Continuing Education Activity
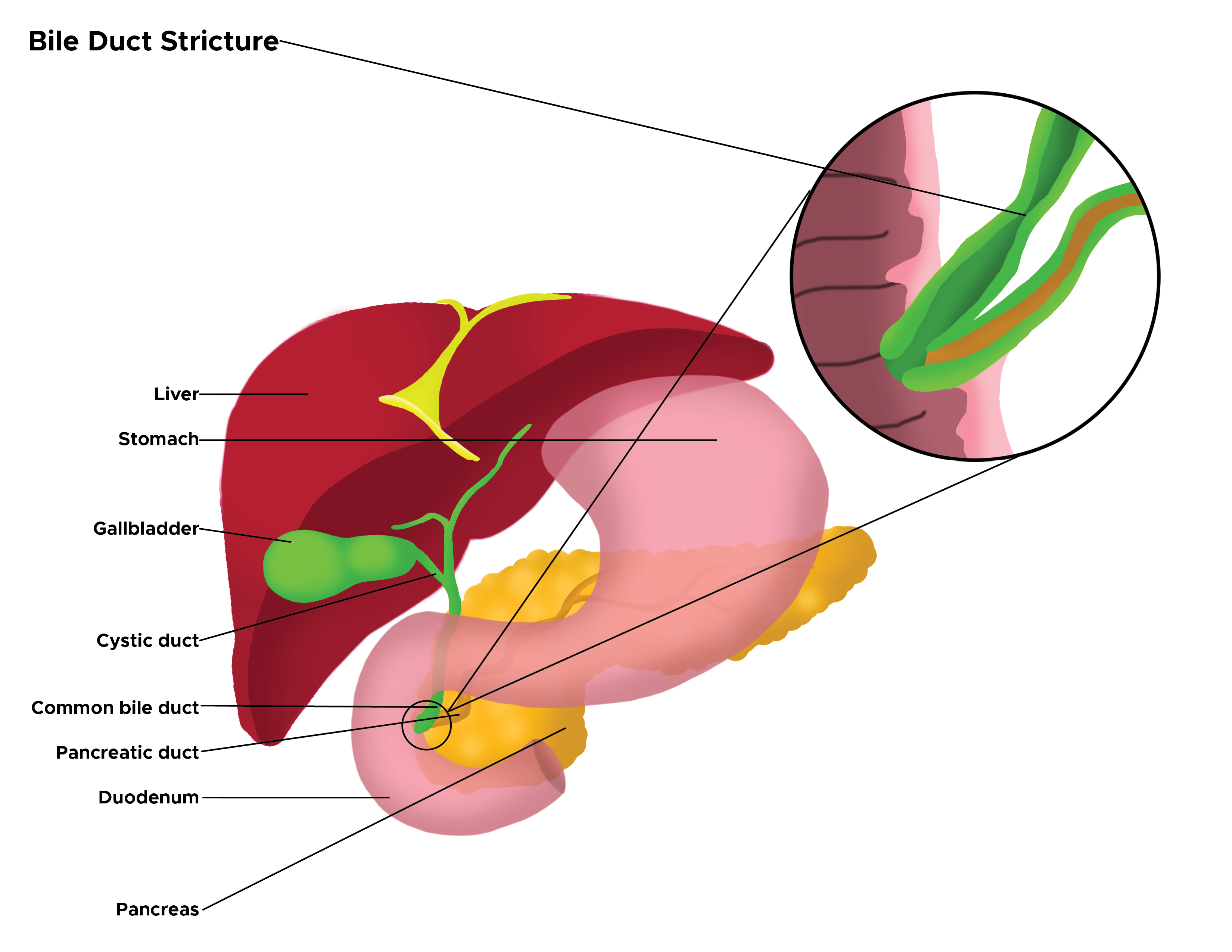
Bile duct strictures are segments of the narrowing of the intrahepatic or extrahepatic biliary ductal system. The narrowing impedes the normal antegrade flow of bile, causing proximal dilatation resulting in significant morbidity from the clinical and pathological sequelae of biliary obstruction. The management of these strictures depends on the etiology, which could be benign or malignant. This activity reviews the evaluation and management of bile duct strictures and highlights the role of the interprofessional team in evaluating and treating patients with this condition.
Objectives:
- Describe the etiology of bile duct strictures.
- Outline the presentation of a patient with bile duct strictures.
- Summarize the management considerations for patients with bile duct strictures.
- Explain the importance of improving care coordination among the interprofessional team to enhance the delivery of care for patients with bile duct strictures.
Introduction
Biliary strictures or bile duct strictures refer to segments of narrowing of the intrahepatic or extrahepatic biliary ductal system. When narrowed, they impede the normal antegrade flow of bile, causing proximal dilatation resulting in clinical and pathological sequelae of biliary obstruction. Patients with chronic biliary strictures present a unique challenge when malignancy is suspected. The diagnosis and management of patients with biliary strictures potentially encompass an interprofessional approach, including endoscopists, surgeons, interventional radiologists, and hepatobiliary specialists.[1][2][3]
Etiology
Bile duct strictures can be congenital or acquired.[4] The latter is more common than congenital strictures. Acquired strictures are further classified as either benign or malignant.[5] There is a wide range of benign acquired conditions causing bile duct strictures and contributing to 30% of biliary strictures.[6] This includes iatrogenic strictures, which comprise the majority of benign biliary strictures. Misidentification of the biliary duct for cystic duct during laparoscopic cholecystectomy leads to bile duct injury, which may be partial or complete. The long-term sequelae of these injuries lead to the formation of benign biliary strictures.[7] The incidence of injury may be decreased by obtaining an intraoperative cholangiogram, especially in cases of gangrenous cholecystitis or empyema of the gallbladder.[8][9] Understanding the anatomy of the blood supply to the bile duct is of paramount importance with regard to the repair of the bile duct.[10] Similarly, anastomotic biliary strictures are a known complication after orthotopic liver transplantation.[11] Anastomotic strictures are also known to occur after a Whipple procedure (incidence of 4%), performed for pancreatic mass or trauma. This is especially true for small-caliber thin-walled ducts.[1] Though relatively rare, strictures can also result from infections, like tuberculosis.[12] Other benign causes are listed below:
- Chronic pancreatitis
- Primary sclerosing cholangitis
- Acute cholangitis
- Blunt and penetrating abdominal trauma
- Autoimmune diseases (pancreatitis or cholangitis)
- Mirizzi syndrome
- Ischemic cholangiopathy
- Biliary inflammatory pseudotumors
- Oriental cholangiohepatitis (Ascaris lumbricoides and Clonorchis sinensis)
- Post radiation
However, the most common etiology for biliary strictures is malignancies.[13] Both pancreatic head cancer and cholangiocarcinoma are attributed to the majority of malignant biliary strictures. Others include periampullary cancer, gallbladder carcinoma, hepatocellular carcinoma, lymphoma, and metastasis to regional solid organs and lymph nodes.[6][14][6][15]
Epidemiology
Globally, the incidence of biliary strictures is thought to be on the rise primarily because of the iatrogenic bile duct injuries resulting from the widespread practice of laparoscopic cholecystectomy. Multiple strategies like the critical view of safety have been suggested to minimize bile duct injuries and associated morbidity from bile leaks and strictures.[16] The estimated rate of biliary injuries is about 0.7% after laparoscopic cholecystectomy. Most of these injuries are minor injuries or bile leaks. Biliary strictures are rare in the pediatric age group.[17] There is no published difference in incidence or prevalence of biliary strictures in males as compared to females though some risk factors like alcoholic chronic pancreatitis are commoner in males.
Pathophysiology
Biliary strictures are characterized by narrowing of a segment of the bile duct associated with proximal ductal dilatation. Obstruction of bile flow leads to elevation of serum bilirubin levels with clinical and laboratory features of obstructive jaundice. Stasis of bile is a major risk factor for ascending cholangitis.[18]
As observed from magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP), benign strictures have tapered margins with smooth and symmetric borders. On the other hand, malignant strictures have shouldering of the margins with irregular and asymmetric borders.[11] Malignant strictures involve a long segment as opposed to benign, which involves shorter segments. Malignant strictures appear to enhance on contrast-enhanced cross-sectional imaging.[18]
The strictures can be classified according to the Strasberg-Bismuth classification. Classification helps in guiding management.[18][19][20]
Type E injuries lead to strictures of the hepatic ducts, which are further defined by the proximal extent.
- E1: Common hepatic duct division greater than 2 cm from the bifurcation.
- E2: Common hepatic duct division less than 2 cm from the bifurcation.
- E3: Common bile duct division at the bifurcation.
- E4: Hilar stricture involves confluence and loss of communication between the right and left hepatic duct.
- E5: Involves aberrant right hepatic duct with concomitant stricture of the common hepatic duct.[14]
Histopathology
In general, histopathological findings in biliary strictures depend on the etiological agent or mechanism. For example, in the case of primary sclerosing cholangitis, histopathology reveals intrahepatic or extrahepatic bile duct inflammation and fibro-obliteration.[5] In the assessment of biliary strictures, histological appraisal with cytology or histopathology is primarily required to rule out malignancy.[18] However, if imaging has confirmed or has high suspicion for malignancy, a positive histological diagnosis is not mandatory preoperatively.
History and Physical
The clinical presentation depends on the location and cause of the stricture.[11] Biliary strictures can be clearly asymptomatic with non-contributory findings on physical examination. Nevertheless, a section of patients with biliary strictures will present with features of obstructive jaundice, which include yellowing of mucosal surfaces and skin, pruritus, pale stools, steatorrhoea, and dark urine.[19] These may be accompanied by constitutional symptoms, such as weight loss, fever, nausea, vomiting, and malaise. Patients may present with an acute abdomen secondary to cholangitis or hepatic abscess, which can result as a complication of the bile duct stricture.[21]
History of fever and leukocytosis suggests an infective cause or sequelae to the strictures. History of weight loss, abdominal or back pain, worsening performance status should be taken with caution since it could warn towards a possible malignant etiology.[15]
The previous history of hepatobiliary surgery, autoimmune disease, pancreatitis, cholelithiasis, or chemotherapy should be elicited as it can be pivotal in determining or eliminating the differential diagnosis.[11]
Further efforts should be made during the physical examination to elicit specific clinical signs like Murphy and Courvoisier signs, as this may also help in narrowing down the diagnosis or etiology of jaundice. The presence of hard masses in the abdomen may point towards an advanced malignant process.
Evaluation
Contributory laboratory findings are mainly drawn from a liver function test, a coagulation profile, and a complete blood count. Liver function tests may reveal elevated levels of conjugated bilirubin and liver enzymes (alkaline phosphatase and gamma-glutamyl transferase). Transaminases may be elevated nonspecifically. Immunological studies may be obtained to assess certain autoimmune etiologies of biliary strictures. Apt diagnosis and further management are based on the correlation of laboratory data, imaging findings with epidemiologic and clinical data.[11]
Deranged liver function tests and coagulation profiles may help to determine the algorithm of subsequent imaging and minimally invasive studies.[15][22] Likewise, when present, certain immunological markers help in accurate diagnosis and management. For example, IgG4 associated sclerosing cholangitis presents as hilar or distal common bile duct (CBD) strictures that are associated with autoimmune pancreatitis (IgG4 related). Both these disease entities are responsive to steroid therapy.[6][11] Antinuclear antibody and rheumatoid arthritis factor may help in support of this diagnosis.
Assay of CA19-9 and carcinoembryonic antigen (CEA) can be obtained in patients with suspected hepatobiliary malignancy as they can help with diagnosis and follow-up. Of note, these are not specific to biliary malignancy. Endoscopic ultrasound (EUS) guided fine needle aspiration cytology (FNAC) is highly sensitive and specific but not useful to rule out malignancy.[6]
Ductal dilatation is a major feature of imaging for biliary strictures.[1] Imaging of suspected biliary strictures can begin with a trans-abdominal ultrasound, which detects biliary dilatation and is highly sensitive for the detection of biliary obstruction and the level of obstruction. It has a low yield for the detection of strictures, though. Malignant biliary strictures are more likely to cause severe ductal dilation as compared to benign biliary strictures.[6][11] Endoscopic ultrasound has high sensitivity and accuracy for malignant lesions and has been used as the imaging test of choice in the assessment of distal biliary obstruction.
Computed tomography (CT) scan has higher sensitivity than trans-abdominal ultrasound for biliary malignancy, and its utility can be improved with the use of a multi-detector CT (MDCT) scan and CT-pancreatic protocol in providing more information on tumor vascular encroachment and biliary tree obstruction. It is also able to detect complications from biliary obstruction such as cholangitis and abscesses.[1]
MRCP can provide high-quality cholangiograms, thus establishing the location and extent of biliary strictures. It provides a cross-sectional and three-dimensional reconstruction of the biliary tree.[5] It helps guide endoscopic therapy, especially if ERCP is contraindicated. MRCP also does not have ionizing radiation, thus making it a superior option over a MDCT scan. Its sensitivity and specificity (which can be improved by the use of diffusion-weighted imaging, DWI) are however comparable to that of ERCP.[1][5]
Evaluation of biliary strictures by ERCP can determine etiology, provide tissue samples for cytology and histology, and facilitate therapeutic interventions like stenting of obstructed segments from strictures. It is, however, associated with post-ERCP pancreatitis and is also being overtaken by newer technologies like confocal laser endomicroscopy (CLE). Other emerging technologies useful in the assessment of the etiology of biliary strictures include fluorescent in-situ hybridization (FISH), direct peroral cholangioscopy, and intraductal ultrasound.[5][13][23]
A hepatobiliary iminodiacetic acid (HIDA) scan helps to identify the level of bile leaks and bile injuries after cholecystectomy.[14]
Treatment / Management
Medical management of biliary strictures is largely restricted to addressing complications from biliary obstructions and sometimes treatment of the causative agent. Therefore, analgesics, empiric antibiotics, plus hemodynamic support with intravenous fluids with or without vasopressors and inotropes are often instituted where applicable.[24] Also common are therapies aimed at reducing the effects of increasing bilirubinemia. These efforts are often supportive and in preparation for definitive therapy.[25] Other forms of medical treatment could be aimed at the prevention of further complications like excessive bleeding due to a coagulopathy as well as deep vein thrombosis and sepsis in the early postoperative period.
The goal of the interventions for biliary strictures includes reestablishing patency and avoiding additional procedures.[11][19] There are varying options for operative or interventional management. These options can be accomplished via endoscopy, open surgery, or percutaneously. The etiology and the location of the stricture, as well as the patient’s hemodynamic stability and nutritional status, could determine the timing and type of intervention required.[25] The Bismuth classification can further guide the most appropriate approach since it offers a guide to the determination of the level at which healthy biliary tissue is available for repair and anastomosis.[11] Likewise, the Strasberg classification system, which incorporates the presence of a bile leak and lateral injuries into consideration, can also be useful in some cases in making the choice of the best intervention.[19] Additionally, preoperative determination of malignancy is pivotal in the planning of treatment and avoiding undue exploratory surgery.
In general endoscopic treatment is the first-line treatment of biliary strictures.[26] The treatment of biliary strictures includes options shown below
Common Interventions for Biliary Strictures
Dilatation
- The preferred approach for the management of benign biliary stricture[11]
- Balloon dilatation used extensively for strictures resulting from primary sclerosing cholangitis[5]
- Commonly performed endoscopically
- Tracts resulting from percutaneous transhepatic biliary drainage can be used for access during dilatation[27]
Stenting
- Commonly performed endoscopically
- Useful in the management of both benign and malignant common bile duct (CBD) strictures[2]
- Used to reduce hyperbilirubinemia or cholangitis in patients before definitive surgery[22]
- Useful for palliation in inoperable malignant strictures
Resection and Anastomosis
- The decision depends on whether it’s a malignant or benign stricture and whether the desired outcome is palliative or curative[25]
- Associated with significant morbidity and cost[6]
Bypass
- Hepaticojejunostomy may make it difficult in the future to perform ERCP[25]
- Bypass may involve choledochoduodenostomy in certain cases
Image-guided percutaneous transhepatic biliary drainage catheter may be placed for palliation of hyperbilirubinemia in patients with either inoperable disease or until completion of neoadjuvant therapy.
A biliary sphincterotomy involves the division of the biliary sphincter of Oddi and the intraduodenal segment of the common bile duct. It enables removal of stones, placement of stents, and assists endoscopic access for future ERCP. It also facilitates balloon dilatation.[18]
Novel techniques for the management of biliary strictures include magnetic compression anastomosis (MCA), intraductal radiofrequency ablation, and biodegradable stents.[18] Others include large bore catheterization, cutting-balloon dilation, and placement of retrievable covered stents.[19] The magnetic compression anastomosis has specifically been used for biliary recanalization with favorable results.[3]
Differential Diagnosis
In the diagnosis and management of biliary strictures, the most valuable and critical distinction that should be made is between benign and malignant etiology. This differentiation presents a major diagnostic and therapeutic challenge. Therefore, elaborate history taking, physical examination, and diagnostic workup should be completed.[13] The addition of other techniques like fluorescence in situ hybridization (FISH), Kras/p53 mutation analysis, intraductal biopsies, and confocal laser endomicroscopy (CLE) may be considered to improve the diagnostic yield.[6]
A diagnosis of choledocholithiasis should also be considered in cases of suspected biliary strictures.
Prognosis
The mortality in patients with biliary structures depends on the underlying etiology. Biliary strictures due to chronic pancreatitis, trauma, radiation, or operative injury have a good prognosis, but those resulting from malignant and primary sclerosing cholangitis may have unfavorable prognosis as well as strictures arising in patients with HIV cholangiopathy.
Complications
Biliary strictures can get complicated by chronic low-grade biliary obstruction. The complications include:[11]
- Recurrent cholangitis
- Ascending cholangitis
- Gram-negative septicemia
- Stone formation
- Hepatic abscesses
- Secondary biliary cirrhosis
- End-stage liver disease
- Cholangiocarcinoma
Other complications could result from interventional procedures, and these may include:[26]
- Pancreatitis
- Cholangitis
- Bleeding
- Biliary perforation
- Additionally, there are reports of distal migration of biliary stents leading to duodenal perforation.[2] Stents can also be complicated by ingrowth or overgrowth by the tumor, rendering them non-functional.
Consultations
Biliary strictures frequently present a challenge in terms of diagnosis, necessitating interdisciplinary collaboration. Likewise, a significant proportion of patients with benign strictures may have a protracted, complicated course calling for multiple consultations. Therefore, teams caring for patients with biliary strictures may comprise:[15]
- Hepatobiliary surgeons
- Medical oncologists
- Diagnostic radiologists
- Surgical oncologists
- Endoscopists
- Gastroenterologists
- Interventional radiologists
Deterrence and Patient Education
Patients drinking alcohol should be counseled against the practice, especially those whose diagnosis is linked to drinking i.e alcoholic chronic pancreatitis. Patients who have biliary stents placed should be educated about the recognition of symptoms and signs of blocked stents. Those who have external drains should be taught about how to flush their drains using aseptic measures. Lastly, the patient and their caregivers should be informed about the prognosis of their disease.
Enhancing Healthcare Team Outcomes
Bile duct strictures may present with nonspecific signs and symptoms of obstructive jaundice, abdominal pain, nausea, vomiting, fever, and leukocytosis. The cause of bile duct strictures may be one of the myriads of diagnosis, which includes benign and malignant etiologies. The complexity of this disease process lies in the challenges of its diagnosis and subsequent appropriate management. Inaccurate diagnosis or delay in management can have devastating outcomes for the patient. While the general surgeon is almost always involved in the care of these patients, it may become imperative to consult with an interprofessional team of specialists that include gastroenterologists, interventional radiologists, hepatobiliary surgeons, surgical oncologists, and transplant surgeons.
The society of American gastrointestinal and endoscopic surgeons (SAGES) offers guidelines for the clinical application of laparoscopic biliary tract surgery. Regarding common bile duct injuries, the guidelines suggest that the factors which have been associated with bile duct injury include surgeon experience, patient age, male sex, and acute cholecystitis. (Level II, Grade C) If major bile duct injuries occur, outcomes are improved by early recognition and immediate referral to experienced hepatobiliary specialists for further treatment before any repair is attempted by the primary surgeon unless the primary surgeon has significant experience in biliary reconstruction. (Level II, Grade A)
Nurses play a vital role during the recovery of such patients. They monitor the patient closely for changes in vital signs and mental status as the patients recuperate. The nurses help in the timely recognition of common postoperative complications such as deep vein thrombosis and anastomotic leaks. The role of the laboratory personnel and pharmacist is critical as well. The pharmacist may be involved in the management of parenteral nutrition for critically ill patients.