Introduction
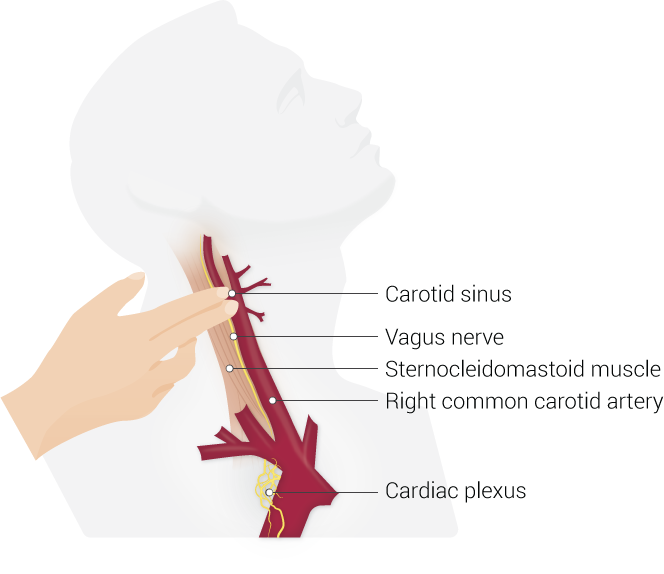
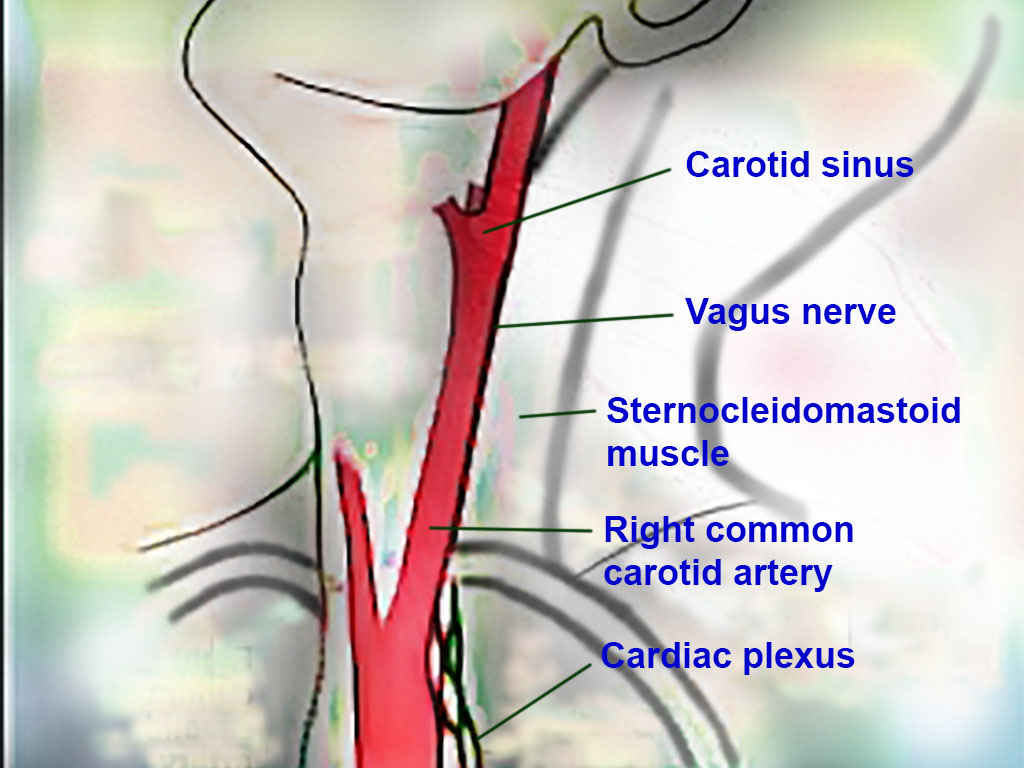
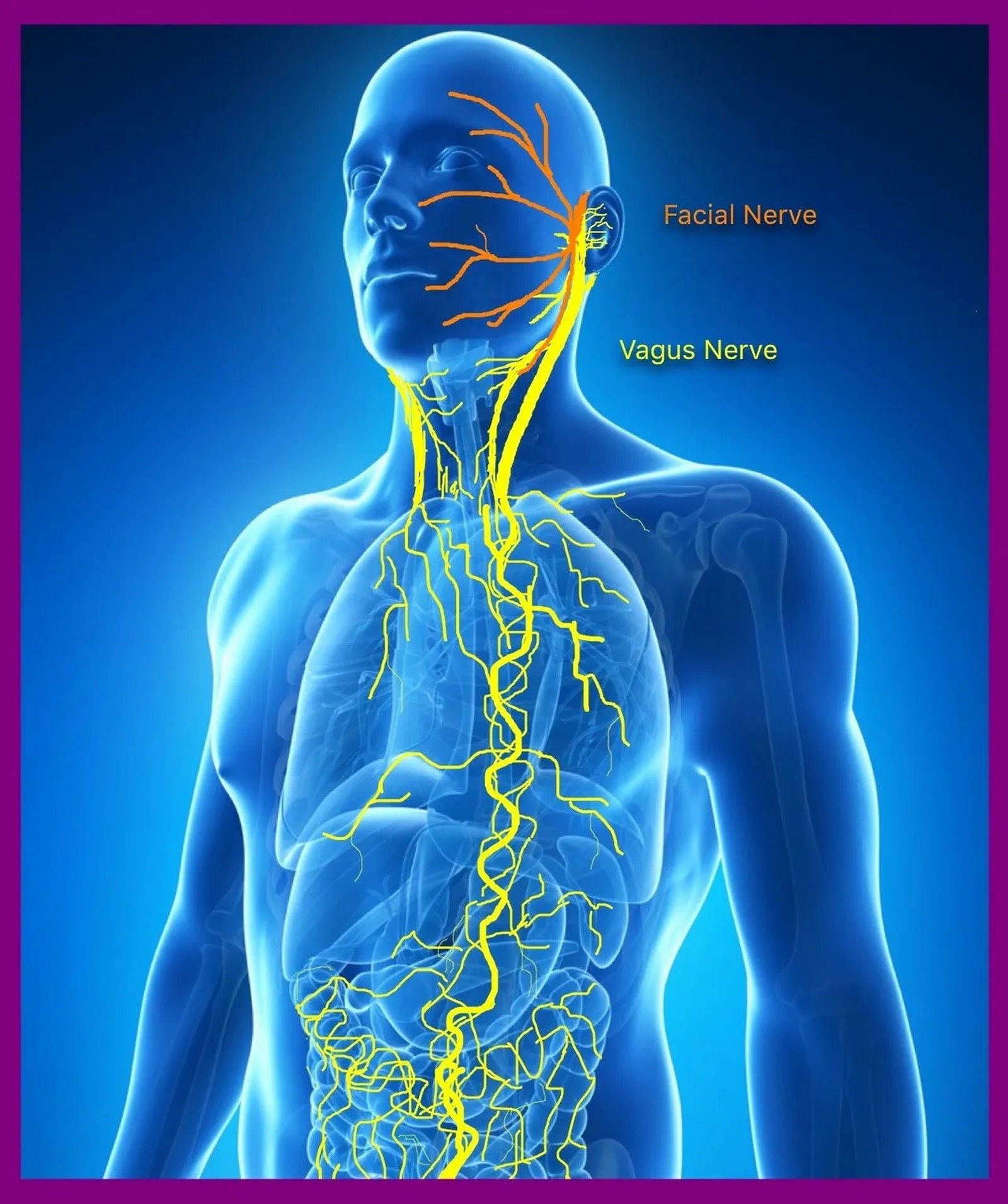
The vagus nerve (cranial nerve [CN] X) is the longest cranial nerve in the body, containing both motor and sensory functions in both the afferent and efferent regards. The nerve travels widely throughout the body affecting several organ systems and regions of the body, such as the tongue, pharynx, heart, and gastrointestinal system. Because of the wide distribution of the nerve throughout the body, there are several clinical correlations of the vagus nerve. See Image. Path of the Vagus Nerve.
Structure and Function
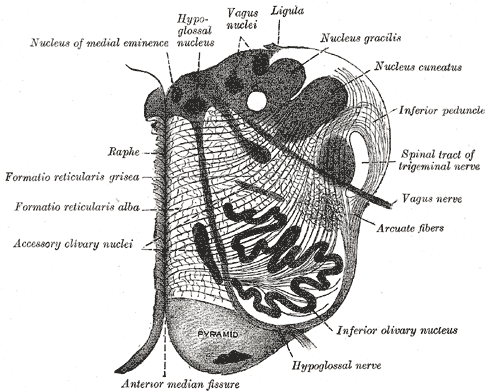
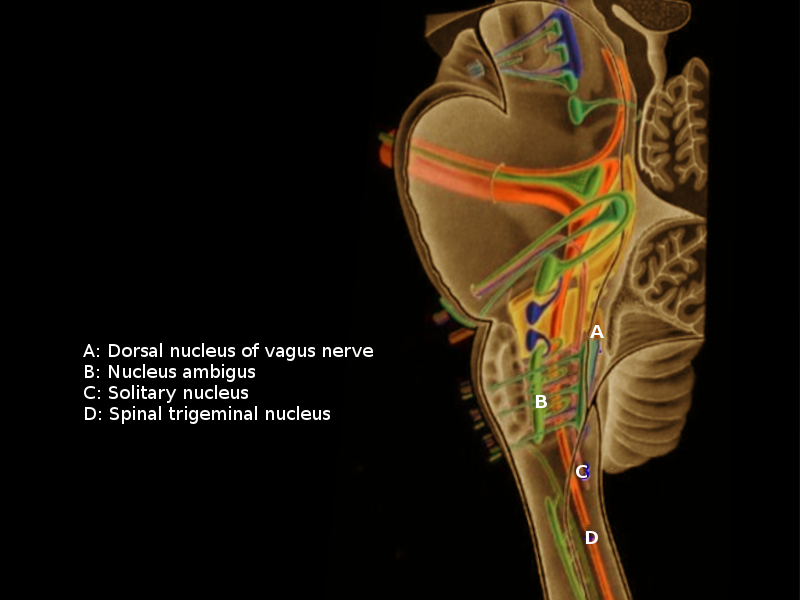
The vagus nerve has its origin in the medulla oblongata and exits the skull via the jugular foramen (see Image. The Hindbrain or Rhombencephalon). There are two ganglia on the vagus nerve (superior and inferior) as it exits the jugular foramen; the spinal accessory nerve (CN XI) joins the vagus nerve just distal to the inferior ganglion (see Image. Vagus nuclei).[1][2]
The origin of cell bodies for the vagus nerve originates from the nucleus ambiguous; the dorsal motor nucleus of X, superior ganglion of X, and the inferior ganglion of X. The nerve fibers from the nucleus ambiguous are efferent, special visceral (ESV) fibers which help to mediate swallowing and phonation. Fibers originating from the dorsal motor nucleus of X are efferent, general visceral (EGV) fibers which provide the involuntary muscle control of organs it innervates (cardiac, pulmonary, esophageal) and innervation to glands throughout the gastrointestinal tract. Superior ganglion of X provides afferent general somatic innervation to the external ear and tympanic membrane. The inferior ganglion of X provides afferent general visceral fibers to the carotid and aortic bodies; the efferent fibers of this nerve travel to the nucleus tractus solitarius; the inferior ganglion also provides taste sensation to the pharynx and relays this information to the nucleus tractus solitarius.[2][1][3][4][5]
The vagus nerve continues by traveling inferiorly within the carotid sheath where it is located posterior and lateral to the internal and common carotid arteries, and medial to the internal jugular vein (see Image. Carotid Sinus Massage). The right vagus nerve travels anteriorly to the subclavian artery and then posterior to the innominate artery; it makes its descent into the thoracic cavity by traveling to the right of the trachea, and posterior to the hilum on the right, moving medially to form the esophageal plexus with the left vagus nerve. The left vagus nerve travels anteriorly to the subclavian artery and enters the thoracic cavity wedged between the left common carotid and subclavian arteries; it then descends posteriorly to the phrenic nerve and posterior to the left lung, then travels medially towards to the esophagus forming the esophageal plexus with the right vagus nerve.[5][1][3][4]
There are four branches of the vagus nerve within the neck: pharyngeal branches, superior laryngeal nerve, recurrent laryngeal nerve, and the superior cardiac nerve (see Image. Neck Anatomy).[6]
The pharyngeal nerve branches arise from the inferior ganglion of CN X containing both sensory and motor fibers. These fibers form the pharyngeal plexus–branches of this plexus innervate the pharyngeal and palate muscles (except the tensor palatine muscle); the pharyngeal plexus also supplies the innervation to the intercarotid plexus which mediates information from the carotid body.[3][6]
The superior laryngeal nerve travels between the external and internal carotid arteries; the nerve divides into internal and external branches near the level of the hyoid. The internal laryngeal nerve goes through the thyrohyoid membrane entering the larynx. The external portion travels distally with the superior thyroid vessels. The external portion supplies the cricothyroid muscle, whereas the internal branch supplies the mucosa superior to the glottis.[6]
The right recurrent laryngeal nerve’s fibers branch from the vagus nerve near the right subclavian artery, traveling superiorly to enter the larynx between the cricopharyngeus muscle and the esophagus. The left recurrent laryngeal nerve then loops around the aortic arch distal to the ligamentum arteriosus and then enters the larynx. All of the laryngeal musculatures receives supply via the recurrent laryngeal nerve except for the cricothyroid muscle (supplied by the laryngeal nerve).[3][6]
While the vagus nerve is within the carotid sheath, it gives off the superior cardiac nerve and is associated with parasympathetic fibers and travels to the heart.[7][4]
The vagus nerve gives off anterior and posterior bronchial branches in which the anterior branches are along the anterior lung forming the anterior pulmonary plexus, whereas the posterior branches form the posterior pulmonary plexus.[3][6]
Esophageal branches of the vagus nerve are anterior and posterior and form the esophageal plexus. The left vagus is anterior to the esophagus; the right vagus is posterior.[3][6]
Gastric branches supply the stomach; celiac branches (mainly derived from the right vagus nerve) supply the pancreas, spleen, kidneys, adrenals, and small intestine.[3][1][8][4]
Embryology
The vagus nerve arises from the fourth branchial arch; this arch is also responsible for the development of the pharyngeal and laryngeal muscles, the laryngeal cartilages, the aortic arch, and subclavian artery.
Blood Supply and Lymphatics
The middle meningeal artery supplies the intracranial blood supply to the vagus nerve. The extracranial blood supply is from the common carotid artery, internal carotid artery, inferior thyroid artery, external carotid artery, a posterior meningeal artery, internal thoracic arteries, bronchial arteries, and esophageal arteries.[9][6]
The vagal system is involved in regulating the contraction of lymphatic (containing actin) cells.
Nerves
The vagus nerve has branches within the neck; these branches are the pharyngeal branches, superior laryngeal nerves, recurrent laryngeal nerves, and superior cardiac nerves. The structure and function of these nerves were described above.
Muscles
The vagus nerve has several fibers that innervate the striated muscles of the larynx and pharynx; there are two exceptions: the stylopharyngeus muscle (CNIX) and the tensor veli palatini muscle (V3).[3]
The vagus nerve innervates one muscle of the tongue: palatoglossus muscle–its function is to elevate the posterior portion of the tongue.[3]
The external branch of the superior laryngeal nerve supplies the cricothyroid muscle.[3]
The pharyngeal branches of the vagus supply: levator veli palatini, salpingopharyngeus, palatopharyngeus, and the uvula.[3]
Recurrent laryngeal nerves innervate the intrinsic muscles of the larynx, except the cricothyroid muscle (the external branch of the superior laryngeal nerve).[3]
Physiologic Variants
The recurrent laryngeal nerve has two branches prior to inserting into the larynx; the branching is typically inferior to the cricoid cartilage; however, there are instances when there are more than two branches, and thus are called esophageal branches.[10]
There are several variations of the non-recurrent vagus nerve.
Surgical Considerations
Consideration for the branches of the recurrent laryngeal nerve is critical during surgery of the thyroid gland. Because of the proximity of the thyroid gland and the branches of the recurrent laryngeal nerve, recommendations are for maintaining all nerves in this region unless there is a compromise of the nerve itself by malignancy.[4][6][11]
The recurrent laryngeal nerve may be damaged during a cervical esophagectomy, during the removal of a pharyngoesophageal diverticulum or a gastroesophageal anastomosis after performing the trans-hiatal esophagectomy. In the diverticulum excision and the anastomosis, the recurrent laryngeal nerve is lesioned from pressure applied by retractors in the operating room.[10][12][11]
Damage can be done to the external laryngeal nerve at the time of ligation of the superior thyroid artery during a thyroidectomy.[4][11]
Clinical Significance
The vagus nerve is commonly tested clinically in conjugation with the glossopharyngeal nerve because of their apparent effects that are oftentimes reliant upon another. A patient is often asked to open their mouth and say ‘ah,’ this should cause elevation of the uvula. If there is a lesion, the uvula shifts away from the paralyzed side. Gag reflex should not be used as a clinical exam as there can be a bilateral loss of the gag reflex in a healthy patient. If a patient is noted to have hoarseness during the physical exam, this should show the need to test the vocal cords in the patient; if there is hoarseness with a normal gag reflex and palatal elevation, this indicates a lesion of the recurrent laryngeal nerve.[3]
Vagus nerve stimulation was created as a means to reach a centrally located neurological structures by minimally invasive means. In the conventional vagus nerve stimulation technique, a device is implanted surgically under the skin in the chest, and electrical wires connect to the left vagus nerve (left used more often than right, as the right vagus nerve is more likely to have branches to the heart). Vagus nerve stimulation is approved to treat epilepsy and depression; however, with the wide distribution of the vagus nerve throughout the body, stimulation is being explored for other purposes such as the treatment of obesity.[13][4]
Stimulation of the larynx provides reflexes including cough, apnea, and effects on the cardiovascular system such as bradycardia and hypotension.
Central lesions of the vagus nerve can cause dysphagia, dysarthria and hoarseness; uvula deviation (towards the opposite side of the lesion); and transient parasympathetic effects.
Lateral medullary syndrome (posterior inferior cerebellar artery infarction) leads to the destruction of the glossopharyngeal and vagus nerves, the nucleus ambiguous, the solitary nucleus, and the spinocerebellar tracts.[14]
Other Issues
Mechanical alterations of the vagus nerve may be related to emotional problems (depression and anxiety) in patients with chronic obstructive airway disease and congestive heart failure. One of its dysfunctions could also be a source of pain in the same patient population.[15][16][17]