[1]
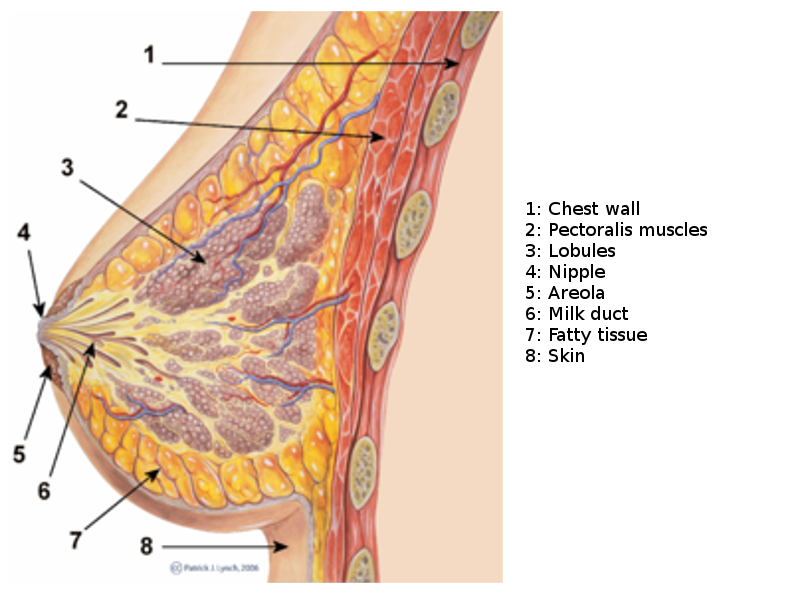
Pandya S, Moore RG. Breast development and anatomy. Clinical obstetrics and gynecology. 2011 Mar:54(1):91-5. doi: 10.1097/GRF.0b013e318207ffe9. Epub
[PubMed PMID: 21278507]
[2]
Inman JL, Robertson C, Mott JD, Bissell MJ. Mammary gland development: cell fate specification, stem cells and the microenvironment. Development (Cambridge, England). 2015 Mar 15:142(6):1028-42. doi: 10.1242/dev.087643. Epub
[PubMed PMID: 25758218]
[3]
Macias H, Hinck L. Mammary gland development. Wiley interdisciplinary reviews. Developmental biology. 2012 Jul-Aug:1(4):533-57
[PubMed PMID: 22844349]
[4]
Musumeci G, Castrogiovanni P, Szychlinska MA, Aiello FC, Vecchio GM, Salvatorelli L, Magro G, Imbesi R. Mammary gland: From embryogenesis to adult life. Acta histochemica. 2015 May-Jun:117(4-5):379-85. doi: 10.1016/j.acthis.2015.02.013. Epub 2015 Mar 20
[PubMed PMID: 25800977]
[5]
Hassiotou F, Geddes D. Anatomy of the human mammary gland: Current status of knowledge. Clinical anatomy (New York, N.Y.). 2013 Jan:26(1):29-48. doi: 10.1002/ca.22165. Epub 2012 Sep 19
[PubMed PMID: 22997014]
[6]
Misery L, Talagas M. Innervation of the Male Breast: Psychological and Physiological Consequences. Journal of mammary gland biology and neoplasia. 2017 Jun:22(2):109-115. doi: 10.1007/s10911-017-9380-0. Epub 2017 May 27
[PubMed PMID: 28551701]
[7]
Anderson WF, Devesa SS. In situ male breast carcinoma in the Surveillance, Epidemiology, and End Results database of the National Cancer Institute. Cancer. 2005 Oct 15:104(8):1733-41
[PubMed PMID: 16138363]
[8]
Duivenvoorden HM, Rautela J, Edgington-Mitchell LE, Spurling A, Greening DW, Nowell CJ, Molloy TJ, Robbins E, Brockwell NK, Lee CS, Chen M, Holliday A, Selinger CI, Hu M, Britt KL, Stroud DA, Bogyo M, Möller A, Polyak K, Sloane BF, O'Toole SA, Parker BS. Myoepithelial cell-specific expression of stefin A as a suppressor of early breast cancer invasion. The Journal of pathology. 2017 Dec:243(4):496-509. doi: 10.1002/path.4990. Epub 2017 Oct 31
[PubMed PMID: 29086922]
[9]
Visvader JE, Stingl J. Mammary stem cells and the differentiation hierarchy: current status and perspectives. Genes & development. 2014 Jun 1:28(11):1143-58. doi: 10.1101/gad.242511.114. Epub
[PubMed PMID: 24888586]
Level 3 (low-level) evidence
[10]
Zhu W, Nelson CM. Adipose and mammary epithelial tissue engineering. Biomatter. 2013 Jul-Sep:3(3):. doi: 10.4161/biom.24630. Epub 2013 Apr 1
[PubMed PMID: 23628872]
[11]
Sigl V, Jones LP, Penninger JM. RANKL/RANK: from bone loss to the prevention of breast cancer. Open biology. 2016 Nov:6(11):
[PubMed PMID: 27881737]
[12]
Stone K, Wheeler A. A Review of Anatomy, Physiology, and Benign Pathology of the Nipple. Annals of surgical oncology. 2015 Oct:22(10):3236-40. doi: 10.1245/s10434-015-4760-4. Epub 2015 Aug 5
[PubMed PMID: 26242366]
[13]
Val-Bernal JF, Diego C, Rodriguez-Villar D, Garijo MF. The nipple-areola complex epidermis: a prospective systematic study in adult autopsies. The American Journal of dermatopathology. 2010 Dec:32(8):787-93. doi: 10.1097/DAD.0b013e3181ddbec5. Epub
[PubMed PMID: 20802299]
Level 1 (high-level) evidence
[14]
Hovey RC, Aimo L. Diverse and active roles for adipocytes during mammary gland growth and function. Journal of mammary gland biology and neoplasia. 2010 Sep:15(3):279-90. doi: 10.1007/s10911-010-9187-8. Epub 2010 Aug 19
[PubMed PMID: 20717712]
[15]
Muschler J, Streuli CH. Cell-matrix interactions in mammary gland development and breast cancer. Cold Spring Harbor perspectives in biology. 2010 Oct:2(10):a003202. doi: 10.1101/cshperspect.a003202. Epub 2010 Aug 11
[PubMed PMID: 20702598]
Level 3 (low-level) evidence
[16]
Schedin P, Mitrenga T, McDaniel S, Kaeck M. Mammary ECM composition and function are altered by reproductive state. Molecular carcinogenesis. 2004 Dec:41(4):207-20
[PubMed PMID: 15468292]
[17]
Brinkman RJ, Hage JJ. Andreas Vesalius' 500th Anniversary: First Description of the Mammary Suspensory Ligaments. World journal of surgery. 2016 Sep:40(9):2144-8. doi: 10.1007/s00268-016-3481-6. Epub
[PubMed PMID: 26943658]
[18]
Betterman KL, Paquet-Fifield S, Asselin-Labat ML, Visvader JE, Butler LM, Stacker SA, Achen MG, Harvey NL. Remodeling of the lymphatic vasculature during mouse mammary gland morphogenesis is mediated via epithelial-derived lymphangiogenic stimuli. The American journal of pathology. 2012 Dec:181(6):2225-38. doi: 10.1016/j.ajpath.2012.08.035. Epub 2012 Oct 11
[PubMed PMID: 23063660]
[19]
Need EF, Atashgaran V, Ingman WV, Dasari P. Hormonal regulation of the immune microenvironment in the mammary gland. Journal of mammary gland biology and neoplasia. 2014 Jul:19(2):229-39. doi: 10.1007/s10911-014-9324-x. Epub 2014 Jul 4
[PubMed PMID: 24993978]
[20]
Atashgaran V, Wrin J, Barry SC, Dasari P, Ingman WV. Dissecting the Biology of Menstrual Cycle-Associated Breast Cancer Risk. Frontiers in oncology. 2016:6():267. doi: 10.3389/fonc.2016.00267. Epub 2016 Dec 26
[PubMed PMID: 28083513]
[21]
Onstad M, Stuckey A. Benign breast disorders. Obstetrics and gynecology clinics of North America. 2013 Sep:40(3):459-73. doi: 10.1016/j.ogc.2013.05.004. Epub 2013 Jul 24
[PubMed PMID: 24021252]
[22]
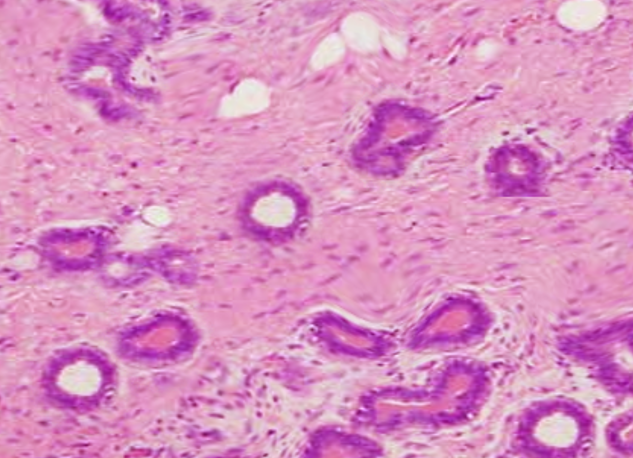
Tucker DK, Foley JF, Hayes-Bouknight SA, Fenton SE. Preparation of High-quality Hematoxylin and Eosin-stained Sections from Rodent Mammary Gland Whole Mounts for Histopathologic Review. Toxicologic pathology. 2016 Oct:44(7):1059-64. doi: 10.1177/0192623316660769. Epub 2016 Jul 29
[PubMed PMID: 27474221]
Level 2 (mid-level) evidence
[23]
Hvid H, Thorup I, Oleksiewicz MB, Sjögren I, Jensen HE. An alternative method for preparation of tissue sections from the rat mammary gland. Experimental and toxicologic pathology : official journal of the Gesellschaft fur Toxikologische Pathologie. 2011 May:63(4):317-24. doi: 10.1016/j.etp.2010.02.005. Epub 2010 Mar 2
[PubMed PMID: 20199854]
[24]
Janowczyk A, Basavanhally A, Madabhushi A. Stain Normalization using Sparse AutoEncoders (StaNoSA): Application to digital pathology. Computerized medical imaging and graphics : the official journal of the Computerized Medical Imaging Society. 2017 Apr:57():50-61. doi: 10.1016/j.compmedimag.2016.05.003. Epub 2016 May 16
[PubMed PMID: 27373749]
[25]
Sun C, Wang B, Li J, Shangguan J, Figini M, Zhou K, Pan L, Ma Q, Zhang Z. Quantitative measurement of breast carcinoma fibrosis for the prediction in the risk of bone metastasis. American journal of translational research. 2018:10(6):1852-1859
[PubMed PMID: 30018725]
[26]
Zaha DC. Significance of immunohistochemistry in breast cancer. World journal of clinical oncology. 2014 Aug 10:5(3):382-92. doi: 10.5306/wjco.v5.i3.382. Epub
[PubMed PMID: 25114853]
[27]
Akram M, Iqbal M, Daniyal M, Khan AU. Awareness and current knowledge of breast cancer. Biological research. 2017 Oct 2:50(1):33. doi: 10.1186/s40659-017-0140-9. Epub 2017 Oct 2
[PubMed PMID: 28969709]
[28]
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2018 Nov:68(6):394-424. doi: 10.3322/caac.21492. Epub 2018 Sep 12
[PubMed PMID: 30207593]
[29]
Serdy KM, Leone JP, Dabbs DJ, Bhargava R. Male Breast Cancer. American journal of clinical pathology. 2017 Jan 1:147(1):110-119. doi: 10.1093/ajcp/aqw207. Epub
[PubMed PMID: 28171879]
[30]
Ferzoco RM, Ruddy KJ. The Epidemiology of Male Breast Cancer. Current oncology reports. 2016 Jan:18(1):1. doi: 10.1007/s11912-015-0487-4. Epub
[PubMed PMID: 26694922]
[31]
Weigelt B, Geyer FC, Reis-Filho JS. Histological types of breast cancer: how special are they? Molecular oncology. 2010 Jun:4(3):192-208. doi: 10.1016/j.molonc.2010.04.004. Epub 2010 Apr 18
[PubMed PMID: 20452298]
[32]
Azim HA Jr, Partridge AH. Biology of breast cancer in young women. Breast cancer research : BCR. 2014 Aug 27:16(4):427. doi: 10.1186/s13058-014-0427-5. Epub 2014 Aug 27
[PubMed PMID: 25436920]