Continuing Education Activity
A knee dislocation is a potentially devastating injury and is often a surgical emergency. Knee dislocations frequently comprise ligamentous, bony, and neurovascular injuries that, when unrecognized, significantly increase the risk of amputation of the affected limb. Even dislocations that spontaneously reduce before evaluation by a healthcare professional carry the risk of significant neurovascular injury. Also, delayed diagnosis and management of knee dislocations increases the risk of long-term arthrofibrosis and joint instability. While most dislocated knees never fully return to their pre-injury state, timely and accurate diagnosis paired with prompt intervention can significantly improve outcomes for patients with this potentially complex orthopedic injury. This activity for healthcare professionals reviews the etiologic mechanisms of injury, epidemiology, evaluation, and management of knee dislocations and highlights the role of the interprofessional healthcare team in caring for patients with this traumatic joint disruption.
Objectives:
Identify patients with probable knee dislocation based on their clinical history and physical examination findings.
Select the most appropriate diagnostic studies when evaluating patients with knee dislocations for concomitant injuries.
Apply best practices when treating patients with a knee dislocation injury.
Develop and implement effective interprofessional team strategies to improve outcomes for patients with a knee dislocation injury.
Introduction
A knee dislocation can be defined as complete congruency loss between the distal femoral and proximal tibial articular surfaces. Bicruciate or multiligamentous injuries can also be categorized as knee dislocation due to the mechanism of injury.[1] A knee dislocation is a potentially devastating injury and is often a surgical emergency. This injury requires prompt identification, evaluation with appropriate imaging, and consultation with surgery for definitive treatment. Vascular injury and compartment syndrome are complications that the clinician should not miss in the workup of a knee dislocation.[2][3] This is in distinct contrast to patellar dislocations, which generally do not require immediate surgical or vascular intervention.[4][5]
Etiology
High-energy trauma is usually required to cause tibiofemoral dislocation at the knee joint. To disrupt this joint, Multiple concomitant ligamentous injuries and instability are also expected with disruption of the knee joint. Motor vehicle collisions, high-velocity sports-related injuries, and falls may all cause knee dislocation. Posterior and anterior dislocations occur most frequently; medial, lateral, and rotatory dislocations are also possible.
Epidemiology
Knee dislocations are infrequently encountered but are potentially limb-threatening injuries. Associated undiagnosed vascular injury can lead to prolonged limb ischemia, necessitating amputation.[6][7][8] Knee dislocations represent 0.001% to 0.013% of all orthopedic injuries.[9][10][11] However, their incidence is underreported, as almost 50% of knee dislocations spontaneously reduce at the scene, before arrival to the emergency department, or are misdiagnosed. Knee dislocations are more commonly reported in men than women, with a ratio of 4:1. Obesity is an independent risk factor for sustaining this injury from an ultra–low–energy mechanism of injury.
Pathophysiology
Anatomy
The knee is a ginglymoid joint with 3 articulations: the tibiofemoral, patellofemoral, and tibiofibular. Four major ligaments help to stabilize the knee joint: the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL). A knee dislocation can be associated with multiligamentous disruption. The normal range of motion (ROM) of the knee is 0 to 140 degrees, with 8 to 12 degrees of rotation during flexion and extension.
Mechanism of Injury
Knee dislocation can happen following high-energy injuries such as traffic accidents, dashboard injuries, falls from heights, and crush injuries. Low-energy injuries can also result in a knee dislocation, such as those encountered in athletic injuries or routine walking. Even ultra–low-energy injuries can result in a knee dislocation in patients with morbid obesity.
Associated Neurovascular Injuries
The popliteal artery is at the highest risk of a vascular insult due to a tibiofemoral dislocation. The popliteal artery stretches across the popliteal space and gives off several branches in a collateral system around the knee. Given its position in the popliteal space and the mechanism of knee dislocation, up to 40% of patients with a tibiofemoral disruption will sustain an associated vascular injury. These injuries are usually due to tethering at the popliteal fossa, proximally by the fibrous tunnel at the adductor hiatus, and distally by the fibrous tunnel at the soleus muscle. The collateral circulation formed by the geniculate arteries around the knee can provide vascular flow and palpable pulses that mask a limb-threatening vascular injury.[2] Peroneal nerve injuries occur in more than 20% of patients with knee dislocation due to the anatomic location of the peroneal nerve at the fibular neck.[2]
Associated Bony and Soft Tissue Injuries
Sixty percent of knee dislocations have associated fractures. Additionally, multiple soft tissue injuries can be associated with knee dislocation, such as patellar tendon rupture, periarticular avulsion, and displaced menisci.
History and Physical
Spontaneously Reduced Cases
Obtaining a thorough problem-oriented history is paramount when evaluating knee dislocations; this is particularly true in the 50% of knee dislocations that spontaneously reduce before contact with a clinician. Inquiries into the mechanism of injury and position of the lower leg immediately after the injury are imperative. When the patient or emergency management services report a change in the position of the tibia relative to the femur, the examiner should assume a knee dislocation occurred with subsequent return to normal anatomical position. The physical examination should include visualization of subtle signs of trauma, such as abrasions, bruising, ecchymosis, and effusion. Gross joint instability suggested by hyperextension of the knee > 30 degrees when lifting the heel strongly suggests a knee dislocation.
Cases Presenting With Notable Deformity
The diagnosis is more straightforward when a patient presents with an obvious deformity consistent with knee dislocation. A significant joint effusion, swelling, and ecchymosis may be present, limiting the examination of ligament integrity. Buttonholing of the medial femoral condyle through the medial capsule, known as a "dimple" or "pucker sign," may occur and indicates an irreducible posterolateral dislocation.[5] A closed reduction procedure is contraindicated in this scenario due to the risk of skin necrosis.
Physical Examination
All patients with a history suggestive of a knee dislocation require a comprehensive physical examination of the affected extremity. Particular attention should be paid to the neurovascular stability of the extremity and ligamentous stability of the joint.
Distal and popliteal pulses should be assessed and compared with the contralateral side. Excluding a vascular injury is prioritized before and after reduction; serial examinations are necessary. A palpable distal pulse does not exclude vascular injury. Limb-threatening vascular ischemia can result in the presence of palpable distal foot pulses, as collateral circulation can mask a complete popliteal artery injury.[12]
The ankle-brachial index (ABI) should be measured in all patients suspected of knee dislocation.[13] When the ABI exceeds 0.9, patients should be monitored with serial examinations. An ABI of less than 0.9 necessitates further investigation with an arterial duplex ultrasonography or computed tomography angiography. Vascular surgical consultation is imperative if arterial injury is confirmed.
Patients with absent or diminished pulses should undergo immediate joint reduction, followed by reassessment. If the pulses remain undetectable or diminished, surgical exploration should ensue. Ischemia of greater than 6 hours has been reported to be associated with amputation rates of up to 86%. If the pulses return following joint reduction, ABI measurements should be taken, followed by observation and serial examination or angiography.
Neurological deficits can occur concomitantly with vascular injuries. Sensory and motor function should be assessed and documented, although limitations by pain and swelling are common. The ligamentous integrity of the 4 major knee stabilizers should also be evaluated.
Evaluation
Ankle-Brachial Index
The ankle-brachial index (ABI) is the ratio of lower extremity perfusion via the posterior tibial and dorsalis pedis arteries and upper extremity perfusion via the brachial artery. An ABI of 0.9 or greater is considered normal, whereas an ABI of less than 0.9 can indicate a vascular compromise.[13] While pulse and perfusion examinations may be conducted, they are of limited utility unless there are hard signs of vascular compromise; in this case, prompt evaluation by vascular surgery is necessary. Normal pulses or ABIs do not necessarily rule out any injury; reports exist of popliteal artery contusion, intimal layer disruption, and delayed thrombus formation in patients with distal perfusion after knee dislocation.
Duplex Ultrasonography
If readily available, duplex ultrasonography can evaluate the vasculature at the bedside. However, imaging with computed tomography angiography should be pursued in cases of asymmetric pulses, decreased ABI, or abnormal duplex ultrasonography. Absent or weak pulses, pale or cool extremities, paresthesias, or paralysis mandate emergent vascular surgery consultation.[14]
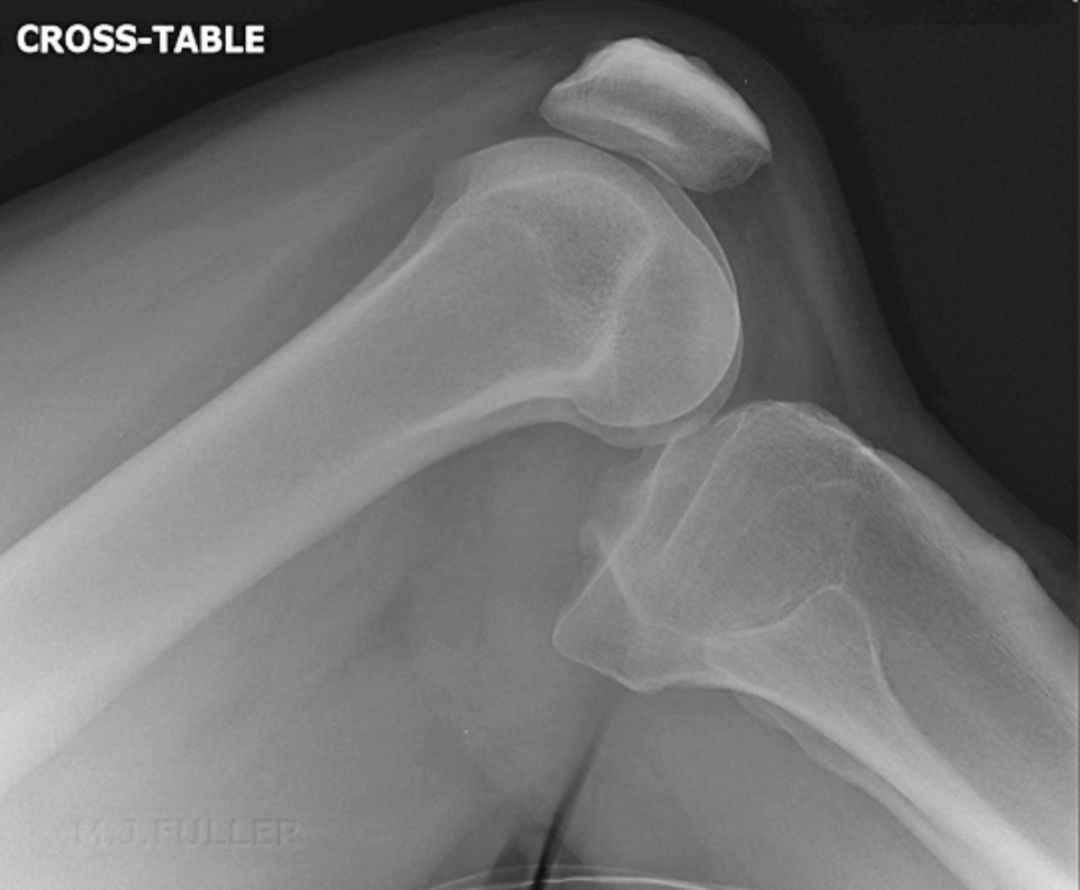
Imaging Studies
Anteroposterior and lateral knee radiographs can confirm the reduction of the joint and any concomitant fractures. A 45-degree oblique radiograph is optional, especially in associated fracture cases. Radiographs can be normal in cases of spontaneously reduced knee dislocations. Radiographic findings in knee dislocation include joint space asymmetry or irregularity, associated avulsion fractures such as Segond sign or lateral tibial condyle avulsion fracture, or osteochondral fractures or defects.
Computed tomography (CT) is indicated when fractures are identified in postreduction radiographs. CT better delineates fracture patterns and the level of extension, such as in tibial eminence, tibial tubercle, or tibial plateau fractures. Magnetic resonance imaging (MRI) may be indicated to assess soft tissue structures and assist surgical planning. MRI is best performed after acute reduction and before hardware placement to obtain better-quality images.[15]
Treatment / Management
Nonoperative Management
Knee dislocation is an orthopedic emergency requiring acute closed reduction followed by evaluation of the vascular status.[1][16] Hospital admission for serial vascular examinations is an option solely for patients with clearly strong distal pulses, normal ABI, and normal duplex ultrasonography. Otherwise, emergent vascular surgery consultation and CT angiography should be pursued to rule out popliteal artery injury. The technique for a closed reduction following an anterior dislocation is axial traction and anterior translation of the femur; for a posterior reduction, it is anterior translation of the tibia. In medial, lateral, or rotatory dislocations, the technique comprises axial traction and manipulation opposite to the present deformity. After closed reduction, the knee should be splinted with 20 to 30 degrees of flexion.
Operative Management
Surgical immobilization can be the definitive treatment following a successful acute closed reduction absent vascular injury. Nonoperative management as a definitive treatment bears inferior outcomes. However, prolonged immobilization can be complicated by an unstable knee with a restricted range of motion.[17]
Open reduction
An open reduction is indicated in knee dislocations recalcitrant to closed reduction or delayed presentations.[18] Other indications for open reduction include posterolateral dislocation and open fracture–dislocation. Obesity poses a challenge to the closed reduction of dislocated knees, but an open reduction could be an alternative option. Additionally, open reduction is indicated with associated vascular injury.
Open reduction is performed via a midline incision with a medial parapatellar approach. If the medial femoral condyle is buttonholed through the medial capsule, the condyle must be reduced and the medial capsule repaired. Concomitant soft tissue injuries, such as meniscal tears, periarticular ligament avulsions, or patellar tendon rupture, may benefit from an acute repair. Concomitant bony injuries can be managed with acute internal fixation or spanning via external fixation followed by planned delayed definitive management. External fixation is also indicated following vascular repair and in cases complicated by obesity. Other indications for external fixation include open fracture–dislocation, compartment syndrome, and polytrauma.[19]
Early ligament repair or reconstruction
Arthroscopic management may not be an option for early ligament repair or reconstruction, especially in cases of large capsular injury, due to the risk of fluid extravasation and compartment syndrome. Open reconstruction would be indicated for the posterolateral and posteromedial corners, including the collaterals, as they are subcutaneous and close to the neurovascular structures. Intra-articular injuries, such as meniscal, cartilaginous, and capsular injuries, can also be addressed acutely. Unstable knees should be managed with ligament repair or reconstruction. Surgery within 3 weeks of the injury offers improved outcomes.[20] Patients should be in a knee immobilizer until definitive management of the ligamentous injuries. Acute and staged reconstructive procedures have equivalent outcomes.
Differential Diagnosis
The differential diagnosis for knee dislocation includes:
- Anterior cruciate ligament injury
- Femoral shaft fractures
- Knee fracture management in emergency medicine
- Medial collateral ligament injury
- Meniscus injuries
- Patellar injury and dislocation
- Patellofemoral joint syndromes
- Tibia and fibula fractures in the emergency department.
Staging
There are 2 commonly used classification systems for knee dislocation: the Kennedy Classification, which mainly relies on the direction of tibia displacement, and the Schenck Classification, which considers concomitant knee ligament injuries.
Kennedy Classification
Anterior dislocation: this is due to a hyperextension injury. This is the most common knee dislocation pattern and accounts for 30% to 50% of dislocation injuries. Anterior dislocations have the highest rate of peroneal nerve injury and usually involve a PCL injury. When concomitant vascular injury is present, it is usually an arterial intimal tear from traction.
Posterior dislocation: this is the second most common knee dislocation pattern, comprising 30% to 40% of knee dislocations, and is caused by axial loading to a flexed knee, as in a dashboard injury. Posterior dislocation has the highest rate of vascular injury, most commonly characterized by a complete popliteal artery tear.
Lateral dislocation: the mechanism of injury in lateral knee dislocations is either varus or valgus force, usually with concomitant ACL and PCL injury. Lateral dislocations comprise approximately 13% of knee dislocation injuries.
Medial dislocation: as with lateral dislocations, the mechanism of injury is either varus or valgus force, and both the PLC and PCL are usually injured. Medial dislocations are uncommon and account for only 3% of dislocations.
Rotational or rotary dislocation: this is usually an irreducible dislocation pattern and posterolateral dislocation is most common, with buttonholing of the femoral condyle through the capsule.[21]
Schenck Classification
KD I: Multiligamentous injury with involvement of either the ACL or PCL.
KD II: Injury to 2 ligaments: the ACL and PCL only.
KD III: Injury to 3 ligaments: the ACL and PCL, in addition to either the PMC or PLC.
KD IIIM: Involves the ACL, PCL, and MCL
KD IIIL: Involves the ACL, PCL, and LCL.
KD IV: Injury to 4 ligaments, including the ACL, PCL, PMC, and PLC. KD IV injuries have the highest rate of concomitant vascular injury (5% to 15%).
KD V: A multiligamentous injury with a periarticular fracture.[22]
Prognosis
Knee dislocation is a serious injury in which the knee rarely returns to its preinjury state and the need for surgical intervention is common.
Complications
Complications are a common denominator in traumatic knee dislocations and vary in incidence. The most common dislocation complication is arthrofibrosis, and the most serious is vascular injury. Other commonly encountered complications following traumatic knee dislocation include but are not limited to injuries to the peroneal nerve and nearby vascular structures.
Arthrofibrosis or stiffness is the most common complication of knee dislocation, occurring in up to 38% of the patients. Delayed immobilization of the affected joint is a reported risk factor for arthrofibrosis; early mobilization is encouraged as a preventative measure. Manipulation under anesthesia and arthroscopic lysis of adhesion are the available management options.
Some degree of instability is experienced in up to 37% of knee dislocation cases. However, redislocation is uncommon. Management varies from bracing to revision reconstruction.
Peroneal nerve injuries in knee dislocations occur in 10% to 40% of patients, with partial recovery reported in up to 50% of those affected.[23] Men, patients with obesity, and cases with associated fibular fractures are at an increased risk for peroneal nerve injuries. Management of the injuries employs an ankle-foot-orthosis (AFO) to prevent equinus contracture. In acute injuries, the injury can be managed by neurolysis or exploration of the nerve at the time of the reconstruction. In chronic cases, management includes nerve repair, reconstruction, or tendon transfer. A dynamic tendon transfer requires transferring the tibialis posterior tendon to the foot.
Vascular injuries are reported in 5% to 15% of all knee dislocations; nearly 50% of all vascular injuries occur with anterior or posterior dislocations.[24] KD IV dislocations have the highest rate of vascular injuries. Vascular injuries should be managed with emergent vascular repair and prophylactic fasciotomies.
Postoperative and Rehabilitation Care
Rehabilitation after traumatic knee dislocation is highly physically demanding. Although there are no definitive protocols, the rehabilitative principles are the same. A delay of 1 to 3 weeks between the injury and operative management permits the inflammatory reaction to subside; straight leg raise exercises should be performed to avoid quadriceps muscle wasting.[25] The goal of early postoperative rehabilitation is the protection of the operative repair, especially if the PCL was reconstructed. Hence, some protocols recommend the use of a limited extension brace.[26][27][28] Delayed postoperative rehabilitation is patient-, injury-, and repair-specific.
Deterrence and Patient Education
The immediate treatment after a knee dislocation involves splinting, bracing, or surgery. Rehabilitation requires exercises to restore strength, flexibility, and function; its importance cannot be overstated.[29] Weight-bearing restrictions and activity modifications must be thoroughly explained, including the use of crutches, braces, or other assistive devices during the recovery period.
Increased pain, swelling, or sensory changes of the affected extremity may be indicative of neurovascular complications. Patients must be educated regarding the signs and symptoms of these complications and instructed on how and when to seek care. Additionally, the importance of commitment to rehabilitation and ongoing care must be stressed. Patients with traumatic knee dislocations may benefit from connecting with support networks, seeking counseling, or joining a rehabilitation group.
Pearls and Other Issues
A palpable distal pulse is an inadequate indicator of normal vascular function following a knee dislocation. Further evaluation is mandatory to exclude popliteal arterial insult; any sign of vascular compromise mandates emergent vascular surgery consultation. A delay in the diagnosis of popliteal artery injury may result in irreversible injury and ischemia, requiring above-knee amputation. Generally, any ischemia persisting for more than 8 hours will necessitate amputation. Delayed thrombosis is also possible and may not be present during the initial evaluation.
Other injuries the clinician may encounter following knee dislocation include peroneal nerve injuries, which can cause foot drop. Compartment syndrome and deep venous thrombosis are other possible complications. Associated fractures and ligamentous injuries should receive treatment as per orthopedic surgery recommendations.
Enhancing Healthcare Team Outcomes
Knee dislocation is a relatively common injury seen in the emergency department. Because the dislocation can be associated with a neurovascular injury that can lead to the loss of a limb, patients with a knee dislocation are best served by an interprofessional team. The first-responder and triage staff must be fully aware that a dislocated knee can disrupt the vascular supply to the distal leg; immediate admission and consultation with an emergency department physician are necessary. A vascular surgery consult is required if there is a loss of pulses in the leg, and a radiologist may be consulted to image the blood supply. Orthopedic consultation is also necessary in almost all cases.
The outcomes are good for most patients with knee dislocations who obtain prompt management. A chronically unstable and painful knee is common when diagnosis and treatment are delayed.[30][31] All patients will require some degree of physical rehabilitation following a knee dislocation injury.