pilocytic Astrocytoma
- It is benign in nature
- Has cystic consistency
- Location is mostly infratentorial
- Presents classically in childhood
- Can be resected surgically
- Variant: Pilomyxoid astrocytoma
Diffuse Astrocytoma
- Grade II
- Usually seen in adults
- May progress to glioblastoma
Anaplastic Astrocytoma
- Grade III
- Also usually seen in adults
- There is a lack of endothelial proliferation
Glioblastoma
- Commonest malignant brain tumor
- Peak age is around 65 years
- Very bad prognostication
- Variants: Giant cell glioblastoma, Gliosarcoma
Uncommon Types
Pleomorphic Xanthoastrocytoma (PXA)
- Prognosis is usually good
- Age group affected: Children & adults (young)
- Has big lipidized cells
- May mimic malignant tumor
Subependymal Giant Cell Astrocytoma(SEGCA)
- Located mostly intraventricularly
- Benign in nature
- Affects the adolescent age group
- Associated with Tuberous sclerosis
Gliomatosis Cerebri
- Old term, used for extensive & diffuse astrocytomas
- Not a distinct entity since 2016
- Radiological evidence of > 3 lobe involvement is required, bilaterally
- WHO grade III
- Division into 2 types possible on the basis of solid component presence:
1. Type 1 GC: No IDH 1/2 mutation, diffusely growing
2. Type 2 GC: IDH 1 mutation +, solid component present
- Genetically overlaps diffuse astrocytic gliomas, glioblastoma & oligodendrogliomas
H3 K27M Mutant Diffuse Midline Glioma
- High-grade
- Location: midline including spinal cord, brainstem & thalamus
- Adolescents & children are mostly involved
- DPIG(Diffuse pontine intrinsic glioma) is included
- New entry after 2016 WHO classification
- Poor prognosis is usually there when:
- Absence of EGFR amplification
- Presence of unmethylated MGMT promoter
- Enhancement in MRI: may/may not be present
- Histologically may range from minimum hypercellularity to full-blown glioblastoma
Gliosarcoma
- WHO considers it as a variant of glioblastoma
- It is quite rare, with only about 200 case reports
- Has Glioblastoma & sarcoma components(fibroblastic, osseous, cartilage, smooth & striated muscle, fat cells)
- Similar to glioblastomas, it is usually found in temporal lobe
- Prognositicallly like glioblastoma
Immunohistochemistry:
- Astrocytic component is glial fibrillary acidic protein (GFAP) positive & spindle cell negative
- Smooth muscle part (Gliomyosarcoma ) is Smooth muscle antibody (SMA) & factor VIII positive
Gliofibroma
- It is very rare
- Usually found in children
- Has fibroblastic part, which is non-malignant
History and Physical
History
Symptoms can be divided into two categories: general & focal. General symptoms include headache (usually early morning), nausea, vomiting, cognitive difficulties, personality changes, and gait disorders. Localizing symptoms include seizures, aphasia, or visual field defects. A visual field defect is often unnoticed by the patient, may be revealed after it leads to injury such as automobile accidents. Seizures occur in about 90% of patients with low-grade glioma.
Physical
Always do a full neurological examination. All signs should be well elicited as they have localizing features. For example, a positive Babinski's sign on the right side suggests a left lobe pathology. Similarly, the demarcation of sensory levels will help in localizing the spinal cord malignancy level. Cranial nerve palsies are a good sign for localizing intracranial locations. Further confirmation of the location of tumors should be done by neurological imaging.
Evaluation
Imaging Studies
Neuroimaging is the only test necessary to diagnose a brain tumor. MRI is the best imaging for the same. Gadolinium contrast-enhanced MR imaging should be used whenever possible. If there is any contraindication for MRI, such as joint implants or pacemakers in situ, computed tomography or CT may be done. Lower-grade gliomas aren't contrasting enhancing, so fluid-attenuated inversion recovery (FLAIR) sequences of MRI are done. If a tumor is found, a neurosurgeon must perform a biopsy on it. This simply involves the removal of a small amount of tumor tissue, which is then sent to a neuropathologist for examination and grading. CT appearance of lowgrade astrocytomas is also generally not very definitive. They are homogeneous, not well defined, and appear as poorly defined and non-contrast enhancing lesions. In anaplastic astrocytomas, there may be some contrast enhancement. There may be a possible metastatic disease; hence whole-body imaging should also be considered to look for an alternate primary.
On MRI, T2 hyperintensity is seen in astrocytomas, whereas on T1, there is isointensity. Tumor vascularity is very important; hence new techniques are being developed to identify it. These include ASL (arterial spin labeling) and DCE (dynamic contrast enhancement) MRI. Functional MRI is an upcoming imaging modality. It is useful pre-surgery to demarcate various areas of the brain on the basis of functionality. Other modalities include PET scan, MRS (magnetic resonance spectroscopy), and perfusion. These may give information about metabolic action in the tumor, the blood flow characteristics, and the constitution of the tumor. Using this, it can be determined whether the lesion is progressive or necrosed after chemotherapy and radiotherapy.
Treatment / Management
WHO classification(2016) classifies diffuse astrocytomas as grades II, III, and IV. Grade I infiltrating astrocytoma is not mentioned. It is based on the following four characteristics: 1. Nuclear atypia: nuclear pleomorphism and hyperchromasia 2. Mitoses:
- Has to be unequivocal
- Ki67 proliferation index is used to separate grade II tumors from grade III
3. Microvascular proliferation:
- Glomeruloid type - commoner, prognostically lesser significance as it's found in lower-grade gliomas (like pilocytic astrocytoma) also
- Endothelial proliferation - in the large vessel lumen. It is less common and has more association with high-grade gliomas
4. Necrosis:
- Coagulative necrosis
- Pseudopalisading necrosis
WHO Histological Grading: Diffuse Astrocytomas
- Grade II (diffuse astrocytoma): nuclear atypia alone
- Grade III (anaplastic astrocytoma): nuclear atypia + focal/dispersed anaplasia. There are prominent proliferation activity and mitoses
- Grade IV (glioblastoma): nuclear atypia, mitoses, microvascular proliferation or necrosis
WHO Histological Grading: Localized Astrocytomas
- Pilocytic astrocytoma: corresponding to WHO-grade I
- Doesn't recommend definitive grade allotment yet for pilomyxoid astrocytoma
- SEGCA (subependymal giant cell astrocytoma): Grade I
- Pleomorphic xanthoastrocytoma: grade II and anaplastic pleomorphic:[3] Grade III[4]
Glioma Treatment Recommendations Based on Grade
Grade I (pilocytic astrocytomas)
- Uncommon, typically noninvasive and are considered benign. Potentially curable by surgery but if surgical removal is not possible completely, radiotherapy or expectant management is used
Grade II (low-grade infiltrative astrocytomas, oligodendroglioma, mixed gliomas)
- Surgery is recommended with maximal safe resection
- Unfavorable prognostic factors: age > 40 years, dimension ≥6 cm, crossing midline and presence of neurologic deficit before resection; 3 or more factors are high risk
- Low-risk, < 40-year patients: observation
- High-risk patients: fractionated external-beam radiotherapy (EBRT) or adjuvant chemotherapy[5]
- The standard radiation dose for low-grade astrocytomas is 45-54 Gy, delivered in 1.8 to 2.0 Gy fractions
- Adjuvant therapy includes temozolomide 150 to 200 mg/m^2/day orally on days 1-5 of a 28-day cycle (6-8 cycles)
- Recurrences or progressive, low-grade disease (previously untreated): Temozolomide 75 mg/m^2 PO daily on days 1-21 or 150 to 200 mg/m^2 PO on days 1 to 5 of a 28-d cycle until disease progression or for a maximum of 24 cycles
- Postoperative radiation therapy is often employed for unresectable, residual, or recurrent tumor
- Chemotherapy is often used for low-grade oligodendrogliomas, particularly tumors with the 1p19q deletion, which is a marker for tumor susceptibility to chemotherapy
Grade III (anaplastic astrocytoma or oligoastrocytoma)
- Standard of care: surgical resection followed by EBRT (60 Gy in 30 to 35 fractions) and adjuvant temozolomide, 75 mg/m^2/day orally on days 1 to 42, usually 1 to 1.5 hours before radiation
- Post–radiation therapy: Continue temozolomide at higher doses of 150 to 200 mg/m^2/day PO on days 1 to 5 every 28 days or
- PCV (procarbazine, lomustine, vincristine): lomustine (CCNU) 90 to 130 mg/m^2 PO on day 1 plus procarbazine 60 to 75 mg/m^2 PO on days 8 to 21 plus vincristine 1.4 mg/m^2 IV (not to exceed 2 mg/dose) on days 8 and 29; administer every 6 weeks for up to 4 cycles with deferred radiotherapy
Grade IV (glioblastoma):
- Standard of care is surgical resection followed by EBRT (60 Gy in 30 to 35 fractions) and adjuvant temozolomide 75 mg/m^2/day orally on days 1 to 42, usually 1 to 1.5 hours before radiation[4][6]
- Postradiation therapy: Continue temozolomide at higher doses of 150 to 200 mg/m^2/day PO on days 1 to 5 every 28 days[7]
Recommendations for recurrent tumors: reoperation, carmustine wafers, and alternate chemotherapeutic regimens. Re-radiation is rarely helpful. Bevacizumab, a humanized VEGF monoclonal antibody, has activity in recurrent glioblastoma, increasing progression-free survival & reducing peritumoral edema & glucocorticoid use. Recurrent glioblastoma treatment decisions must take into consideration factors such as previous therapy, time to relapse, performance status, and quality of life. Whenever possible, patients with recurrent disease should be enrolled in clinical trials.
How to Approach
As with the rest of the malignancies, a multimodal treatment approach is undertaken, including surgical, medical, and radiation oncology.
Low-grade astrocytomas: No clear superiority of any particular modality is known. As these low-grade tumors can be quite indolent, questions arise about the risk-benefit ratio of undertaking any intervention. A study by Ishkanian et al. demonstrated the efficacy of adjuvant radiotherapy for pilocytic astrocytoma (WHOgrade I), it prolongs PFS (progression-free survival) at 5 and 10 years as compared to observation.[8] Overall, survivals were equal, however.
Grade 2 astrocytoma: Radiotherapy and adjuvant chemotherapy are better than only radiotherapy. A trial showed that chemotherapy with vincristine, procarbazine, and lomustine following radiotherapy leads to better 10 years PFS (51% v/s 21%).[9]
Anaplastic astrocytomas: multimodal therapy is incorporated, including surgery, radiation, and chemotherapy(adjuvant temozolomide). Data regarding concurrent temozolomide is lacking, although some studies showed improved survival (46% vs. 29%). IDH( Isocitrate Dehydrogenase ) mutation is also associated with improved 5-year survival (79% vs. 22%).[10] Response to chemotherapy is better in Anaplastic astrocytomas than glioblastomas. In the event of recurrence, temozolomide shows better response. Nitrosourea treated recurrent tumors showed about 35% response with temozolomide. Moreover, 6month survivals were also better(46% v/s 31%).[3] Adjuvant carmustine also shows a slight survival benefit.
Prophylactically starting antiepileptics is controversial. Those who have a complaint of seizure should be started on antiepileptics. For seizures, the patient is usually started on levetiracetam, topiramate, lamotrigine, valproic acid, and lacosamide. These drugs interfere less with the hepatic microsomal enzyme system. Other drugs such as phenytoin and carbamazepine are used less frequently as they are potent enzyme inducers that can interfere with both glucocorticoid metabolism and metabolism of chemotherapeutic agents. Corticosteroids are also used as they lead to excellent symptomatic relief due to their anti-inflammatory action. This leads to a decrease in mass effect. Dexamethasone is the glucocorticoid of choice because of its low mineralocorticoid activity. Initial doses are typically 12-16 mg/d in divided doses orally or IV ( both are equivalent). Concurrent prophylaxis for gastrointestinal ulcers should be prescribed with corticosteroid administration.
Surgical Care
Surgery provides to remove/debulk the tumor. Moreover, histological diagnosis is made possible by the tissue biopsy provided by the surgeon. Other symptom-relieving procedures include ICT (intracranial tension), reducing procedures like VP shunting, EVD insertion, etc. It has been shown that complete resection (>98% based on volumetric MRI) improves median survival compared with subtotal resection (13 vs. 8.8 mo).[11] For low-grade gliomas, supratotal resection is also advocated (i.e., removal of tissue beyond the MRI-defined abnormalities), suggesting an increase in overall survival with this strategy.[12]
Other Medications Summary
Venous thromboembolic disease occurs in 20% to 30% of patients with high-grade gliomas and brain metastasis; hence prophylactic anticoagulants should be used during hospitalization and in non-ambulatory patients. Those who have had deep venous thrombosis (DVT) or pulmonary embolus can receive safely therapeutic doses of anticoagulation without increasing risk for hemorrhage into the tumor.
Antineoplastic Agent
Temozolomide (alkylating agent): Oral alkylating agent converted to MTIC at physiologic pH; 100% bioavailable; approximately 35% crosses the blood-brain barrier.
mTOR inhibitors are also proposed for the treatment of grade 1 astrocytomas.
Differential Diagnosis
- Glioblastoma multiforme
- Brain metastasis
- Brain abscess
- Oligodendroglioma
- Encephalitis
- Multiple sclerosis
- Primary CNS lymphoma
- Toxoplasmosis
Staging
Staging is not done in astrocytoma. Grading only is done, as described previously, which is a determinant of prognosis.
Prognosis
It is favorable for low-grade tumors, with survival times approaching 7 to 8 years after surgery. In anaplastic astrocytoma, therapy focuses on improvement in symptoms. Radiotherapy of partially resected tumors increases postoperative survival rates. Survival rates after post-surgery radiation are nearly double that of only surgical intervention (5 vs. 2.2 years).
Genetics also plays a role in determining the prognosis of a particular form of a tumor. Oligodendroglioma with Ch 1p19q changes responds better to PCV [procarbazine, CCNU (lomustine), and vincristine]. Genetics is the upcoming field for individualized tumor therapies.
Kallikrein levels are associated with patient prognosis:[13]
- Increased KLK6 / KLK7-IR leads to poor outcomes
- Immunoreaction with KLK6/9 decreased survival
Complications
Neurosurgical interventions always have an added risk of surgical complications. Complications of chemotherapy and radiotherapy are also seen, as with the treatment of cancers, but efficient drugs have been devised for the proper management of these complications.
Deterrence and Patient Education
Patients must understand that new strides are being achieved in oncology with each passing day. Any fear or query must be addressed bravely with the full faith in his/her clinician.
Enhancing Healthcare Team Outcomes
Early initiation of treatment after consultation with the oncology team comprising of medical oncologists, surgical oncologists, radiation oncologists, radiologists, and pathologists is a must. Interdisciplinary collaboration with other team members, including anesthetists, nurses, pharmacists, and surgical technologists are paramount for optimal patient care.